Cognitive FX’s Long Haul COVID Treatment Protocol
Most patients with COVID-19 recover within a few days or weeks after a brief acute infection. However,about 10%experience long-term symptoms such as brain fog, fatigue, headaches, shortness of...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.
If this sounds familiar and started after a COVID-19 infection, you're not imagining things. What you're experiencing has a name: long COVID insomnia. And according to research published in the Journal of Clinical Sleep Medicine (2025), you're far from alone.
The reality: Sleep disturbances affect approximately 40-52% of people with long COVID, making it one of the most common and disabling symptoms of the condition. Perhaps even more concerning, these sleep problems don't simply fade away on their own. Studies show that insomnia symptoms can persist for 12 months or longer following COVID-19 infection.
The good news? These sleep problems are treatable. And understanding what's actually happening in your body is the first step toward getting the rest you desperately need.
Before we go further, take a moment to consider whether your sleep problems might be connected to COVID. Do any of these apply to you?
If you checked several of these boxes, long COVID may be affecting your sleep. Keep reading to understand why this happens and what can actually help.
Long COVID insomnia isn't simply a matter of stress or anxiety (though those can certainly make things worse). Research has revealed that the SARS-CoV-2 virus can directly affect multiple body systems involved in regulating sleep. Understanding these mechanisms helps explain why standard sleep remedies often fall short for long COVID patients.
A 2023 study published in The Lancet eClinicalMedicine found structural changes in the thalamus of long COVID patients. The thalamus serves as your brain's central relay station and plays a critical role in controlling sleep-wake cycles. When this region is disrupted, falling asleep and staying asleep becomes significantly harder.
Beyond structural changes, researchers have observed disruptions in what's called neurovascular coupling (NVC). In healthy brains, neurons signal to nearby blood vessels when they need oxygen and nutrients. This dynamic communication keeps different brain regions functioning properly.
In long COVID patients, this signaling gets disrupted in certain areas. If the affected regions include those responsible for sleep regulation (like the hypothalamus or brainstem), the result is exactly what so many people experience: difficulty falling asleep, waking frequently, and feeling unrested even after sleeping.
Perhaps the most significant factor in long COVID sleep problems involves the autonomic nervous system (ANS). This is the part of your nervous system that operates automatically, controlling heart rate, digestion, breathing, and yes, sleep.
Your ANS has two main branches:
The sympathetic nervous system (SNS) activates during stress or danger. It increases heart rate, directs blood to muscles, and creates that alert, "on guard" feeling. Think of it as your body's accelerator.
The parasympathetic nervous system (PNS) activates during rest and relaxation. It slows heart rate, promotes digestion, and prepares your body for sleep. This is your body's brake pedal.
Normally, these two systems trade off throughout the day based on what you need. When you're working or exercising, the SNS takes over. When you're relaxing in the evening or sleeping, the PNS should dominate.
The problem in long COVID? Research shows that many patients experience persistent SNS dominance. Your body stays stuck in "fight or flight" mode even when there's no danger. The result is a racing heart, anxiety, and the inability to wind down for sleep.
This autonomic dysfunction (sometimes called dysautonomia) affects up to 70% of people with long COVID according to some estimates. It also explains why you might experience other symptoms alongside insomnia, such as heart palpitations when standing, dizziness, temperature regulation problems, or digestive issues.
COVID-19 triggers a significant inflammatory response in the body. While inflammation is a normal part of fighting infection, in some people it persists long after the acute illness resolves.
This chronic low-grade inflammation affects sleep in several ways. Inflammatory molecules called cytokines directly influence sleep-regulating chemicals in the brain. The relationship becomes a vicious cycle: poor sleep weakens immune function, which can worsen inflammation, which further disrupts sleep.



If you've been struggling to sleep for weeks or months, reaching for a pill might seem like an obvious solution. While sleep medications have their place, they come with significant limitations for long COVID patients.
The core issue: Most sleep medications treat symptoms rather than underlying causes. They may help you fall asleep, but they don't address the nervous system dysfunction, brain changes, or inflammation driving your insomnia.
Common sleep medications and their drawbacks:
Benzodiazepines (like Xanax, Valium, Ativan) can help short-term but carry high risks of dependency. They also suppress the deep, restorative sleep stages your body needs most.
