I started figure skating competitively when I was eight years old. I loved the feeling of flying across the ice, the “wind” racing across my skin, vaulting into the air and sailing through a landing. Like many, I dreamed of the Olympics, and I poured every ounce of energy into training.
But shortly after I turned thirteen, my health unraveled. Not all at once; it was slow and sneaky. At a doctor’s visit in 2005, I complained of fatigue and the inability to gain stamina, no matter how hard I worked out. My doctor waived it off as a series of colds.
That “series of colds” was actually the start of a 14-year search for answers.
When I finally quit skating at sixteen years old because of my health issues, I thought everything would get better, but it didn’t — and no one could tell me why.
No one could tell me why a super fit, serious athlete (nicknamed “Energizer Bunny” by my relatives) would experience sudden blood pressure drops after exercise, or get so exhausted that a lap around the rink was tiring. They couldn’t explain why I collected food sensitivities like trophies, or why I gradually felt less and less rested in the morning, even though I slept the whole night. When I had to read a science textbook over and over to retain the information, I thought I was the problem.
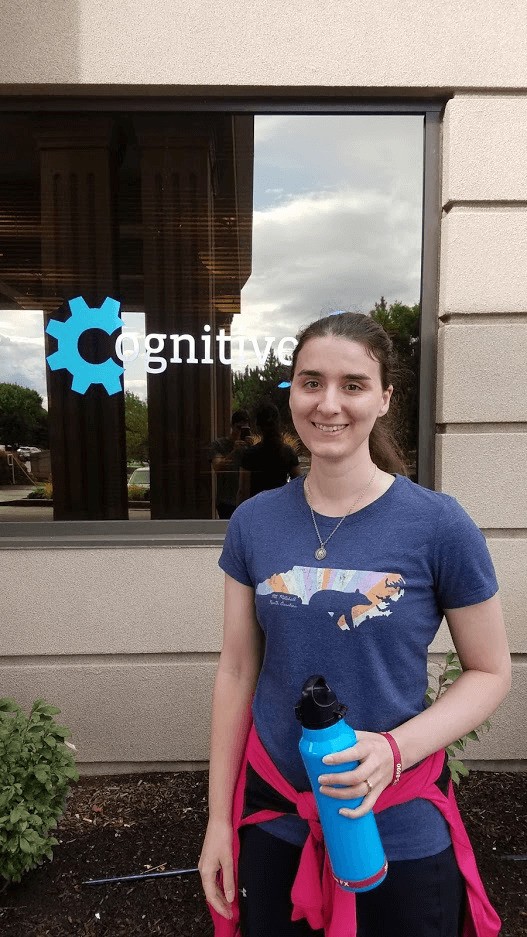
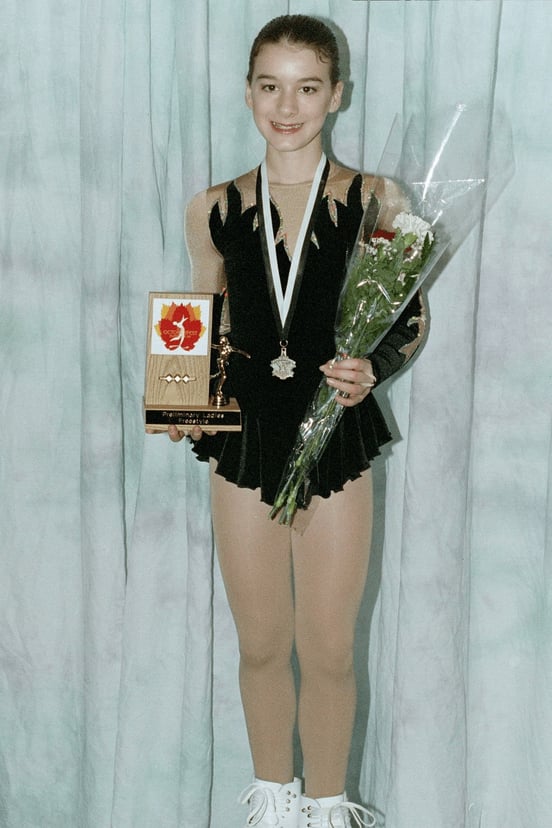
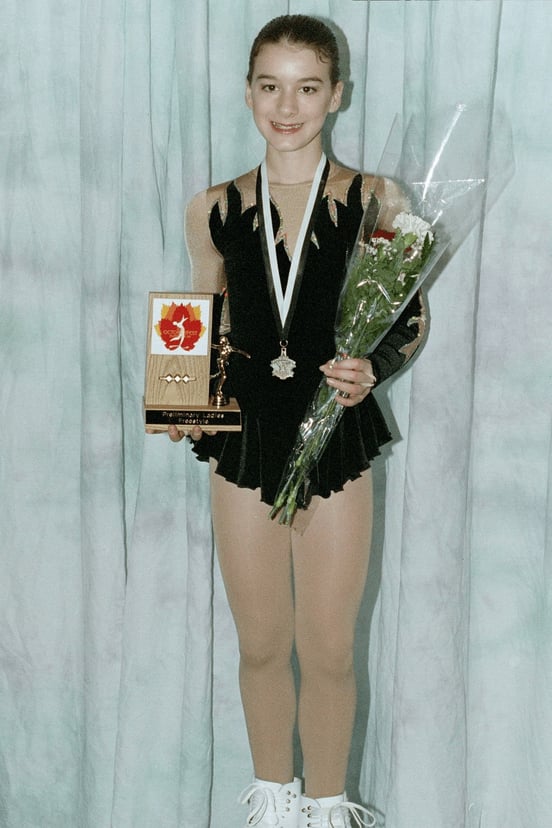 A photo from 2003, before all the health problems started. I really liked that flame dress!
