How Long COVID Shortness of Breath Lasts | Cognitive FX
While recovering from COVID-19, you may find yourself getting breathless easily from activities that didn’t used to tire you, like carrying laundry or walking up the stairs.

If you’ve been feeling fuzzy-headed and have been struggling to concentrate since you’ve had COVID-19, you’re not alone. Even months after the disease, some patients still can’t shake the feeling that their brain is lost in a maze. Many describe it as walking through a fog, unable to see where they’re going.
Brain fog is not a medical term, but the name pops up frequently in medical literature to refer to cognitive difficulties that patients with various conditions sometimes experience, including those with chronic fatigue syndrome, cancer patients experiencing side effects from chemotherapy, brain injury patients, and women who are either pregnant or transitioning into menopause.
And now, there’s one more condition to add to the list: Long COVID. Some patients live with this symptom for months after contracting the coronavirus, and it inevitably affects their ability to carry out daily activities and results in a lower quality of life.
Brain fog is not a new symptom for our treatment team. At Cognitive FX, we’re used to hearing patients with a mild traumatic brain injury describe the same problems. In fact, we’ve had a few patients who have completed our treatment both for a concussion and Long COVID, and they say the brain fog feels exactly the same for both conditions.
Other Long COVID patients, however, may express that “brain fog” doesn’t entirely fit their experience. This contrast underlies the need for objective testing of brain dynamics, as symptoms are unique to each individual. It’s still too early to say for sure, but based on our initial research, both post-concussion syndrome and Long COVID affect the brain in a similar manner.
Because we see the same type of brain dysfunction in Long COVID patients and post-concussion syndrome (PCS) patients, we’ve adapted our treatment for post-concussion syndrome to help patients suffering from Long COVID. The treatment process includes a few adjustments to ensure we can cover COVID patients’ (who may also call themselves “Long Haulers”) specific needs. You can read more about our treatment later in the article.
In this article, we cover:
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.

For most patients, COVID-19 infections are mild or even asymptomatic, and whatever symptoms are present completely resolve within a few weeks. A considerable number of patients, however, struggle to fully recover from this infectious disease. They experience a wide range of symptoms for much longer than expected, especially if they only had a mild case of COVID-19 in the first place.
This is such a new condition that, up until now, there was no formal definition. Using the term “post-COVID-19 condition”, the World Health Organization (WHO) announced its official definition of what constitutes Long COVID. According to this organization, Long COVID “occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually three months from the onset of COVID-19, with symptoms that last for at least two months and cannot be explained by an alternative diagnosis.” (In this blog we will continue to use Long COVID as a synonym for this condition.)
Reports of Long COVID started appearing quite early in the pandemic. Initial values were alarming, with more than 70% of patients who had been hospitalized with a severe COVID infection still reporting symptoms months after the initial infection. Among those who stayed at home, initial studies suggested lower values, with around 30% of patients reporting at least one symptom nine months later.
However, more recent research suggests Long COVID may be much less common than previously believed. In April 2021, the UK Office for National Statistics put the proportion at about one patient in every seven developing Long COVID, but the latest analysis in August, which looked at more than 50,000 people, suggested it’s roughly one in 30 patients who have symptoms lasting at least three months.