Non-benzodiazepine sleep aids (like Ambien, Lunesta) were designed as safer alternatives but can still cause dependency, memory problems, and next-day drowsiness.
Over-the-counter sleep aids (like diphenhydramine/Benadryl) often leave you groggy and lose effectiveness quickly.
Melatonin shows some promise for long COVID patients. Research published in 2022 found that melatonin supplements can improve sleep quality and may even have anti-inflammatory benefits. However, timing and dosage matter significantly, and results vary widely between individuals.
The bigger picture: Insomnia is rarely an isolated symptom in long COVID. Most patients experience fatigue, brain fog, headaches, or other symptoms alongside their sleep problems. Treating only the insomnia while ignoring these connected issues rarely produces lasting improvement.
Further reading: Natural treatment options for long COVID
At Cognitive FX, our treatment doesn’t involve the use of medication. We don’t treat each symptom as an isolated problem to be solved; instead, we realize that long COVID symptoms are all related. Therefore, we treat long COVID as a whole using a combination of physical exercise and multidisciplinary therapy.
Before treatment starts, all patients must undergo a detailed medical examination. Our team will ask you about your symptoms and medical history and conduct a physical, cognitive, and psychological assessment to determine how long COVID is affecting your health. This assessment includes a:
Patients also complete a brain imaging scan called functional NeuroCognitive Imaging (fNCI) that’s designed to determine how and where the virus affected brain function. This scan checks how your brain is working in about 100 regions, as well as how these regions communicate with each other, while the patient performs a series of standardized cognitive tasks.
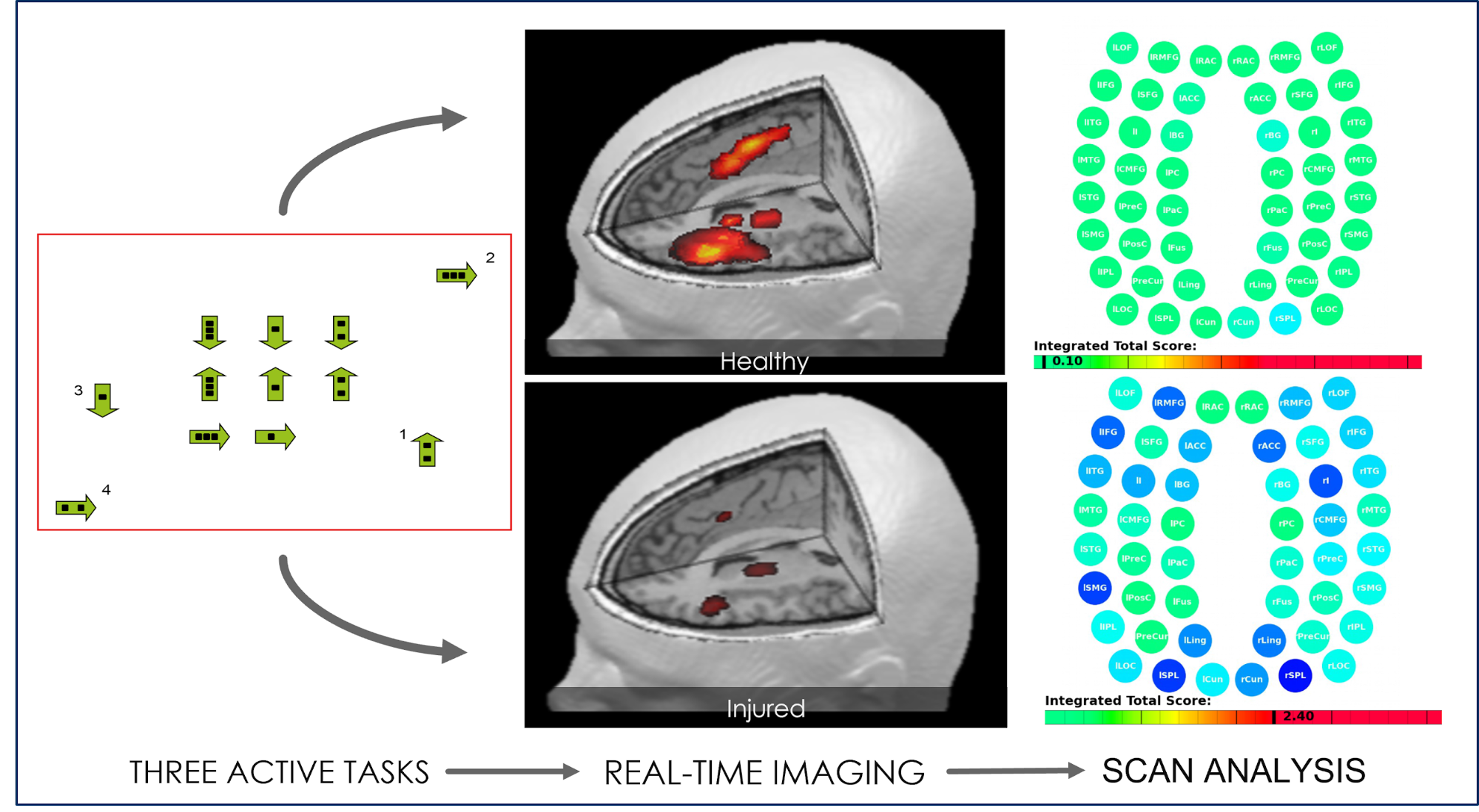
Once this examination is finished, our therapists gather all the information from the various tests and design a treatment plan to target specifically the areas of your brain that were most affected by COVID-19.