A photo from 2003, before all the health problems started. I really liked that flame dress!
During the search for answers, we found pieces of the puzzle — celiac disease, endometriosis, hormone dysregulation, environmental allergies — but managing and treating those conditions never fixed my health the way I expected it to. I know what it’s like to have a doctor tell me that there’s nothing actually wrong with me. Or to say, “I’m so sorry. I don’t know what else to try.”
But I’m not writing because I’m still searching for answers. I’m telling my story now because I finally found the last puzzle piece: concussions.
I only made the connection because I started writing about concussions for work. In retrospect, there were plenty of clues to the underlying problem; I just didn’t know how to spot them. Once I went through testing and treatment, there was no question that post-concussion syndrome was the mystery illness I’d been fighting.
And spoiler alert: I am doing so much better than I was, even just three months out from treatment. My energy levels are higher, and my symptoms are less oppressive. It’s awesome. I just hope that by sharing my story, others suffering from the same “mystery illness” can get help, too.
If you’re experiencing symptoms that won’t resolve after a concussion, you’re not alone. And you’re not crazy. 95% of patients at Cognitive FX experience statistically verified restoration of brain function. To see if you are eligible for treatment, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
The Frog in the Pot: Why I Didn’t Connect My Symptoms to Concussions
When I was a kid, I thought a concussion happened when you hit your head really hard and lost consciousness and your eyes did funny things. Anything else, and it was just a bump — right?
Let’s clear a few things up:
- You can get a concussion without hitting your head (if your brain hits your skull from jostling or whiplash, it can still be injured).
- Even if you “only” have mild, tolerable symptoms that don’t completely sideline you, it’s still a concussion.
- You don’t have to experience loss of consciousness (i.e. a “blackout”) for it to “count”.
- You can tweak your schedule and arrange your life to minimize symptoms, but that doesn’t mean your symptoms aren’t real or worth treating.
- Symptoms don’t always go away, even if your injury was years ago.
- You can have symptoms after your concussion that don’t seem like they’re brain-related, making it harder to diagnose.
And knowing that, I realized that I’ve had at least three concussions, but probably more.
There was that time when I fell off the top of a playground into one of those curly-cue structures and rag-dolled my way down until my body thudded to the ground. I don’t remember the impact. All I remember was waking up to my dad and sister staring down at my motionless form, wondering if I had broken my neck. (I’m not sure how old I was, but I was definitely less than ten years old).
I also climbed a lot of trees. I fell out a few times. There was root-to-head contact at some point. Now that I think about it, I had a lot of headaches as a kid.
And then there was skating.
The Big Fall
Back when I was 12 or 13 (so 2004 or 2005), I was practicing a double lutz jump. You glide backward on your left outside edge, reach your right leg straight back, tap into the ice with the toe-pick, launch yourself in the air, and turn around twice before landing on your right foot.
 Me doing a double lutz, double toe-loop combination during a competition in 2007, several years after hitting my head on the ice.
Me doing a double lutz, double toe-loop combination during a competition in 2007, several years after hitting my head on the ice.
I was worn out after a long practice and my coach at the time was pushing me to do more, more, more. Always more. But something went wrong, and I came down on the heel of my blade instead of the ball of my foot. I went flying backward, my butt slammed into the ice, and my head whipped back & crashed into the ice immediately after.
I was terrified that I’d cracked my skull, but it was intact, and I wasn’t bleeding. As soon as I stood up, I knew I couldn’t keep skating that day. I felt nauseated and just “off.” I don’t remember much about the days afterward — all I know is that I didn’t take time off the sport. But if I had to pick a turning point for my health, that was it.
I was used to the more visible skating injuries — sprains, overuse injuries, knee problems — but concussions were new to me. I didn’t even know what the symptoms were. As long as I could walk, I was always back at the skating rink, even when I felt terrible.
