Stop guessing - see your injury, target your treatment. Get your life back.
One week with us can give you your life back. We don't guess about your injury; our advanced brain imaging allows us to see the problem and build a personalized intensive plan to fix it. Most of our patients feel they are at the end of the road, but 77% recover after treatment. Find out in 5 minutes if we can help you recover.
Pre-Treatment Brain FunctionPost-Treatment
Pretreatment vs
Post Treatment
Patient Severity Index Score (SIS)
- 0-0.8 (Healthy Brain)
- 0.8-1.5 (Borderline)
- 1.5+ (Injured Brain)
See Your Brain. Understand Your Injury.
Our functional NeuroCognitive Imaging (fNCI) scan reveals exactly how your brain is functioning compared to healthy individuals, guiding a personalized treatment plan.
Severity Index Cumulative Score (SICS)
Your fNCI scan measures brain function using z-scores, which show how far your results deviate from healthy individuals. A z-score of 0 means average function. Scores between -1 and +1 are considered within normal range. Scores beyond ±2 indicate significant deviation that may be causing your symptoms.
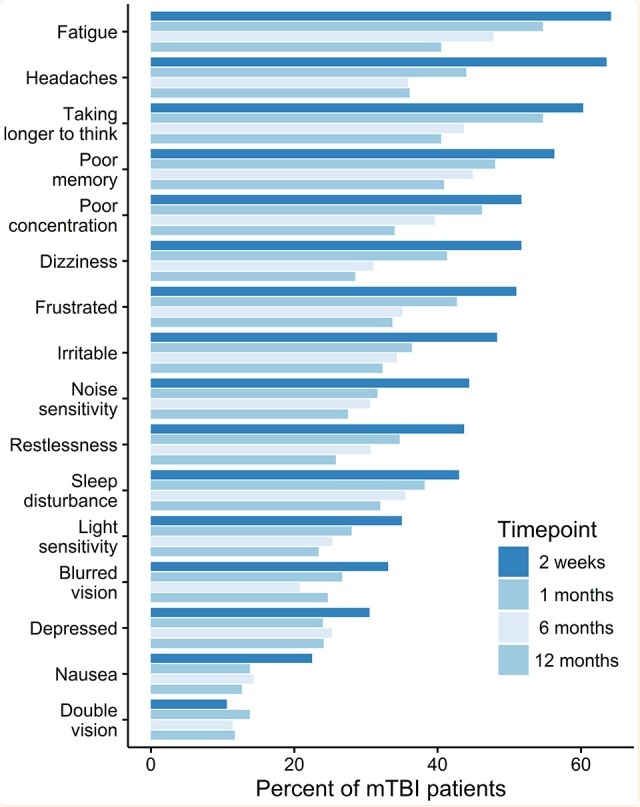
Why You Feel This Way
Your symptoms aren't "in your head." They're measurable, biological responses to specific brain regions working incorrectly. Here's the connection between what you experience and what your scan reveals.
Your visual processing regions are working 3x harder than normal to interpret what you see. This metabolic overdrive can create inflammation and pressure, triggering headaches that radiate from behind the eyes.
Your brain is flooding the language comprehension zone with excess blood flow. Simple tasks drain your cognitive battery because less efficient brain regions are doing the work of efficient ones.
The brain region responsible for reasoning, planning, and sustained attention is dysregulated. Your attention system can't filter all the other hyperactivity going on.
Your thalamus is your brain's sensory gateway that should "dim the lights" at night. When it's hyperactive, sensory signals keep firing instead of quieting down.
This region controls your reward/punishment response and impulse regulation. When it's overworking, minor frustrations register as major threats. Your brain's emotional thermostat is miscalibrated.
Brain Region Analysis
Executive Function
9 regionsAttention
10 regionsLanguage
9 regionsVisual Processing
16 regionsSubcortical
10 regionsMemory
10 regionsYour Personalized Treatment Plan
Based on the scan findings, our multi-disciplinary team creates a customized EPIC treatment protocol targeting your specific areas of dysfunction.
