You did everything right.
You found the tick. You recognized the rash. You went to the doctor immediately. You took every single antibiotic exactly as prescribed. Maybe you even did a second round. Or a third.
Your blood tests came back clear. Your doctor said the infection was gone. You were supposed to get better.
But here you are, six months later. Maybe a year. Maybe longer. Still exhausted by noon. Still forgetting words mid-sentence. Still dealing with headaches that won't quit. Still wondering if this fog in your brain will ever lift.
And the worst part? The looks you get when you try to explain that you're still sick. The subtle (or not so subtle) suggestions that maybe it's stress. Maybe it's depression. Maybe it's anxiety. Maybe it's all in your head.
If this is your story, please hear this: You are not imagining this. You are not crazy. And you are not alone.
What you're experiencing has a name, a biological explanation, and most importantly, treatment options that work differently than anything you've tried before.
You're Not Alone (And You're Definitely Not Crazy)
Let's start with the numbers, because sometimes validation begins with simply knowing you're not the only one.
According to research from the Johns Hopkins Lyme Disease Research Center, approximately 10-20% of patients who receive prompt, appropriate antibiotic treatment for Lyme disease never fully recover. A 2022 study from their team found that even among patients who were diagnosed early and treated quickly, 14% went on to develop what's called Post-Treatment Lyme Disease Syndrome, or PTLD.
That's not a tiny fraction. That's roughly one in every six or seven people who do everything "right."
If you've spent the past several months (or years) being told that your symptoms don't make sense, that the infection is gone so you should be fine, that there's nothing more that can be done... those statistics tell a very different story. They tell you that what you're experiencing is well-documented, medically recognized, and shared by hundreds of thousands of people.
The problem isn't that your symptoms aren't real. The problem is that the medical system hasn't caught up to the science of why they persist.
Why Antibiotics Worked—But You Still Feel Terrible
Here's something that might help the pieces start falling into place.
The antibiotics did their job. They killed the Borrelia bacteria that cause Lyme disease. Your doctor was right about that. The infection, in the traditional sense, is gone.
But here's what most patients are never told: killing the bacteria doesn't automatically undo the damage they caused.
Groundbreaking research published in 2025 by scientists at Northwestern University has shed new light on exactly why this happens. Their team discovered that when the Lyme bacteria are killed by antibiotics, they don't simply disappear. Instead, fragments of their cell walls, called peptidoglycans, persist in the body long after the living bacteria are gone.
These bacterial fragments have unusual chemical properties that allow them to stick around. And here's the key part: your immune system continues to react to these remnants as if the infection were still active. The bacteria are dead, but the inflammatory alarm bells keep ringing.
Think of it like this. Imagine someone breaks into your house and your security alarm goes off. The police arrive, catch the intruder, and take them away. The threat is gone. But somehow, the alarm system got damaged in the process. Now it won't stop sounding. Day after day, the alarm keeps blaring, even though there's no intruder anymore.
That's essentially what's happening in your body. The "intruder" (the bacteria) is gone. But your immune system's alarm (the inflammatory response) is stuck in the "on" position.
This is why more antibiotics don't help. A comprehensive 2024 systematic review published in the European Journal of Neurology analyzed eight randomized controlled trials examining whether additional antibiotic treatment helped PTLD patients. The conclusion was clear: extended antibiotics showed no improvement in quality of life, depression symptoms, cognitive function, or fatigue. In fact, the additional treatment often caused more adverse events without providing benefit.
This isn't because antibiotics are bad. They were necessary and appropriate for treating the active infection. But once the infection is cleared, you're dealing with a different problem entirely. And that problem requires a different solution.
What's Actually Happening in Your Brain Right Now
If you've experienced the cognitive symptoms of PTLD, you already know something is wrong with your brain. The word-finding difficulties. The mental fatigue that hits after simple tasks. The feeling of trying to think through wet concrete. The short-term memory that used to be sharp and now feels like a sieve.
For years, patients describing these symptoms were often dismissed. "The tests look normal." "There's no infection." "Maybe try some stress management."
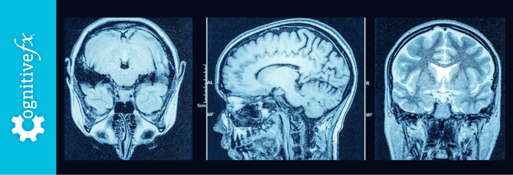
But in 2018, researchers at Johns Hopkins University published findings that changed the conversation. Using advanced PET imaging, they were able to visualize what was happening inside the brains of PTLD patients. And what they found was remarkable.