A Gradual Decline
So, over time, it just got worse. My stamina gradually decreased. A few years after that fall, I would have to lie down on the bench after doing a program run-through (3-4 min of extreme cardio while trying to convince the audience it’s not hard at all would consistently trigger extreme lightheadedness).
In late 2006, we had gotten a diagnosis of “neurocardiogenic syncope,” a fancy name for your-blood-pressure-drops-suddenly-and-we-don’t-actually-know-why. That only happened because we measured my blood pressure immediately after intense cardio, and it was 92/60 (shout out to my mom who kept crazy accurate medical records for me). For reference, standard resting blood pressure is around 120/80, and it’s supposed to get higher when you exercise.
It didn’t matter how hard I worked; I just stopped improving. I wheezed through choreography even though I trained 5 days a week and did off-the-ice cardio 3-4 times per week. Eventually, I dreaded just doing some laps around the rink.
I also noticed that I could feel the more intense falls in my head, resulting in an increased headache (I say increased because I always had a headache by then). Even if the damage was subconcussive — meaning, not in itself enough to cause a concussion — the repeated jarring made everything worse.
My parents were convinced I was killing myself by continuing to skate, so in 2008, when I was sixteen years old, I had to quit. It was devastating to me. I had a lot of emotions to work through afterward.
 Doing a side layback spin (into a Biellmann) during a competition in 2007.
Doing a side layback spin (into a Biellmann) during a competition in 2007.
College Years & Beyond
Over the next few years, I got more and more out of shape. Exercise became even harder. I was tired most of the time, I’d get brain fog a lot, and my stomach started acting up (turned out that last one was mainly, but not entirely, from celiac disease).
During my junior year of college (early 2013), I wrote up a symptom list and tried a local doctor known for her willingness to troubleshoot difficult chronic illness. Here are some of the symptoms I noted at the time:
- Low basal body temperatures (consistent with thyroid dysfunction)
|
- Heart flutters after naps
|
|
|
- “Easily spooked, bad with crowds, irrational anger” (yes, I am directly quoting my past self)
|
- Mild depression and anxiety
|
|
- Situational dizziness/vertigo/light-headedness
|
|
- Hypoglycemic reactions (couldn’t survive without a regular supply of snacks/meals)
|
|
|
|
- Extreme nausea and stomach pain with heavy exercise
|
- Caffeine and alcohol intolerance
|
|
She confirmed that I had hypothyroidism and that my adrenocorticotropic hormone (ACTH) was low to nonexistent. ACTH is a hormone produced by the pituitary gland and regulated by the hypothalamus, both of which are located in the brain (you can see where I’m going with this). It tells the adrenal glands to make cortisol, which is a necessary hormone involved in many processes, but which is best known for its role in helping you handle stress.
And my cortisol levels would fluctuate. Sometimes it would be fine ... and then I’d go through something stressful (like finals, or getting a cold) and it would be ... not fine. So for a time, I took oral hydrocortisone, which really helped me through my last two years of college and my first year as a high school math and science teacher.
Unfortunately, many endocrinologists will tell you that you either have adrenal failure (from which there is no recovery) or your adrenal glands are fine. My struggles didn’t fit within the narrow confines of their clinical experience. One even told me that he wouldn’t consider my lab results (showing lower than normal cortisol and ACTH) as evidence because a different doctor ordered the test done, but when he tested me in his own practice, I was in the normal range again.
Joke’s on them — turns out they were right when they said it was “all in my head.” Head injuries can cause hormone dysregulation such as what I experienced.
Nevertheless, they insisted it would be best for me to stop taking hydrocortisone. Weaning off it was unpleasant, and handling life without it was worse. The years after my college graduation saw a sharp decline in health, especially after I lost hydrocortisone as my stop-gap fix.
At the time, the energy demand of teaching was way too high. Turns out that I also had a bad case of endometriosis at the time. It ratcheted up my pain levels and drained my already depleted energy. So in 2016, I quit teaching, had surgery, and worked hard on recovery.
While surgery helped a lot with the pain and gave me back some energy, I still had trouble exercising, still felt exhausted in the morning, and still had a very real cap on how much cognitive work I could handle in one day.
When 2018 rolled around, I had given up on finding answers. I just thought I was chronically ill, and that was my lot in life, something for me to accept and work around as best I could.