Physical Therapist
Movement, balance, and motor control rehabilitation
Proprioceptive Neuromuscular Facilitation (PNF) Stretching
Utilize PNF patterns (e.g., D1/D2 flexion/extension) for the upper and lower extremities to reduce spasticity and improve motor pathway efficiency.
Targets the hyperactive Left Precentral Gyrus. The combination of passive stretching and isometric contractions helps reset the neural drive to muscles, reducing the motor tension associated with hyperactivation.
Balance Training on Unstable Surfaces
Have the patient perform static and dynamic balance exercises (e.g., single-leg stance, tandem walking) on foam pads or balance boards.
Targets the hyperactive Precuneus and Postcentral Gyrus. This challenges the proprioceptive and visual systems, forcing more efficient processing and integration to maintain stability, thereby calming overactive networks.
Gait Training with Rhythmic Auditory Stimulation (RAS)
Use a metronome or rhythmic music to cue walking pace, focusing on heel-toe pattern, stride length, and arm swing.
Targets the hyperactive Basal Ganglia and Left Precentral Gyrus. External rhythmic cueing offloads the over-activated internal timing mechanisms of the Basal Ganglia, promoting a smoother, more automatic motor pattern.
Speech-Language Pathologist
Language processing and communication rehabilitation
Auditory Comprehension Desensitization
Present short, simple spoken sentences in a quiet environment, gradually increasing complexity and introducing minimal background noise.
Targets the hyperactive Left Temporal Lobe Language Cluster. This rebuilds comprehension skills from the ground up and helps the brain adapt to auditory input without becoming overwhelmed.
Semantic Feature Analysis (SFA)
For word-finding difficulties, guide the patient to describe an object's features (category, function, appearance) to activate related semantic networks.
Targets the hyperactive Left Inferior and Middle Temporal Gyri. SFA provides a structured approach to access lexical information, bypassing the inefficient, over-activated pathways and building stronger, alternative neural routes.
Paced Auditory Input
Use a text-to-speech program or therapist-led reading to present information at a slowed, deliberate pace, allowing for adequate processing time.
Targets the hyperactive Left Superior Temporal Gyrus. Slowing down the rate of auditory input prevents the hyperactive language processing centers from being overloaded, improving comprehension.
Occupational Therapist
Daily function and cognitive task management
Energy Conservation and Work Simplification
Teach the patient to break down complex tasks (e.g., cooking, cleaning) into smaller, manageable steps with built-in rest periods.
Targets the hyperactive Right Superior Frontal Gyrus and Left Precentral Gyrus. This strategy reduces the cognitive load required for planning and mitigates the physical fatigue caused by inefficient motor control.
Sensory Diet Implementation
Create a daily schedule of sensory activities (e.g., using a weighted blanket, listening to calming music, tactile play) to help regulate arousal levels.
Targets the hyperactive Cingulate Gyrus and Postcentral Gyrus. A sensory diet provides structured input to help modulate the brain's alertness and attention systems, preventing sensory overload.
Vision Therapist
Visual processing and eye movement rehabilitation
Saccadic Eye Movement Training
Have the patient practice rapidly shifting their gaze between two fixed targets (e.g., dots on a wall) horizontally, vertically, and diagonally.
Targets the hyperactive Frontal Eye Fields (within the Frontal Gyri) and Cuneus. This trains more efficient and controlled eye movements, reducing the neural effort required for visual scanning.
Brock String Exercise
Use a string with colored beads to train convergence and divergence, having the patient focus on each bead to perceive a single bead with two strings forming an 'X'.
Targets the hyperactive Fusiform and Lingual Gyri. This provides powerful feedback on binocular vision, helping to stabilize visual input and reduce the processing strain on hyperactive visual association areas.
Psychologist
Emotional regulation and cognitive behavioral support
Cognitive Behavioral Therapy (CBT) for Emotional Regulation
Help the patient identify triggers for emotional outbursts, recognize distorted thoughts, and develop coping strategies to manage impulsivity.