One of the most common neurological symptoms reported by Long COVID patients is "brain fog," with some studies suggesting that as many as 80% of patients experience ongoing issues with memory and fuzzy thinking.
Some patients describe how the fog makes them feel numb, as if an impenetrable haze blocks access to their thoughts. It can affect memory, visual and spatial skills, executive function, and the ability to process information. When these essential brain functions don’t work properly, it becomes difficult to understand, focus, and even remember simple things. Basically, when brain fog happens, your brain doesn’t serve you as well as you would expect.
We’ve all experienced it at some point in our lives. Maybe you were jetlagged and your thinking was lethargic because it felt like 3 a.m. Or perhaps you took some medication that made you fuzzy for a few hours. Whatever the cause, you just had to wait for your brain to go back to normal.
For many COVID-19 long haulers, however, this fog is permanent and much more serious. Typical complaints include memory problems, difficulty retaining information, trouble finding the right words, and a general feeling of being overwhelmed by the smallest task. These patients didn’t actually experience anything during their COVID-19 infection that could explain this cognitive dysfunction, like a stroke or a seizure. Yet, they’re coming out with a cognitive impairment that can seriously impact their quality of life.
That’s often in addition to other ongoing symptoms like fatigue, breathing issues, poor sleep quality, and more.
One of the ways researchers believe COVID-19 causes brain fog is via an inflammatory response in the body that quickly escalates to neuroinflammation in the brain. A study found increased levels of inflammatory cytokines localized in the brain for weeks after COVID-19 infection. In simple terms, cytokines are molecules produced by the immune system that are involved in fighting infections. However, an excessive and uncontrolled inflammatory reaction in the brain interferes with communication between nerve cells and may contribute to brain fog.
A second explanation involves restricted blood flow to the brain as a result of general hypoxia due to breathing problems. In fact, one of the first imaging-based studies of neurological injury in COVID-19 patients found the same metabolic disturbances in both the brains of Long COVID patients and those who had suffered oxygen deprivation.
This restricted blood flow to the brain disrupts the connection between nerve cells and the blood vessels that supply them — known as neurovascular coupling (NVC) — and hinders the distribution of oxygen and energy to the areas of the brain that need it. This is known as neurovascular coupling dysfunction, and it’s one of the leading causes of lingering symptoms — like COVID-19 brain fog — after the virus is gone. It’s also one of the main mechanisms behind lingering symptoms from traumatic brain injury (TBI).
A third possible cause involves dysfunction of the autonomic nervous system (ANS), which is another overlap between Long COVID and TBIs. In a healthy person, the ANS regularly sends messages from the brain to the heart, bowel, stomach, and other organs to either speed them up or slow them down, depending on what’s needed. This is done with the help of the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which have opposing roles. The SNS, which is considered the “fight or flight” system, is characterized by quick responses mobilizing the body for action, while the PNS is the “rest and digest” part, which controls how the body slows down and returns to normal.
However, in Long COVID patients, the sympathetic nervous system is often overactive, making it harder to regulate how the body adapts to each situation. For example, a study showed that long-haulers had a lower SNS response when they had to suddenly plunge their hands in icy water compared to healthy individuals, but SNS activity remained high when patients were resting (as opposed to returning to normal quickly, as it should).
Finally, some patients may develop brain fog indirectly as a consequence of other symptoms also caused by Long COVID, like vision problems.
Eye specialists are starting to notice that many patients who have seemingly recovered from COVID-19 are now beginning to develop eye-related complications. While some patients experience symptoms like blurry vision and conjunctivitis while they are still ill with the virus, the impact of COVID-19 on vision seems to last a lot longer.
For example, one of the conditions that plagues Long COVID patients is retinopathy, where the blood supply to the retina is blocked, or at least restricted, causing blurred vision. This, in turn, causes brain fatigue for these patients, which may end up revealing itself as brain fog, fatigue, feelings of overwhelm, and more.