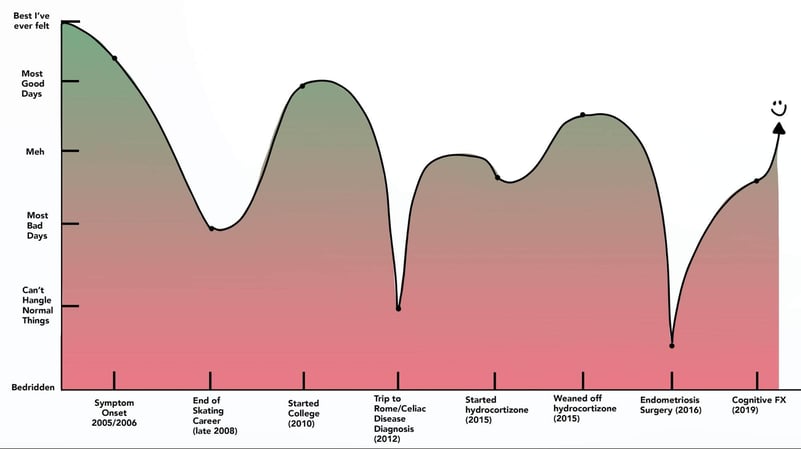
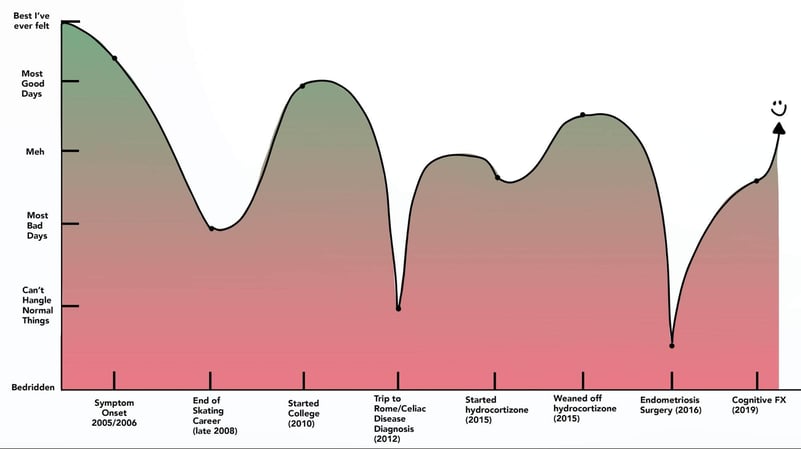 Rough health over time graph. Only producible in retrospect. :)
Rough health over time graph. Only producible in retrospect. :)
How I Discovered Cognitive FX
I attribute my recovery to divine intervention, because I never would have found Cognitive FX on my own.
In 2017, I started writing for a content marketing agency called Grow & Convert. In early 2019, they asked me to handle a new client — a concussion treatment clinic out in Utah. I thought it sounded interesting, and I’d done a smidge of neuroscience research during college, so it felt like a good fit.
Over the next few months, I got to interview their doctors and staff on topics such as what happens to your brain after multiple concussions and how neuroplasticity is key to post-concussion syndrome recovery. I also had the privilege of speaking to patients about their incredible recoveries, like how Myrthe is able to be a mom again, or how Sam is experiencing the world in a whole new way. I learned so much. And I also started recognizing similarities between their experiences and my own.
It wasn’t until I learned that concussions can cause symptoms during and after exercise (from autonomic nervous system [ANS] dysregulation) and hormone dysregulation that the light bulb flicked on.
I filled out a consultation request (OK, maybe I sat on it for a week internally arguing with myself on whether or not my situation was “severe enough” to warrant their attention) and waited for the date to arrive.
During the consultation, we went through my symptoms and medical history. Marci, their Director of Treatment, told me I sounded like a classic post-concussion syndrome case. Because I had come to know and love the people at the clinic, it was simple for me to say yes. I cried as we booked my treatment week for September 2019.
What Treatment for Post-Concussion Syndrome is Like at Cognitive FX

The fNCI Scan
When my husband and I flew out to Utah, the first order of business was to get a functional neurocognitive (fNCI) scan. I’d had two brain MRIs in the past, but they didn’t show anything wrong. Turns out, that’s because a regular MRI won’t show concussion dysfunction; an fNCI, which is a type of functional MRI, can show the difference — if you know what to look for.
fMRIs have been used to study the brain since the 1990s because they can show how your brain uses its resources. Cognitive FX created a unique testing and analysis methodology using fMRI to identify regional brain dysfunction caused by brain injury. Using this fNCI, they can tell you with a very high degree of certainty whether you have post-concussion syndrome. They can also tell you exactly which regions of your brain were affected.
During the scan, I used a set of buttons to answer test questions while they observed which regions of my brain activated, and how much. For example, I was shown a series of 3x3 grids with shapes of various colors and patterns. The task was to identify the one that was missing out of four possible answers.
After six different tests, they had collected the data they needed. When it was time to explain the results to me, they gave me a graph that summarized my overall condition, along with several pages breaking down what they found in different regions.