Targets the hyperactive Right Lateral Orbitofrontal Gyrus. CBT provides top-down cognitive control strategies to modulate the bottom-up emotional dysregulation driven by this region.
Mindfulness-Based Stress Reduction (MBSR)
Teach formal meditation practices (e.g., body scan, mindful breathing) to cultivate non-judgmental awareness of thoughts and emotions.
Targets the hyperactive Cingulate and Orbitofrontal Gyri. MBSR strengthens the brain's capacity for attentional control and reduces the reactivity of emotional circuits, calming these over-activated areas.
Massage Therapist
Physical tension release and nervous system regulation
Myofascial Release for Neck and Shoulders
Apply slow, sustained pressure to the fascial tissues of the cervical spine, shoulders, and upper back to release chronic tension.
Targets the hyperactive Left Precentral Gyrus. Releasing physical tension in the upper body can reduce the afferent (sensory) signals contributing to the over-activation of the motor cortex.
Swedish Massage with Slow, Rhythmic Strokes
Employ long, gliding strokes (effleurage) and gentle kneading (petrissage) to promote systemic relaxation.
Targets the hyperactive Cingulate and Orbitofrontal Gyri. The predictable, rhythmic input helps down-regulate the sympathetic nervous system, calming the brain's over-active emotional and attentional centers.
Ready to See Your Brain?
Take the first step toward understanding and treating your brain injury with our advanced fNCI technology.
Schedule Your ConsultationClinically Proven Results
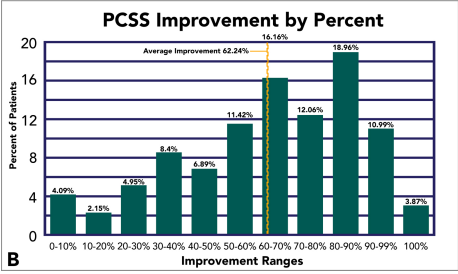
62% Reduction in Symptoms after
1 Week.
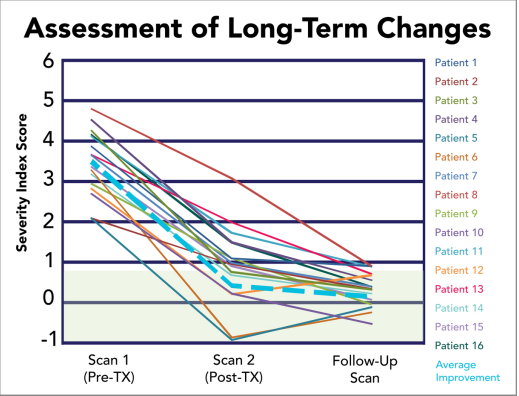
The improvements from treatment are long lasting.
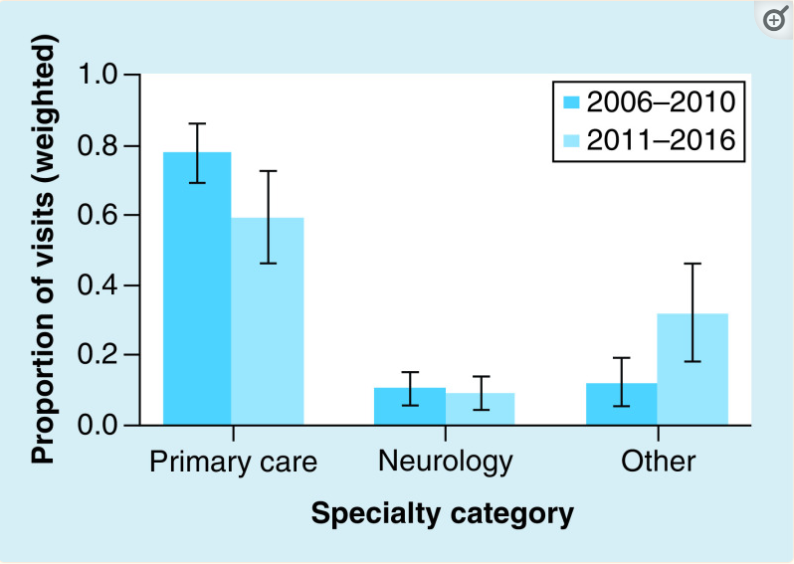
87% of Patients have seen three different types of doctors and have not recovered before CFX.