The study showed elevated markers of neuroinflammation across eight different brain regions in patients with persistent Lyme symptoms. The marker they measured, called the translocator protein, or TSPO, is a well-established indicator of brain inflammation.
<!-- INSERT INFOGRAPHIC: ptld-brain-regions.html -->
In other words, they could see the inflammation. They could measure it. They could prove it was there.
The researchers' conclusion was pointed and important: "Lyme-disease-associated cognitive symptoms are biologic and measurable, not psychosomatic."
Read that again if you need to. Your symptoms are biologic and measurable. Not psychosomatic. Not imagined. Not "just stress."
This neuroinflammation explains so much of what PTLD patients experience. When your brain is inflamed, it can't function properly. Neural pathways that should fire quickly become sluggish. The brain's energy resources get diverted to fighting inflammation instead of supporting normal cognitive function. Blood flow patterns change. Neurotransmitter signaling gets disrupted.
The result is exactly what you've been experiencing: fatigue that sleep doesn't fix, cognitive difficulties that make you feel like you've aged decades overnight, and a general sense that your brain is working at a fraction of its former capacity.
The Treatment Shift Nobody Told You About
Here's where things start to get hopeful.
If PTLD isn't an active infection problem anymore but rather a brain inflammation and function problem, then the treatment approach needs to change accordingly. You don't need more antibiotics. You need brain rehabilitation.
This concept might sound unusual if you've never heard it before. Brain rehabilitation is typically associated with traumatic brain injuries, strokes, and concussions. But the overlap between PTLD and these conditions is significant and increasingly recognized.
In fact, the Johns Hopkins Lyme Disease Research Center now specifically recommends this approach. According to their guidance (cited by Project Lyme), "People with persistent Lyme disease may find relief for their neurological symptoms at interdisciplinary clinics that specialize in brain rehab." They note that "these clinics generally use concussion and mild traumatic brain injury guidelines" because the symptoms and underlying dysfunction are remarkably similar.
Why does this work? Because regardless of what originally caused the brain inflammation—whether it was an impact injury, an infection, or something else—the path to recovery involves similar principles:
Reducing inflammation through targeted interventions. Restoring healthy blood flow to affected brain regions. Retraining neural pathways that have become dysfunctional. Addressing the autonomic nervous system dysregulation that often accompanies neuroinflammation. And rebuilding cognitive stamina and function through structured rehabilitation.
This represents a fundamental paradigm shift. Instead of continuing to chase an infection that's already gone, brain rehabilitation targets the actual problem: a brain that's been damaged by inflammation and needs help healing.
What Brain Rehabilitation Actually Looks Like for PTLD
If you've been living with PTLD for months or years, you might be skeptical of anything promising improvement. You've probably tried supplements, special diets, various medications, and maybe even some alternative treatments. Some might have helped a little. Most probably didn't.
Brain rehabilitation is different because it's not trying to kill something or add something to your body. It's working directly with your brain's own capacity for recovery and adaptation.
At specialized clinics that treat neurological conditions like PTLD, the approach typically begins with understanding exactly what's happening in your individual brain. Not everyone with PTLD has the same pattern of dysfunction. Some patients have more issues with blood flow regulation. Others have more significant problems with the connection between brain regions. Some struggle primarily with autonomic function (the system that controls heart rate, blood pressure, and other automatic processes). Many have some combination of all of these.
Advanced imaging techniques can map out which areas of your brain are underperforming and which pathways aren't communicating properly. This allows treatment to be targeted rather than generic.
Brain rehabilitation often includes:
Neurovascular Coupling Exercises: These help restore the relationship between brain activity and blood flow. When your brain works harder, it needs more blood flow to deliver oxygen and glucose. In many PTLD patients, this coupling is impaired, meaning the brain doesn't get the resources it needs when it needs them.
Autonomic Nervous System Rehabilitation: This addresses the dysregulation that causes symptoms like heart rate variability issues, temperature dysregulation, and exercise intolerance. Many PTLD patients describe feeling like their "fight or flight" system is constantly activated. This isn't imaginary; it's a measurable dysfunction that can be treated.
Cognitive Rehabilitation Exercises: These progressively challenge the brain in specific ways to rebuild function. Just as physical therapy rebuilds muscle strength and coordination after an injury, cognitive rehabilitation rebuilds neural pathways and cognitive stamina.
Vestibular and Visual Therapies: Many PTLD patients have dysfunction in how their brain processes balance and visual information. This contributes to dizziness, difficulty concentrating, and the "foggy" feeling many describe.
Carefully Calibrated Physical Therapies: These are designed to avoid the post-exertional malaise that many PTLD patients experience. The goal is to gradually increase capacity without triggering setbacks.