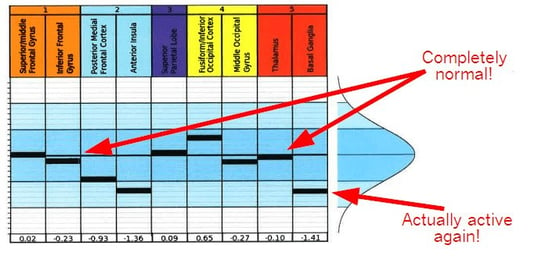
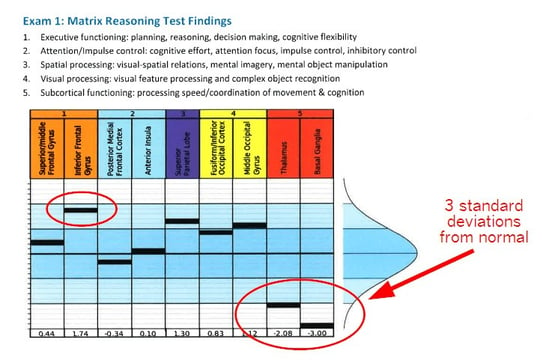 The fNCI showed that my thalamus was hypoactive and my basal ganglia was completely out to lunch. 3 standard deviations from normal basically means that there was no activation seen in that area on the fMRI. All the work was being routed around it — causing fatigue and stress on the rest of my brain. The inferior frontal gyrus was trending toward hyperactive (using too many resources for given tasks).
The fNCI showed that my thalamus was hypoactive and my basal ganglia was completely out to lunch. 3 standard deviations from normal basically means that there was no activation seen in that area on the fMRI. All the work was being routed around it — causing fatigue and stress on the rest of my brain. The inferior frontal gyrus was trending toward hyperactive (using too many resources for given tasks).
I cried (yes, again) while Marci explained what they found. Seeing those graphs re-opened old emotional wounds from my journey, but it also brought relief and closure.
Going through this process is part of what makes Cognitive FX different from many of the other treatment centers I could have tried. They know exactly which brain regions were affected in what way, so they adjusted my therapy regimen to target those specific areas.
Treatment Week: Time for a Brain Workout!
When you get a mild traumatic brain injury (the fancy term for concussion), the resulting inflammation and cellular damage can cause inefficient communication pathways in your brain. You can read more about that here.
Fortunately, our brains have the ability to repair that dysfunction (it’s called neuroplasticity), but they won’t always do it without the right motivation (a combination of exercise, for increased blood flow, and multisensory therapies to keep your brain’s pathways maxed out).
Treatment at Cognitive FX runs from Monday to Friday, although the most intense therapy happens on Tuesday through Thursday. You do cardio every day to get some blood moving through your brain, then follow that up with a combination of physical and cognitive exercises. The therapists are great about helping you manage symptoms during and after exercise.
I remember during one of the cognitive therapy tasks on Monday that I was told to listen to a series of words and tap the table whenever a pair of opposites showed up. In the background, the therapist put on a recording of a noisy restaurant. It took so much mental power for me to focus on the words that my peripheral vision went dark!
Therapy difficulty levels increased rapidly throughout the week. They wanted to keep pushing my brain to its limits so that it would look for more efficient ways to solve the problems I faced.
One of my favorite therapies was sensorimotor therapy (SMT). The therapist would give me sensors for my hands and feet and ask me to perform certain actions in time with a metronome. On Tuesday, I did a four-step pattern while playing Taboo.
On Wednesday, I struggled mightily with the new task. It was a five-step pattern: tap R leg, tap L knee, L step forward, tap L shoulder, R step forward. At the same time, I had to look at a chart of arrows and try to name the direction it was pointing without losing my place in the chart. I did okay at first, but once I made a mistake, it was a downward spiral of trying to get my rhythm back and struggling with distractions.
Another favorite therapy was Dynavision. It’s a board with concentric rings of lights that flicker on and off, either red or green, in a random pattern. The goal is to hit the lit-up buttons as fast as you can (which ones you need to hit depends on the game mode). I was slow at first, but once I got some practice in I made the monthly and all-time leaderboards. It was a blast.
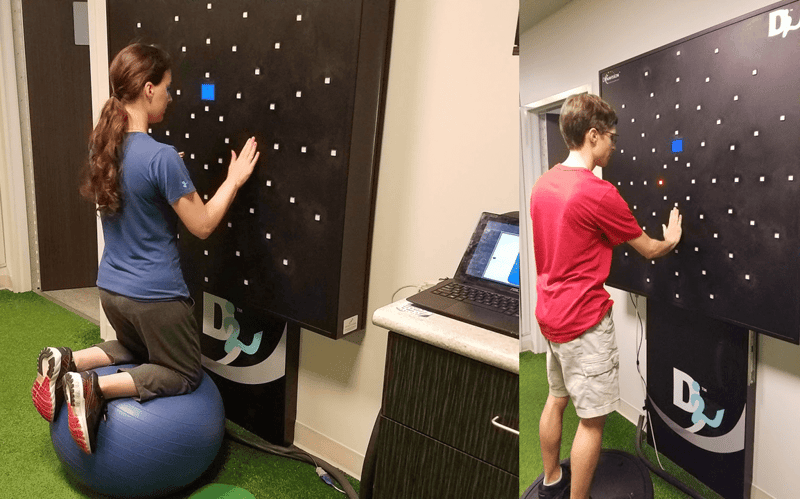 Left: Doing Dynavision with a special twist (don’t worry, most patients don’t do therapy while kneeling on an exercise ball!).