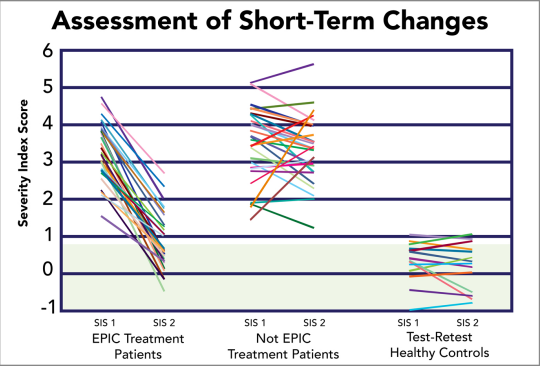
Treatment patients improve; untreated patients' brains remain the same.
Symptoms Patients Report Before Treatment
Patient Stories
Personalized Scan Guided Treatment
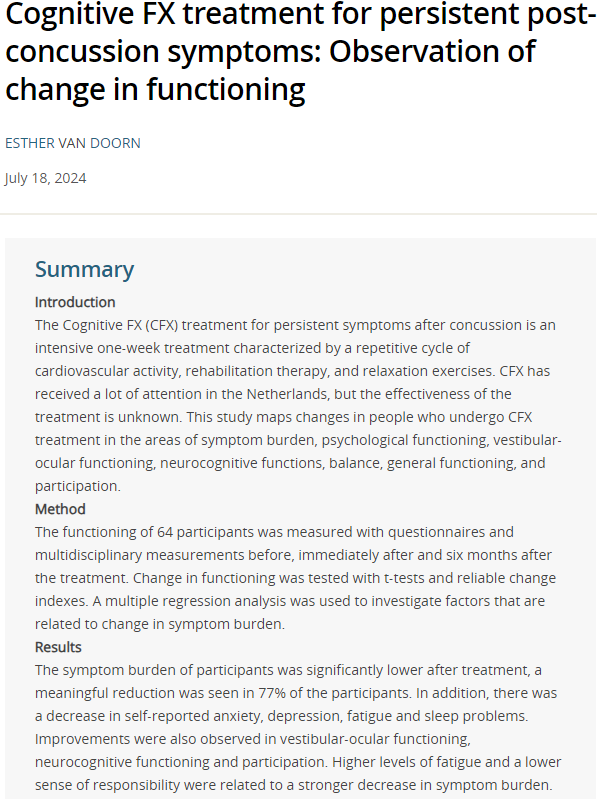
6 Month Treatment Results
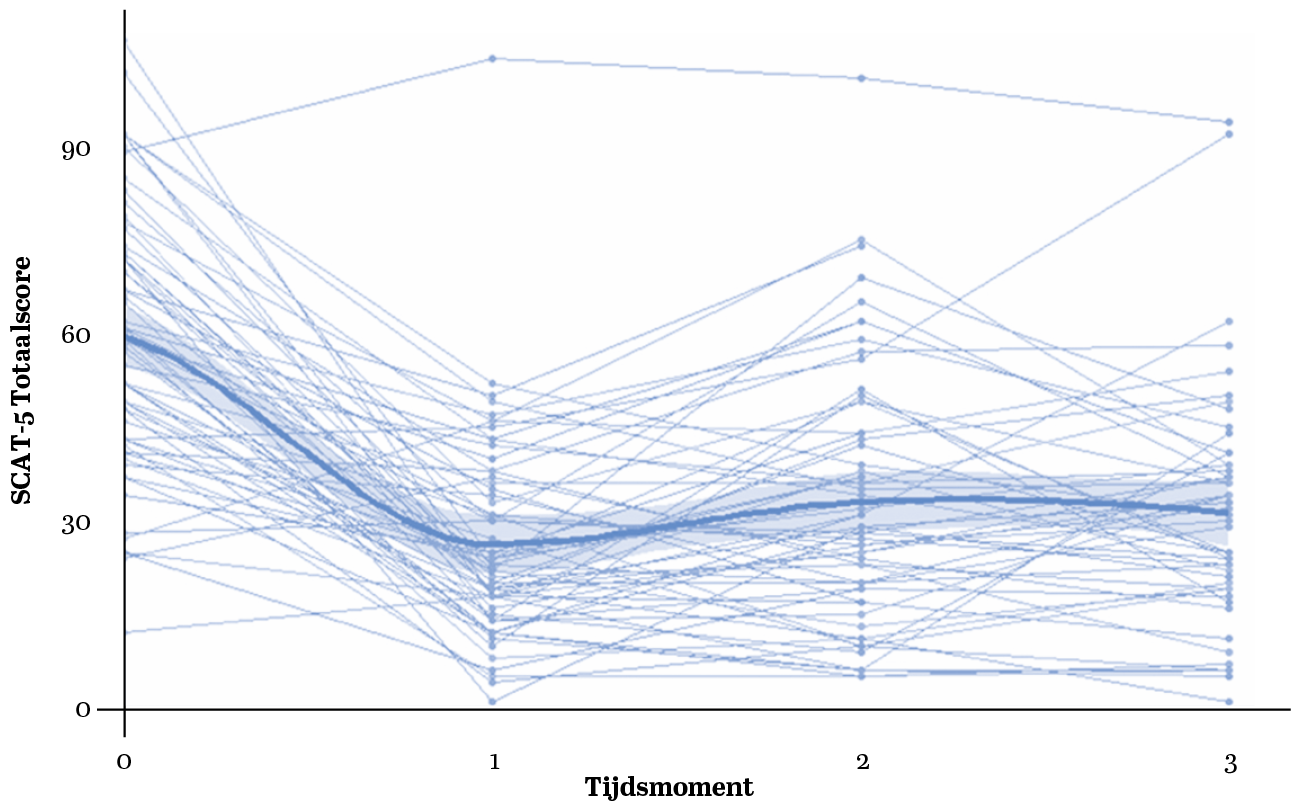
77% returned to normal with proven independent third-party validation

94% of patients reported symptom reduction after treatment

Proven Brain Remapping After Treatment utilizing third party analysis
Frequently Asked Questions
How confident should I be that I will get better if I come for treatment?

Third-party and our internal tracking show that roughly 75% of patients will get significantly better with treatment. The remainder will see some improvement in symptoms but not return to pre-injury levels. Between 5% and 7% of patients will see no improvement with treatment or a temporary regression of symptoms. We are improving at identifying what types of brain injuries don't respond to our treatment.