Although Long COVID and traumatic brain injuries both trigger neurovascular coupling disruption and ANS dysfunction, the mechanism behind these changes is slightly different.
For this reason, we believe Long COVID patients need a modified approach to treatment, with a particular focus on the respiratory and cardiovascular systems, both of which are usually affected by COVID. We’ve adapted the assessment and treatment we offer our long haulers to make sure we cover what these patients need. This is still work in progress and we continue to make small adjustments as we gather more data.
At Cognitive FX, assessment starts with a functional Neurocognitive Imaging (fNCI) scan to detect the areas of the brain that were affected by the injury. The scan spots which regions are still operating normally and which are either under or over-activated. Patients also complete a detailed interview to assess previous health history and the progression of symptoms. We also explain what they should expect from treatment.
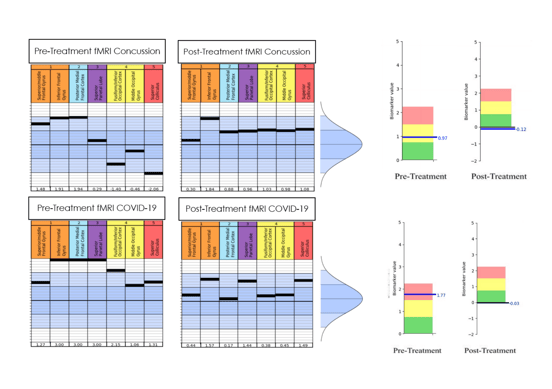 Brain scan results pre- and post-treatment for a patient who was seen separately for post-concussion syndrome and Long COVID. Overall scores (shown on the right) improved to healthy ranges with treatment.
Brain scan results pre- and post-treatment for a patient who was seen separately for post-concussion syndrome and Long COVID. Overall scores (shown on the right) improved to healthy ranges with treatment.
Armed with the results of the scan and the patient interview, we customize a treatment plan to target the specific areas of the brain that were highlighted as dysfunctional by the scan. This typically involves multiple therapies, such as vision therapy, occupational therapy, cognitive therapy, neuromuscular therapy, sensorimotor therapy, and psychotherapy, which are included in our treatment called Enhanced Performance in Cognition (EPIC) Treatment. Treatment is overseen by a clinical neuropsychologist, clinical neuroscientist, neurosurgeon, a host of therapists in multiple disciplines, and more.
To counteract the sympathetic nervous system dominance described earlier, we offer Long COVID patients extra cardio sessions combined with breathing exercises to encourage the parasympathetic system to become active. These exercises are meant to retrain the brain, allowing both SNS and PNS to respond to what the body needs.