Left: Doing Dynavision with a special twist (don’t worry, most patients don’t do therapy while kneeling on an exercise ball!).
Right: My husband, Mark, tries Dynavision after my therapy finished for the day.
The exercises I did sound crazy, but they were exactly what my brain needed. Sensorimotor therapy challenged my basal ganglia and thalamus while encouraging the “left” and “right” sides of my brain to work together.
The Dynavision exercises we did were designed to help a host of visual, cognitive, and motor-related processes, including things like reaction time, peripheral vision, executive function, and balance. I have no doubt those exercises helped my thalamus wake up.
Early Signs of Change
Treatment week went by without many changes from my perspective, but I did notice a few. One of the more notable ones seemed like a negative at first.
I hadn’t experienced any major light sensitivity in recent years and had even forgotten what I experienced during my college years. But on Tuesday night after treatment, I was hit with the sudden onset of light sensitivity. Indoor lights felt piercing and grating. I made my husband, Mark, turn off all but one of the lights in the Airbnb we were renting!
It was a sign that my thalamus was starting to wake up and recalibrate after years of hypoactivity. I also started having carbon-copy dreams from my childhood that I hadn’t had in years (I don’t remember all the details, but one of them involved shooing bears and a leopard out of my childhood home with a broom).
As the week progressed, I kept having dreams from when I was younger, but they started to blend with the current people and events in my life (like having the fNCI tech, Brian, walk up and ask me how I was doing ... in the middle of a totally unrelated dream).
By the end of the week, I actually had some energy when I woke up in the morning. My sleep was getting more refreshing. So, I knew something had changed by Friday, but I didn’t know how much until they showed me the results of my second, end-of-week fNCI scan.
Getting the Results
All of the patients getting therapy that week came in on Friday morning with the same anticipatory air. Many patients talked about how they didn’t feel very different, so they weren’t confident their brains had changed. The first patient to get her results came into the lounge crying tears of joy. She had gone from over the red zone (very bad) and into the green (pretty good)!
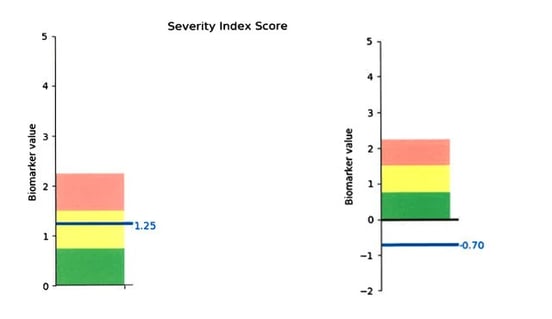
My improvement was significant, too. I couldn’t have asked for better results:
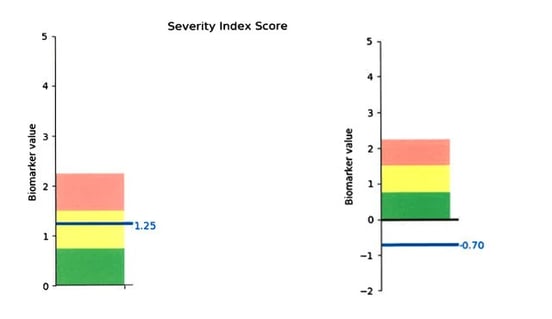
Overall results, before (on left) and after (on right). Zero is the “normal” average score determined by scanning healthy and efficient, functioning brains. The standard deviation is +/- 0.75, so a score of -0.7, while rare, is not unheard of. It just means that my brain function now looks very similar to their computer model.
And remember those initial scan results I showed you earlier? After treatment, my thalamus looked amazing (hence why I am starting to sleep better), my inferior frontal gyrus normalized, and my basal ganglia reactivated. That has made a huge difference in work distribution throughout my brain, resulting in overall fewer symptoms and higher energy levels.
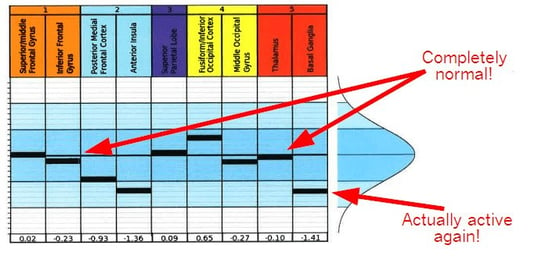
Since the scan is done after only a week, my brain is expected to continue to improve from there.