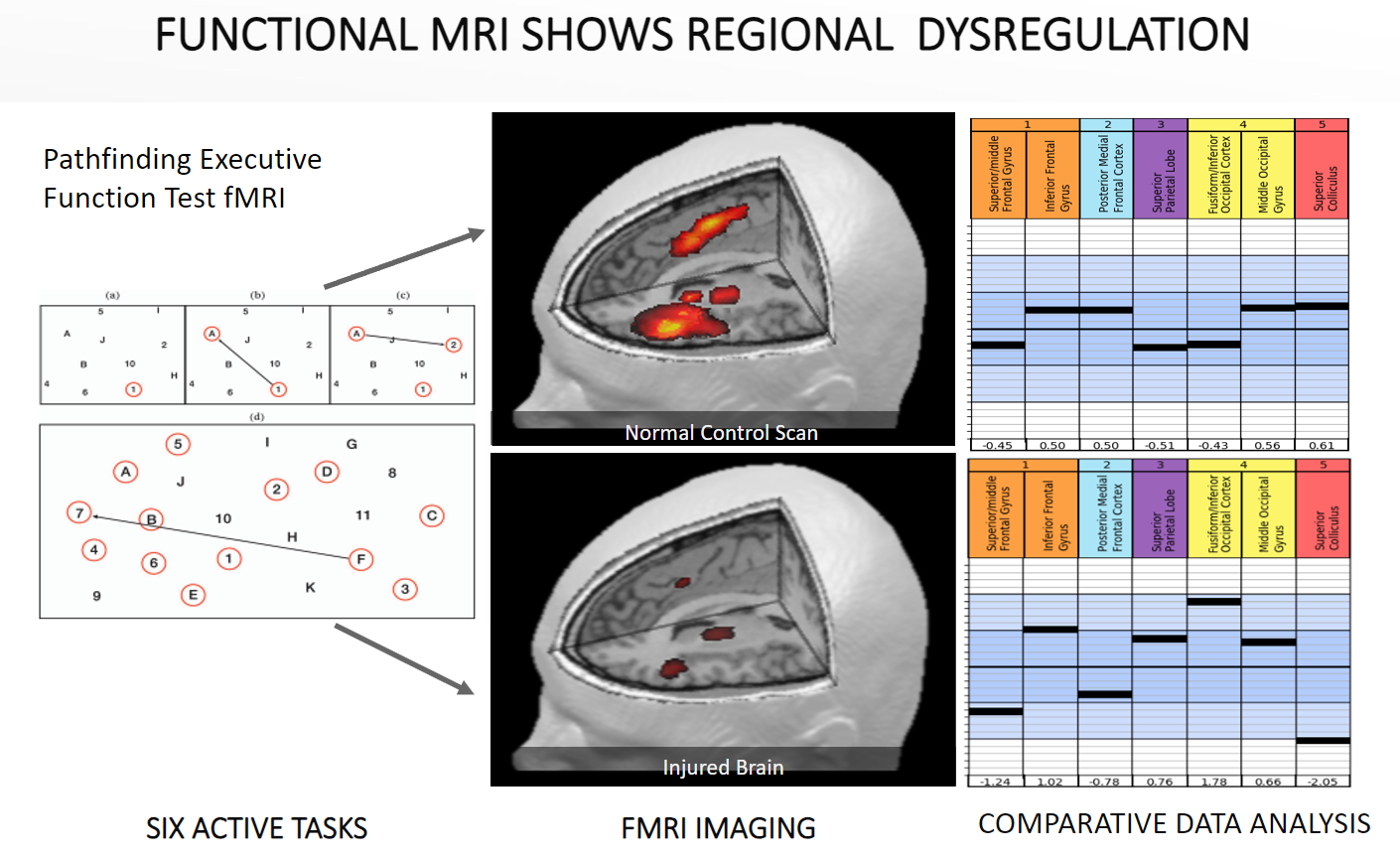
How does the fMRI allow you to customize my treatment?
All patients begin with a fMRI of their brain before we begin treatment. This allows us to look at how your brain in activating when it is doing standard tasks. We compare that with a database of healthy brains. From the scan, we are able to determine what areas of the brain are not working as they should. We can customize the Prepare, Activate, Recovery protocol to meet your needs.

This represents a standard normal curve. This patient has activations two standard deviations higher than normal, which can lead to brain fog, fatigue, and headaches. Parts of their brain are consuming far more resources than normal to compensate for an injury.
How is Cognitive FX different than other clinics?
Instead of conducting interviews with the patient about their symptoms, we take a more accurate approach and scan the brain, looking for differences between an injured brain and a normal brain.
Symptoms don't match up with the area of the brain that needs treatment. Hyperactivation across brain regions results in fatigue and headaches even though it may just be a few over active regions that are causing all the symptoms. On the other hand hypoactivation (low brain activation) can result in brain fog, taking longer to think etc. Without knowing what areas are impaired, it is hard to know where to focus treatment.