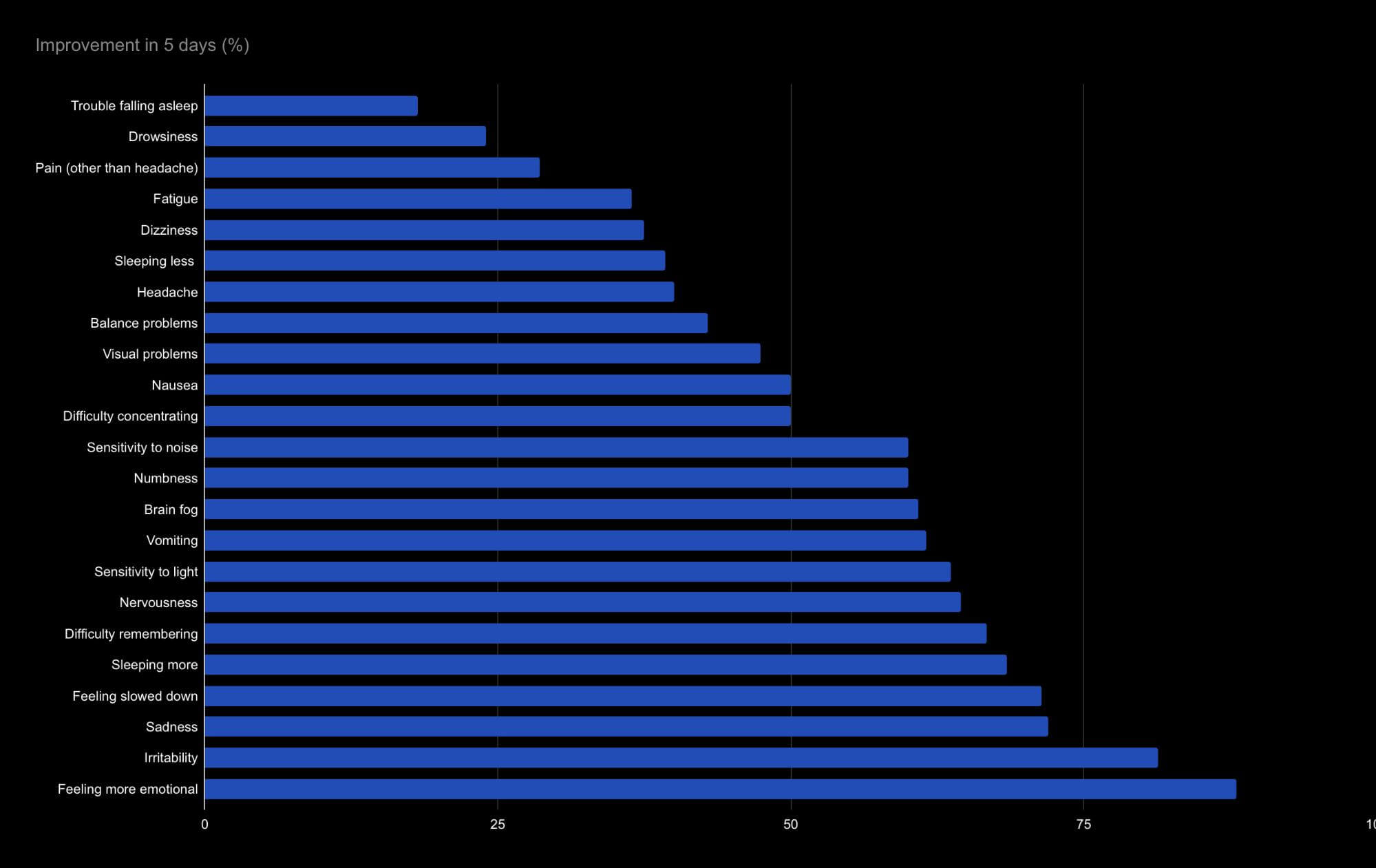
On the last day of treatment, patients undergo a second scan to see how much their brain changed. Average improvement on the second brain scan is currently 112%. Self-reported symptom improvements after one week vary widely, from an almost 90% improvement in emotional symptoms to less than 20% improvement in falling asleep.
On average, long haulers saw their symptoms reduced by half after a week of treatment. Neurological and cognitive symptoms, such as sadness and difficulty remembering, seem to improve more quickly than physical symptoms, such as drowsiness and headaches. However, we’ve only treated 17 patients and we need more data to draw any significant conclusions.
In terms of brain fog, patients experienced a 60% improvement, which is likely to significantly impact their quality of life, allowing for more clear thinking and better memory.
Our sister clinic, Neural Effects, has also successfully treated patients with COVID-19, but their treatment is designed to be more immediate, typically between 4 and 12 weeks after the initial infection, when patients still have symptoms. Treatment includes breathing exercises combined with physical and cognitive therapy, which helped these patients achieve a full recovery.
To discuss your specific symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.