There is still work to be done, but my brain started using the pathways it’s supposed to use, and nothing (aside from another knock to the head) will make it revert back. This is because our brains prefer more efficient pathways to the less efficient pathways that can develop during injury.
Phase 2: Recovering at Home
It’s important to understand that treatment at Cognitive FX does not mean all your symptoms magically disappear at the end of the week (although I have heard of some patients who recovered immediately and have been fine since).
On Friday, they put together an at-home exercise plan for you to continue improving at home. Recommendations vary per person and involve some mix of the following:
- Sustained physical activity
- Cardio intervals
- Cognitive activities
- “Brainwaves” (10 min of rest in a dark room with soothing audio in the background)
 I’ve been doing that regimen fairly faithfully since treatment. I’ve also been attending vision therapy sessions every week to correct eye teaming issues and convergence excess (fancy terms for eyes that don’t want to work together the way they should). We discovered those problems because Cognitive FX referred me to Dr. Devin Duval, who is an expert in diagnosing and treating vision problems from concussions.
I’ve been doing that regimen fairly faithfully since treatment. I’ve also been attending vision therapy sessions every week to correct eye teaming issues and convergence excess (fancy terms for eyes that don’t want to work together the way they should). We discovered those problems because Cognitive FX referred me to Dr. Devin Duval, who is an expert in diagnosing and treating vision problems from concussions.
Recovery requires patience. Not every day feels amazing. It takes some time for your body to adjust to a newly efficient brain, and when you have ANS and hormonal dysregulation like I do, it takes even longer. But overall, I have made tremendous progress.
(Photo on right: From my first week back from Utah. My sweet, old cat Teva likes to help with brainwaves.)
Really Feeling the Change
The first time I realized that I really was getting better happened a couple of weeks after treatment. I got up early, did my therapy exercises, got in a normal (for me) workday, helped Mark cook a big pot of soup, then brought it over to my friend’s house on a whim and enjoyed his company.
Pre-treatment Olivia would not have had a day like that. Before treatment, I struggled to get up before 8am because I always felt horrible in the morning. I needed a nap during the day to get enough work done. And as for cooking dinner and exercising? Forget about it.
In fact, I’ve noticed a whole slew of positive changes in the last three months:
|
Before Treatment
|
After Treatment
|
- Had to get to bed by 10pm
- Had to sleep until 8am
- Woke up feeling exhausted
- Needed a nap (or at least to lie down) partway through the day
|
- Still have to go to bed by 10pm, but consequences for poor choices are less severe
- Get up at 6:30am every day and don’t need a nap
- Wake up feeling energized and able to handle a new day
|
- Basically worthless in the evening
- Doing stuff after work would cost me the next day
|
- Can run errands, cook, or do other activities without “paying for it” later
|
- Liable to become overwhelmed by small things (like abandoning a cooking project just because a pan I needed was dirty)
|
- Not easily overwhelmed; if something is standing in my way, I just handle it
|
- Hated crowded, noisy spaces
|
- Handled Thanksgiving celebrations with over 23 people (13 children under age 10 and over 10 adults) with ease. Instead of finding a quiet corner and staying there all evening, I helped prep food, chatted with multiple people at one time, didn’t get a headache, and had at least as much energy and enthusiasm as the others in attendance!
|
- Couldn’t even do light exercise without getting brain fog and attention difficulties for the rest of the day
- Couldn’t do heavy exercise without dizziness and nausea
|
- Can exercise and still get my work done afterward with little friction
|
The limitations placed on me by post-concussion syndrome are disappearing. I still have to respect my boundaries — I didn’t turn into a robot capable of working around the clock, and I can’t exercise as strenuously as someone who had never been injured (yet). But the quality of life increase from before to after is significant.
Advice for Readers
 Why yes, that is my husband in the reflection taking a million versions of this photo.
Why yes, that is my husband in the reflection taking a million versions of this photo.
Reflecting on my experiences, here are a few tips I would share with anyone who might have post-concussion syndrome.
- If you think you might have post-concussion syndrome, just sign up for a consultation. I hemmed and hawed because of self-doubt, but filling it out was actually eye-opening because the paperwork they send you forces you to think through your symptoms and history. Talking with the team at Cognitive FX about whether I would be a good fit for the program helped me make a good decision. If you’re not a fit for their treatment, they tell you.
- If you decide to go, bring someone who can help take care of you. Prepare whatever you can ahead of time so you can just focus on recovery. I made a meal plan in advance, and my husband cooked for me throughout the week. We stayed at a clean, spacious Airbnb that was the perfect quiet place to come back to. I let go of all my stressors and focused on doing whatever they wanted me to work on — and gave that all my attention. We ate super healthy and went to sleep at reasonable times. It’s worth giving yourself the best chance at recovery possible.