Secondly, during the week, we promote brain plasticity and stress the brain so it will try to remodel the neural pathways it had preinjury. To do that effectively, you can't have one or two appointments a week. The brain typically won't change 6 months after an injury without some serious work.

What is treatment like and what kinds of treatment will I get?
Treatment will last 1 or 2 weeks depending on your injury severity and to a lesser degree age. Treatment is between 6-9 hours every day for the week with a shorter day on Friday to accommodate an exit scan. We follow a Prepare, Activate and Recovery strategy for treatment. The types of therapy you could receive are: physical therapy, occupational therapy, speech therapy, cognitive therapy, vision therapy, massage, vestibular therapy, brain wave entrainment, CO2 therapy, dynavision, NSI, Righteye, TOMAR, REAX Board, HIIT, psychology depending on your needs.
The activation portion of the treatment is the most individualized. The Prepare phase is based on increasing the blood flow and creating neurochemicals (BDNF, dopamine, acetylcholine, etc.) that help with brain plasticity and neurogenesis.

How do I know if Cognitive FX is right for me and my injury?
If you have been dealing with symptoms for over 9 months, the research shows that without intervention, the likelihood of recovery is very low. The data shown above shows that 77% returned to normal SCAT 5 testing results. The average patient was over 4 years post-injury, so there is hope.
If you are longer than 6 months post-injury and symptoms aren't improving or getting worse, you are an ideal patient. If you have had multiple concussions and have severe symptoms and you are less than 6 months, you are also an ideal treatment candidate. If you have only had one concussion and are less than 6 months continue with your local treatment or see if you will recover. If, after 6-9 months, you haven't improved, reach out to us.

Will I be able to do treatment with my symptoms?
We have treated thousands of patients that have post-concussion syndrome or a mild TBI. We have lots of techniques that will help lessen any flair-up in symptoms. We also schedule recovery sessions in your schedule so you can rest and prepare for the next activation window.
Doctors




.png?width=250&height=75&name=Untitled%20(1).png)


Brain Injury Recovery Timeline: When Should You Seek Treatment?
Evidence-based recovery trajectories showing typical vs. prolonged recovery patterns. Interactive data points reveal key statistics from peer-reviewed research.
Treatment Recommended
Experiencing persistent headaches or symptoms beyond 6 weeks?
Evidence shows early treatment leads to better outcomes.
Research References
- McCrory P, et al. (2017). Consensus statement on concussion in sport—the 5th International Conference on Concussion in Sport. British Journal of Sports Medicine, 51(11):838-847. doi:10.1136/bjsports-2017-097699
- Makdissi M, et al. (2010). Natural history of concussion in sport. American Journal of Sports Medicine, 38(3):464-471. NCBI Reference
- Kontos AP, et al. (2020). Less Than Half of Patients Recover Within 2 Weeks of Injury. JOPT, 50(5):254-260. PMID: 32132366
- McClincy MP, et al. (2006). Recovery from sports concussion. Brain Injury, 20(1):33-39.
- Polinder S, et al. (2018). Multidimensional Approach to Post-concussion Symptoms. Frontiers in Neurology, 9:1113. PMC6306025
- Ellis MJ, et al. (2021). TRICORDRR score. PLOS Medicine, 18(7):e1003652. doi:10.1371/journal.pmed.1003652
- Leddy JJ, et al. (2020). Active Recovery from Concussion. Current Pain and Headache Reports, 24(6):27. PMC7046089
- King LA, et al. (2024). Getting rehab earlier improves outcomes. OHSU Study. OHSU News
Patient Testimonials
You deserve to heal and feel better.
You're tired of going from specialist to specialist and not seeing the improvements you want.
Now's the time to find out if a personalized approach customized to your actual brain scan delivered by a multidisciplinary team can treat the root causes of your symptoms so you can return to the life you want.
Answer 20 questions to tell us about your injury and find out if treatment could be right for you with a free patient consultation.