Typically, this involves a combination of aerobic exercise and multidisciplinary therapies. The aim is to take advantage of a process in the brain called the post-exercise cognitive boost (PECB). PECB triggers the release of chemicals in the brain, including one called brain-derived neurotrophic factor (BDNF). BDNF improves communication between different areas of the brain and promotes the growth of brain cells. As a result, the patient’s brain is more flexible and can benefit more from subsequent therapy.

Therapies used during treatment include:
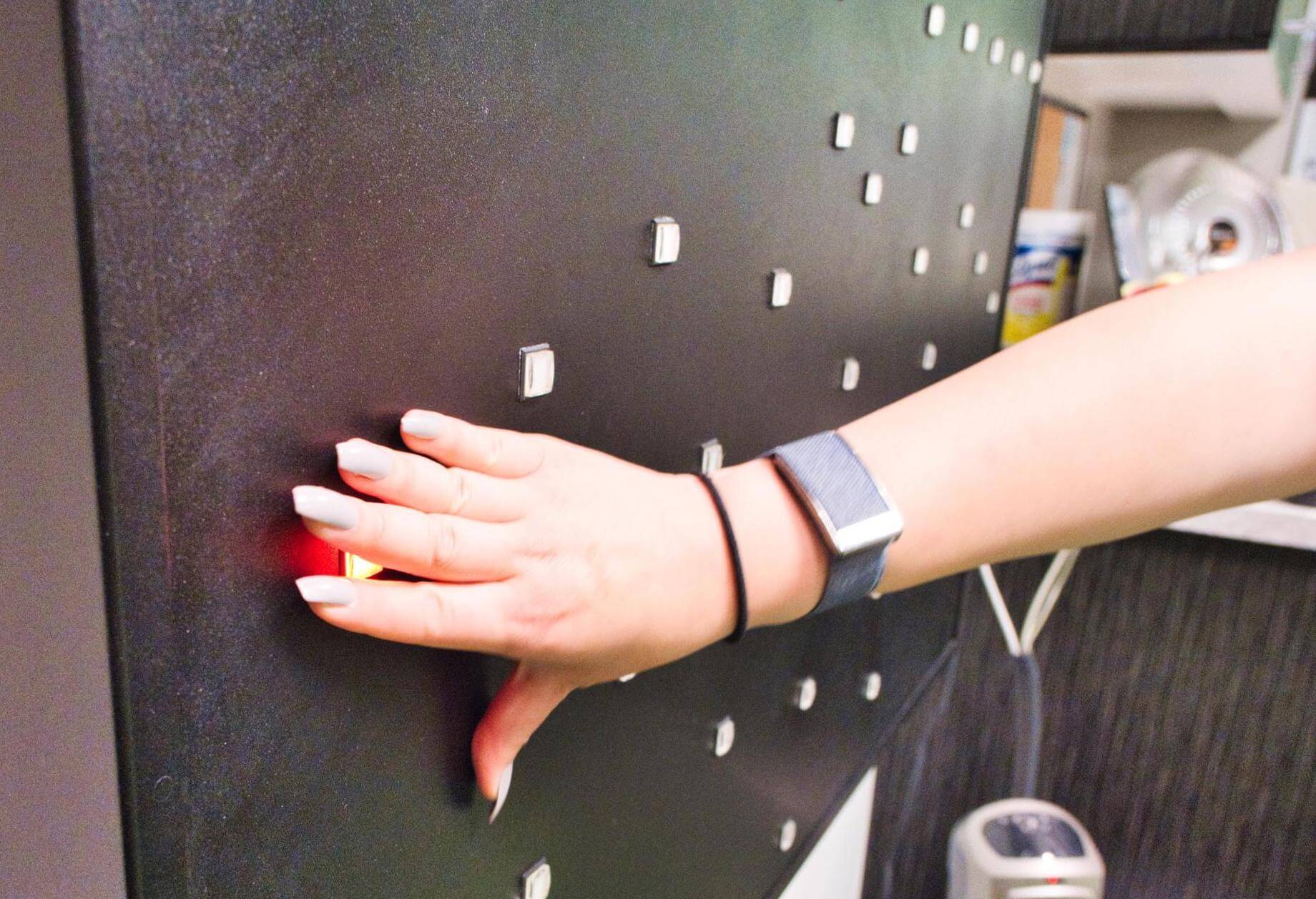
Each patient will have an unique combination of exercises from these therapies to address their symptoms. Some therapies can be administered in quick succession or even in combination with each other. For example, our therapist may ask you to balance on a Bosu ball while tossing color-coordinated balls back and forth and naming an animal for each letter of the alphabet. This forces your brain to activate specific areas so you stay balanced, catch the ball, and think of the next animal name — all at the same time. This encourages the restoration of healthy neurovascular coupling as the brain grapples with the increased demand for resources in multiple brain regions simultaneously.

Throughout the day, patients are also given opportunities to rest and relax so their brains can recover before the next therapy. This may include a neuromuscular massage to the neck and shoulders, breathing exercises, or mindfulness meditations, for example. For patients with insomnia, these activities can be extremely helpful to re-teach the brain how to relax and unwind. Some of these exercises can also be done at home, which further helps the patient’s recovery.
After treatment, our patients repeat the initial evaluation, including the physical and cognitive assessment, and discuss with our team how their symptoms changed during treatment. Patients also undergo a second fNCI scan, which allows our team to assess their progress and suggest ways to move forward. For example, if we feel that you may benefit from further therapy in a particular area (such as vision), we can refer you to suitable specialists.
Further reading: Vision problems after COVID
Finally, you will meet with one of our therapists to go over your results and receive a series of homework exercises. This usually includes physical exercises, cognitive activities, visual and vestibular exercises, and relaxation techniques designed to help during your recovery. These exercises take about an hour to complete. Initially, patients should do them five times a week, but the frequency can be reduced as symptoms improve.
Since the COVID pandemic started, we’ve treated dozens of patients with long COVID. All were experiencing several different symptoms, including headaches, brain fog, and dizziness, among others.
After treatment, patients experienced significant improvements in many lingering symptoms of COVID-19. Most patients reported an overall improvement in quality of life and say their symptoms are easier to cope with in their daily lives.
If you’re experiencing insomnia or other sleep-related problems and are considering coming to Cognitive FX for treatment, it’s worth mentioning that our previous patients experienced better sleep after treatment.