Life with Long COVID can be challenging, but there are some things you can do at home to help your recovery:
Practice breathing exercises
We cannot overstate the importance of practicing breathing exercises during recovery. We’ve seen patients go through cognitive therapy and simply forget to breathe because they’re concentrating on something else. Practicing diaphragmatic breathing can help decrease pain, muscle tension, and other physical and cognitive deficits. If you practice this type of breathing at home on a regular basis, you will feel the benefits in your daily life.
Follow good sleep patterns
One bad night is not going to have a major impact, but recurrent sleep deprivation can make your brain fog worse. Aim for at least eight hours of sleep every night, but you may find that you need more to feel better. You can find some more tips about how to train your brain to sleep after brain damage here.
Eat a brain-friendly diet
Not eating a balanced diet can make it difficult for your brain to focus. Diets rich in sugar, saturated fats, or high in calories are harmful for neural function because they increase levels of oxidative stress and hinder cognitive functions.
In contrast, certain foods are rich in nutrients that can actually help your brain operate smoothly. These include, for example, omega-3 fatty acids, which are essential to support nerve cell function and can play a role in maintaining brain health throughout your life.
Pick healthy options rich in omega-3 fatty acids to include in your diet, such as fish, beans, and nuts, and avoid caffeine, alcohol, and processed foods. You can learn more about nutrition for an injured brain here.
Play brain games
The phrase “use it or lose it” really does apply to your brain. Find the time to play brain games, ideally with a memory element. If you don’t like games, try learning a new skill. As long as it’s an enjoyable process and not stressful, it can give your brain a much-needed boost while you recover from the effects of COVID-19. Here are 17 cognitive exercises you can try.
Keep moving
If you have other symptoms alongside brain fog, you may find it hard to be active. However, even gentle exercise can help your recovery. If you can’t go for a run, then go for a walk, but try to move regularly.
Pace yourself
If you find that everyday tasks leave you breathless, tired, and even “foggier” than you started, don’t try to achieve them all at the same time. Instead, break these activities into smaller chunks to do as and when you can. Make sure you take frequent breaks before you become exhausted.
Stay motivated
Think about what you would like to do and set small, achievable goals to get there. Some days will be better than others, but don’t feel discouraged. Always celebrate your successes, no matter how small.
Connect with your friends and family
Whether it’s in person, by phone or email, don’t lose touch with friends and family. Connecting with other people can make you feel better and keep your brain engaged.
See a Mental Health Professional
If you have any severe mood symptoms, we may recommend seeing a cognitive behavioral therapist in addition to other treatment approaches. You can read more about how this therapy helps after a brain injury here.

What are the most common symptoms of Long COVID?
The most common symptoms of Long Covid include shortness of breath, fatigue, and sleep disorders, but researchers have identified over 200 possible symptoms. They found that Long COVID-19 symptoms can affect virtually any organ in the body.
Some symptoms reported by people with Long COVID include:
Who gets Long COVID?
This isn't easy to assess as doctors only recently started recording Long COVID as an official diagnosis.
However, some research suggests Long COVID becomes more likely with age and is twice as common in women and patients with pre-existing conditions. Estimates put 1% to 2% of people in their 20s developing Long COVID, compared with 5% of people in their 60s.
Does the COVID-19 Vaccine Help Prevent Long COVID?
The short answer is yes.
UK researchers looked at data from over 900,000 people who received both doses of the vaccine and found that their risk of developing Long COVID was reduced by half if they actually caught COVID-19. Most common symptoms were similar to those experienced by unvaccinated adults — including loss of smell, cough, headaches, and fatigue — but symptoms in vaccinated adults were milder, and there were fewer hospitalizations.
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.

Dr. Jaycie Loewen is a Clinical Neuroscientist who received her Doctorate of Neuroscience at the University of Utah. Her background includes the study of basic and clinical brain injury, including the publication of research regarding mechanisms of epilepsy pathophysiology. Her work has elucidated the role of glial and neuronal cell profiles in viral-induced brain injury and acute seizures. Dr. Loewen is further a Howard Hughes Medical Institute Scholar, with a Master's in Clinical Investigation awarded in 2018, as well as a recipient of the Higher Education Teaching Specialist Certificate. Through these degrees, she obtained experience with patient care and education as well as an understanding of the necessity of respecting patient experience and symptoms. Dr. Loewen’s focus is firstly patient care and education. She also provides literature analysis and aids in the publication of Cognitive FX’s research. Her goal is to improve Cognitive Fx’s ability to help patients through equal interaction and communication, as well as the furthering of concussion and mild traumatic brain injury treatment and science.

While recovering from COVID-19, you may find yourself getting breathless easily from activities that didn’t used to tire you, like carrying laundry or walking up the stairs.

Most patients with COVID-19 recover within a few days or weeks after a brief acute infection. However,about 10%experience long-term symptoms such as brain fog, fatigue, headaches, shortness of...