The intensive, interdisciplinary nature of this approach is important. These aren't isolated treatments delivered once a week over many months. They're coordinated interventions delivered by a team of specialists who understand how each piece fits together. This concentrated approach often produces faster results than scattered, piecemeal treatments.
The Path Forward: What Recovery Actually Looks Like
Let's be honest and realistic about what brain rehabilitation can and cannot do for PTLD patients.
This is not a magic cure. No responsible treatment center would promise that. Your journey with Lyme has likely taught you to be skeptical of anyone promising overnight miracles, and that skepticism is healthy.
What brain rehabilitation offers is the potential for meaningful, measurable improvement in how your brain functions. Patients often report:
- Reduced severity and frequency of brain fog episodes
- Improved ability to sustain cognitive effort without crashing
- Better word-finding and verbal fluency
- Decreased fatigue
- Improvement in headaches
- Better tolerance for physical activity
- Reduced anxiety and improved mood
- A general feeling that their brain is "coming back online"
The degree of improvement varies from person to person depending on factors like how long symptoms have persisted, what other health conditions are present, and individual biology. But the central point is this: improvement is possible. Your brain has not been permanently broken by Lyme disease. Neural plasticity—your brain's ability to change, heal, and adapt—is still working in your favor.
Many patients describe the experience of brain rehabilitation as finally addressing the right problem. After years of treating an infection that was already gone, or being told nothing was wrong when clearly something was, receiving treatment that actually targets the dysfunction in their brain feels like a turning point.
Taking the First Step When You're Exhausted
If you're reading this with the particular kind of fatigue that PTLD brings, the idea of researching yet another treatment option might feel overwhelming. You've probably already spent countless hours online, tried numerous approaches, and experienced the disappointment of treatments that didn't work.
Here's what we'd suggest: start with a conversation.
At Cognitive FX, we specialize in treating patients with neurological symptoms that persist after various causes, including post-concussion syndrome, traumatic brain injury, and yes, the neuroinflammation that follows Lyme disease. Our approach uses functional brain imaging, specifically, functional MRI, to understand exactly what's happening in your brain, then creates a targeted treatment plan based on those findings.
We know that PTLD patients often come to us feeling dismissed and skeptical. Many have been told their symptoms aren't real or that nothing can be done. We approach every patient differently, because we understand that your brain is unique and your treatment needs to be too.
If you've been living with persistent symptoms after Lyme treatment and you're ready to try an approach that addresses what's actually happening in your brain, we'd welcome the chance to talk with you. A consultation can help you understand whether brain rehabilitation might be appropriate for your situation and what the process would look like.
You've already proven you're persistent by fighting this far. You've advocated for yourself when others didn't believe you. You've kept searching for answers when the easy thing would have been to give up.
That persistence matters. And it might be exactly what leads you to the treatment approach that finally makes a difference.
References
- Johns Hopkins Lyme Disease Research Center. "Post-Treatment Lyme Disease Syndrome." https://www.hopkinslyme.org/lyme-disease/post-treatment-lyme-disease-syndrome/
- Rebman AW, et al. "The Clinical, Symptom, and Quality-of-Life Characterization of a Well-Defined Group of Patients with Posttreatment Lyme Disease Syndrome." Frontiers in Medicine, 2022. PMC9126538
- Berende A, et al. "Randomized Trial of Longer-Term Therapy for Symptoms Attributed to Lyme Disease." New England Journal of Medicine, 2016. DOI: 10.1056/NEJMoa1505425
- Klempner MS, et al. "Two Controlled Trials of Antibiotic Treatment in Patients with Persistent Symptoms and a History of Lyme Disease." New England Journal of Medicine, 2001. DOI: 10.1056/NEJM200107123450202
- "Prolonged antibiotic therapy in post-treatment Lyme disease syndrome: A systematic review and meta-analysis." European Journal of Neurology, 2024. DOI: 10.1111/ene.16293
- Northwestern University. Research on Borrelia peptidoglycan persistence in post-treatment Lyme disease. Science Translational Medicine, 2025. Science Translational Medicine
- Coughlin JM, et al. "Imaging glial activation in patients with post-treatment Lyme disease symptoms: a pilot study using [11C]DPA-713 PET." Journal of Neuroinflammation, 2018. PMID: 30567544
- Project Lyme / Johns Hopkins Lyme Disease Research Center. Recommendations for brain rehabilitation approaches in PTLD patients. https://www.projectlyme.org/
Related Articles
Cognitive FX specializes in treating patients with persistent neurological symptoms through functional brain imaging and targeted rehabilitation. If you're experiencing ongoing symptoms after Lyme treatment, schedule a consultation to learn whether our approach might help.