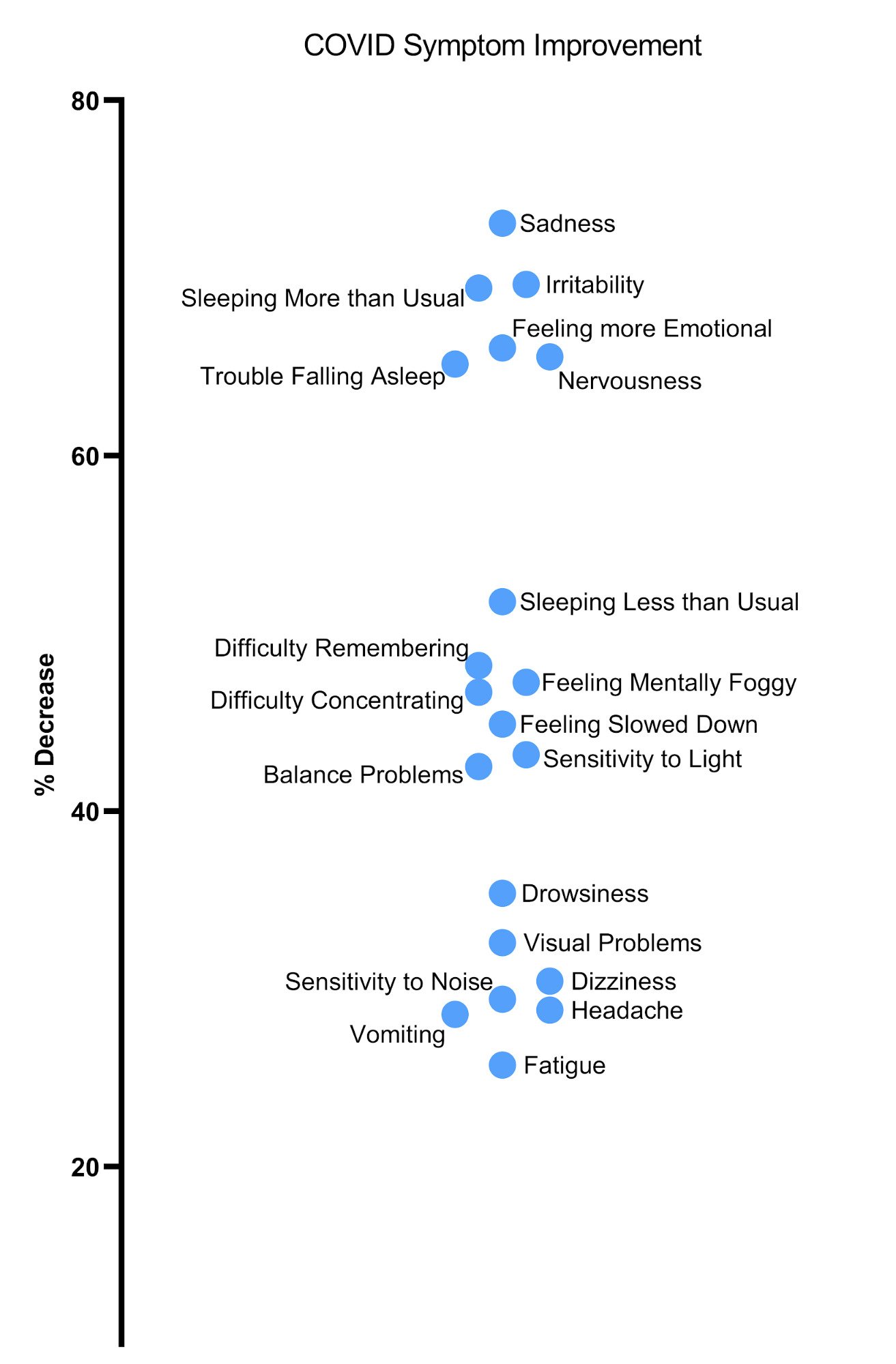
Meanwhile, scores in areas such as fatigue tend to improve once the patient has time to rest and recover at home. Treatment is intense, after all! Visual problems tend to respond more slowly; patients with notable vision problems often need continued therapy at home for full improvement to take effect.
Want to find out if you’re eligible for treatment at our specialized clinic? Contact our team to schedule a consultation.

Whether or not you ultimately pursue treatment at a specialized clinic, there are evidence-based strategies that can help improve your sleep tonight.
Maintain consistent sleep and wake times. Go to bed and wake up at the same time every day, including weekends. This helps regulate your internal clock. If you find yourself needing to hit snooze repeatedly, try moving your bedtime earlier.
Get morning light exposure. Spend at least 15-30 minutes outside in natural light within an hour of waking. Light exposure is one of the most powerful signals for resetting your circadian rhythm. If you can't get outside, sit by a window with direct sunlight.
Limit daytime naps. If you must nap, keep it to 20 minutes or less before 3 p.m. Longer or later naps interfere with nighttime sleep pressure.
Practice breathing exercises. Box breathing (inhale for 4 counts, hold for 4, exhale for 4, hold for 4) activates the parasympathetic nervous system and can help shift your body out of fight-or-flight mode. Practice this throughout the day, not just at bedtime.
Create a wind-down routine. Start relaxing 60-90 minutes before bed. Dim lights, avoid screens, and engage in calming activities like reading, gentle stretching, or listening to quiet music.