- Realize that how well you think you’re doing doesn’t necessarily match with what your brain is experiencing. Therapy is designed to keep getting harder so you feel like you’re never one step ahead of the game. Lots of patients get to the end of the week worried they didn’t get better when they objectively made amazing progress.
- Don’t get discouraged when you have a few bad days at home (and you will). It’s part of recovery — your brain and body need time to adjust.
Note:
I want to thank the amazing people at Cognitive FX who helped me on my recovery journey.
Dr. Fong, Dr. Allen, Jeff — you created a truly amazing place where so many suffering people find healing. Thank you!
Marci, you’ve been an immense help when I write my posts, and I’m so glad you were there to walk me through my own treatment experience. Shout-out to Dr. Loewen for all your help on breaking down complex topics as well!
Brian, you are such a sweet person. Thanks for encouraging me while I went through my scans and saying ‘Hi’ throughout the week.
To all the therapists who worked with me (including but not limited to Michelle, Nate, Paige, Amanda, Kaylie, Jacob, Wes, Alyssa, and Jordan, because I’m terrible at remembering names) — you guys rock. I have rarely felt more supported and encouraged than I did while you helped me through each exercise.
If you’re experiencing symptoms that won’t resolve after a concussion, you’re not alone. And you’re not crazy. 95% of patients at Cognitive FX experience statistically verified restoration of brain function. To see if you are eligible for treatment, schedule a consultation.
 Me doing a double lutz, double toe-loop combination during a competition in 2007, several years after hitting my head on the ice.
Me doing a double lutz, double toe-loop combination during a competition in 2007, several years after hitting my head on the ice.

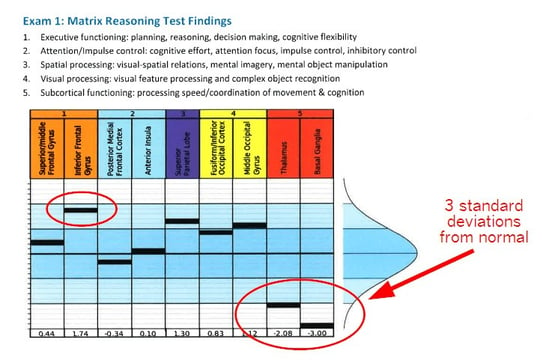 The fNCI showed that my thalamus was hypoactive and my basal ganglia was completely out to lunch. 3 standard deviations from normal basically means that there was no activation seen in that area on the fMRI. All the work was being routed around it — causing fatigue and stress on the rest of my brain. The inferior frontal gyrus was trending toward hyperactive (using too many resources for given tasks).
The fNCI showed that my thalamus was hypoactive and my basal ganglia was completely out to lunch. 3 standard deviations from normal basically means that there was no activation seen in that area on the fMRI. All the work was being routed around it — causing fatigue and stress on the rest of my brain. The inferior frontal gyrus was trending toward hyperactive (using too many resources for given tasks).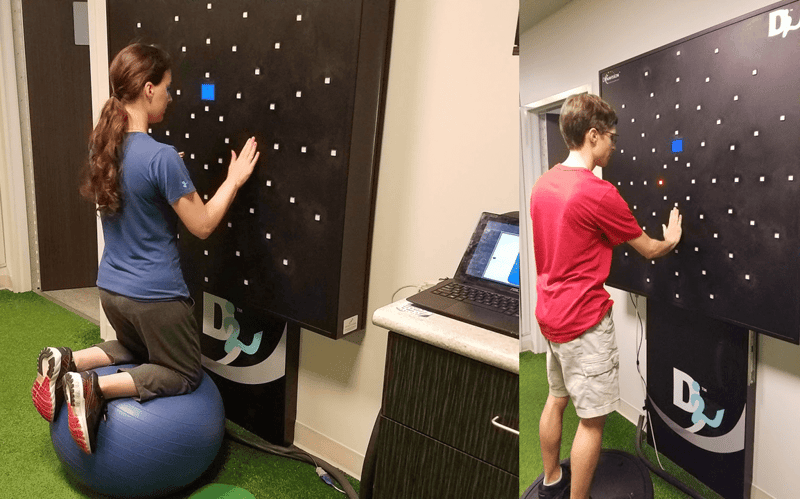
 I’ve been doing that regimen fairly faithfully since treatment. I’ve also been attending vision therapy sessions every week to correct eye teaming issues and convergence excess (fancy terms for eyes that don’t want to work together the way they should). We discovered those problems because Cognitive FX referred me to
I’ve been doing that regimen fairly faithfully since treatment. I’ve also been attending vision therapy sessions every week to correct eye teaming issues and convergence excess (fancy terms for eyes that don’t want to work together the way they should). We discovered those problems because Cognitive FX referred me to