Consider a hot bath or shower. The subsequent drop in body temperature after warming up signals to your body that it's time to sleep.
Keep your bedroom cool. Most people sleep best between 65-68°F (18-20°C). Your body temperature naturally drops during sleep, and a cool room supports this process.
Use your bed only for sleep. Don't work, watch TV, or scroll your phone in bed. This helps your brain associate the bedroom with sleep rather than wakefulness.
Address noise and light. Use earplugs, a white noise machine, blackout curtains, or an eye mask if needed.
Exercise, but time it right. Regular physical activity improves sleep quality and can help regulate the autonomic nervous system. However, intense exercise within 3-4 hours of bedtime can interfere with sleep. Morning or early afternoon workouts are ideal.
Limit caffeine. Avoid caffeine after noon. Even if you think caffeine doesn't affect you, it may still disrupt sleep quality.
Watch your evening diet. Avoid large meals, alcohol, and excessive fluids close to bedtime. All can disrupt sleep in different ways.
Keep a sleep diary. Record when you go to bed, when you fall asleep, how many times you wake, when you get up, and how you feel. This data can reveal patterns and help you (or a healthcare provider) identify what's working and what isn't.
Try these strategies consistently for 2-3 weeks. If your sleep doesn't improve, or if you're experiencing other long COVID symptoms alongside insomnia, it may be time to explore additional options.
Signs that you may benefit from specialized treatment:
Long COVID sleep problems don't have to be permanent. Understanding that your insomnia stems from real physiological changes, not weakness or imagination, is an important first step. And knowing that targeted treatment can address these underlying issues offers genuine hope.
At Cognitive FX, we've helped hundreds of long COVID patients reclaim restful sleep and overall quality of life. Our intensive one-week program addresses the root causes of symptoms rather than just masking them.
Ready to find out if you're a candidate for treatment?
Schedule a free consultation with our team. During this call, we'll discuss your specific symptoms, answer your questions, and help you understand whether our approach might be right for you.
There's no obligation, and the consultation itself often provides valuable insights about your condition.
How long does long COVID insomnia typically last?
Without treatment, studies show that sleep disturbances can persist for 12 months or longer following COVID-19 infection. However, with appropriate intervention targeting the underlying causes, many patients see significant improvement within weeks.
Is melatonin safe for long COVID patients?
Generally yes, and some research suggests melatonin may have benefits beyond sleep for long COVID patients due to its anti-inflammatory properties. However, timing, dosage, and individual factors matter. Consult with a healthcare provider before starting any new supplement.
Can exercise help with long COVID insomnia?
Exercise can be beneficial, but it must be approached carefully. Some long COVID patients experience post-exertional malaise, where symptoms worsen after physical activity. Start slowly, monitor how you feel, and work with a provider who understands long COVID if possible.
What's the difference between long COVID insomnia and regular insomnia?
Long COVID insomnia typically involves multiple underlying mechanisms including nervous system dysfunction, brain changes, and chronic inflammation, rather than just stress or poor sleep habits. This is why standard insomnia treatments often fall short.
How soon after COVID infection might sleep problems start?
Sleep problems can begin during acute infection or emerge weeks to months afterward. Research shows that sleep disturbances most commonly start after recovery from the acute infection (68% of cases) rather than during it.
Struggling with symptoms beyond insomnia? Learn more about how we treat the full spectrum of long COVID symptoms:

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

Most patients with COVID-19 recover within a few days or weeks after a brief acute infection. However,about 10%experience long-term symptoms such as brain fog, fatigue, headaches, shortness of...

When the pandemic started, we were told that children wouldn’t be seriously affected by the virus. And while most children only experience a mild version of the disease, evidence shows that some...
COVID-19 can cause cognitive symptoms in some patients, such as short-term memory loss, difficulties concentrating, problems recalling words, and brain fog (a condition known as long COVID). While...

At the moment, treatment options for long COVID patients are limited. Many patients cope with their symptoms using existing medications or treatments targeting specific symptoms like headaches or...
Memory and attention problems are common in long COVID patients: A recentstudyshowed that 70% of COVID long haulers experience memory and concentration difficulties for months after their initial...

Long COVID is real. Data shared by the Centers for Disease Control and Prevention (CDC) from theHousehold Pulse Survey(July/August 2022) show that more than 40% of adults in the United States have...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY