Long COVID Fatigue: Causes, Duration & Treatment That Works 2025
You used to power through 10-hour workdays. Now you're exhausted after emptying the dishwasher.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Post-concussion syndrome (PCS) is a complex condition in which concussion symptoms persist for weeks, months, or even years after the initial head injury. While most people recover from a concussion within two to six weeks, approximately 15-30% of patients develop persistent symptoms that interfere with daily life, work, and relationships.
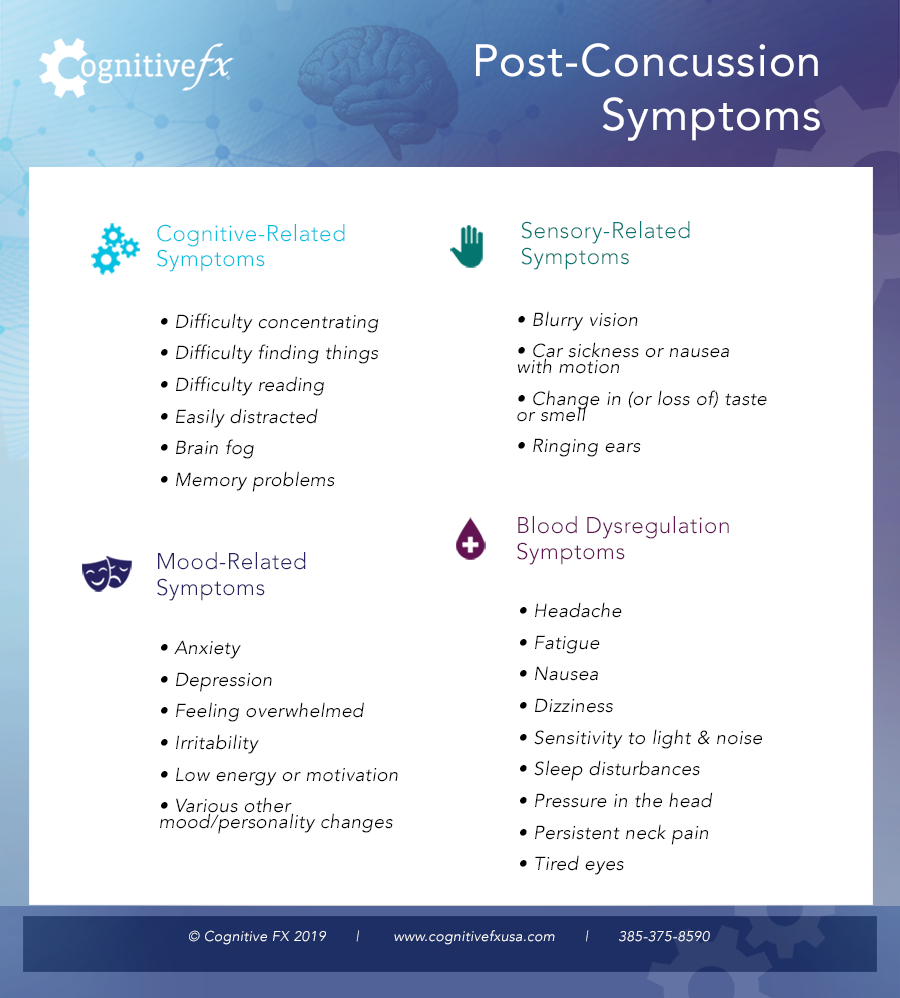
Common symptoms include chronic headaches, difficulty concentrating, memory problems, fatigue, dizziness, sleep disturbances, and emotional changes such as irritability or depression. These symptoms occur because the brain's neurovascular coupling becomes dysfunctional after injury, meaning affected brain regions don't receive the right amount of oxygen at the right time to function properly.
The good news: post-concussion syndrome is treatable. With proper diagnosis and targeted therapy, most patients experience significant improvement in their symptoms and quality of life.

Post-concussion syndrome, sometimes called persistent post-concussive symptoms (PPCS), is diagnosed when concussion symptoms continue for more than three months after a head injury. The condition can develop after any type of mild traumatic brain injury (mTBI), including sports-related concussions, car accidents, falls, or any event that causes the brain to move rapidly inside the skull.
You don't need to lose consciousness to develop PCS. Many patients never "blacked out" during their injury but still experience significant, lasting symptoms. Even seemingly minor bumps to the head or whiplash injuries can lead to post-concussion syndrome in some individuals.
Concussions are extremely common, with an estimated 1.6 to 4 million occurring annually in the United States. Studies suggest that 15-30% of concussion patients develop persistent symptoms lasting beyond the typical recovery window. However, researchers believe these numbers underestimate the true prevalence because many concussions go unreported or undiagnosed.
Post-concussion syndrome affects people of all ages, from children and adolescents to older adults. The condition can significantly impact work performance, academic achievement, relationships, and overall quality of life.
Post-concussion symptoms typically fall into three categories: physical, cognitive, and emotional. Most patients experience symptoms from multiple categories, and the specific combination varies from person to person.
Important: Your symptoms may change over time. Some initial symptoms may resolve while new ones emerge. Additionally, many post-concussion symptoms worsen each other. For example, poor sleep can intensify headaches, which can increase fatigue, which makes concentration harder. This interconnected nature of symptoms is one reason why comprehensive treatment approaches tend to be more effective than addressing symptoms individually.
Post-concussion syndrome can develop after a mild, moderate, or severe TBI. It can also come from brain traumas like carbon monoxide poisoning, transient ischemic attack (TIA), chemical exposure, certain viral or bacterial illnesses, surgery, and more.
Post-concussion symptoms stem primarily from dysfunctional neurovascular coupling (NVC), which is the dynamic relationship between neurons and the blood vessels that supply them. When you experience a concussion (or any TBI), your immune system causes inflammation near the site(s) of injury. The affected parts of your brain experience a temporary breakdown of tiny structures in and around those cells.
As a consequence, those cells don’t get the right amount of oxygen at the right time to power the signaling your brain normally does. When you try to do something that those cells govern — like encoding a new memory or paying attention to a conversation — they won’t be able to accomplish the task. Other neural pathways will then attempt to complete the process, even though it’s a less efficient path for that information to take.
The result of NVC dysfunction is these hypoactive brain regions that can’t do their fair share of the work. Other brain regions will try to take on more work than they should, but they can’t do so efficiently. This tires your brain out, leading to post-traumatic headaches, feeling overwhelmed, irritability, and other symptoms.
For the majority of people who suffer from a concussion, symptoms usually resolve 3-6 weeks post-head trauma. We assume that’s because the brain goes back to using the best pathways for any given process (although it may just be really good at compensating for the injury). But for post-concussion syndrome patients, the brain keeps using less efficient pathways to complete tasks even after the inflammation has resolved. That suboptimal signaling is what results in long-lasting concussion symptoms.
If suboptimal signaling seems confusing to you, think of it like road traffic. A healthy brain would distribute “traffic” — i.e., the signaling and blood flow dynamics needed for a task like reading — equally along existing pathways. Suboptimal signaling is like getting stuck in a traffic jam or taking a frontage road instead of the highway. It’s inefficient and requires more “gas” to get to the same destination.
The more your brain has to use suboptimal pathways, the more likely you are to experience symptoms.
A concussion may also result in...
These post-concussion complications can produce many of the long-lasting symptoms characteristic of post-concussion syndrome.
Post-concussion symptoms can last for weeks, months, or even years after the concussive event. In general, if your symptoms have not gone away after three months, it’s a good idea to explore treatment options.
Note: To be honest, we don't like the term "post-concussion syndrome." The word "syndrome" implies that we don't understand what causes post-concussion symptoms, when in reality, we do. And not only do we know what causes it, we can treat it, too. We'd love to see the language shift from "post-concussion syndrome," "postconcussional syndrome," and “postconcussive syndrome” to "post-concussion symptoms." But since many of our patients are familiar with the term "post-concussion syndrome," we've used it here as in years past.
Researchers don't fully understand why some people develop PCS while others recover quickly from identical injuries. However, several factors appear to increase your risk:
Having one or more risk factors doesn't mean you'll definitely develop PCS, and many people without any known risk factors still develop persistent symptoms. The important thing is to monitor your recovery and seek appropriate care if symptoms persist.
If you've experienced a head injury, it's important to know when to seek medical attention. Even mild concussions warrant evaluation, and certain symptoms require emergency care.

If your symptoms have persisted for three months or more, you likely have post-concussion syndrome and should consult with a healthcare provider who specializes in brain injury rehabilitation. Many primary care doctors and even some neurologists are unfamiliar with effective PCS treatments, so finding a specialist with experience in post-concussion care is important.
There is no single test that definitively diagnoses post-concussion syndrome. Instead, healthcare providers rely on a combination of clinical evaluation, symptom assessment, and various tests to rule out other conditions and confirm a PCS diagnosis.
Most healthcare providers diagnose PCS when a patient has experienced a head injury and continues to have multiple concussion-related symptoms for at least three months. The symptoms must significantly impact daily functioning and cannot be better explained by another condition.
Physical and Neurological Examination: Your doctor will assess your balance, coordination, reflexes, vision, and other neurological functions.
Symptom Questionnaires: Standardized assessments like the Post-Concussion Symptom Scale (PCSS) help quantify symptom severity.
Cognitive Testing: Neuropsychological tests evaluate memory, attention, processing speed, and other cognitive functions.
Balance and Vestibular Testing: Specialized tests can identify problems with your vestibular system that contribute to dizziness and balance issues.
Vision Testing: A neuro-optometric evaluation can detect visual processing problems common in PCS.
Standard CT scans and MRIs are useful for ruling out serious structural damage like bleeding or skull fractures, but they typically appear normal in PCS patients. This is because post-concussion syndrome involves functional problems with how brain regions communicate and process information, not visible structural damage to brain tissue.
Functional MRI (fMRI) can detect the neurovascular coupling dysfunction that underlies PCS. Unlike standard MRIs that show brain structure, functional MRI shows brain activity and blood flow patterns. At Cognitive FX, we use a specialized form of functional MRI called functional NeuroCognitive Imaging (fNCI) that identifies exactly which brain regions are affected and how severely, allowing us to create individualized treatment plans.
If you've been told your brain scans are "normal" but you're still experiencing symptoms, this doesn't mean your symptoms aren't real. It simply means that standard imaging isn't designed to detect the type of dysfunction present in post-concussion syndrome.
Post-concussion syndrome treatment has evolved significantly in recent years. While older approaches focused primarily on rest and symptom management with medications, current research supports active rehabilitation as the most effective approach for most patients.
Active rehabilitation combines controlled aerobic exercise with targeted therapies to help the brain restore normal function. This approach takes advantage of a phenomenon called the Post-Exercise Cognitive Boost (PECB): after aerobic activity, the brain releases neurotransmitters and proteins like brain-derived neurotrophic factor (BDNF) that enhance neuroplasticity and support healing.
Evidence-based therapies commonly used in PCS rehabilitation include:
While medications can help manage specific symptoms, they don't address the underlying neurovascular dysfunction causing PCS. Medications may be prescribed for headaches (pain relievers, anti-nausea drugs), sleep problems (melatonin, sleep aids), or emotional symptoms (antidepressants, anti-anxiety medications).
However, brain-injured patients are often more sensitive to medication side effects. Additionally, using pain medications during activities can mask warning signs that you're overexerting yourself, potentially prolonging recovery. For these reasons, many specialists recommend minimizing medication use and focusing on active rehabilitation when possible.
Certain lifestyle changes can support recovery and help manage symptoms:
At Cognitive FX, we developed EPIC (Enhanced Performance in Cognition) Treatment, an intensive, multidisciplinary rehabilitation program. Each patient receives a functional NeuroCognitive Imaging (fNCI) scan that identifies exactly which brain regions are affected. This information guides a personalized treatment plan combining aerobic exercise with targeted therapies.
In published research involving 270 patients, those who completed our program demonstrated an average 75% improvement in brain function as measured by fNCI scans. Patients also reported an average 62% improvement in self-reported symptoms, with many continuing to improve after returning home.
If you're interested in learning whether EPIC Treatment might be right for your situation, you can schedule a consultation with our team. We'll review your history and help determine the best path forward for your recovery.
Post-concussion syndrome is treatable, and most patients can achieve significant improvement with appropriate care. Without treatment, symptoms may persist indefinitely or even worsen over time. However, with the right intervention, recovery is possible regardless of how long you've been experiencing symptoms.
We've successfully treated patients whose injuries occurred more than a decade ago. The brain retains its capacity for healing and reorganization (neuroplasticity) throughout life, which is why it's never "too late" to seek treatment.
Recovery timelines vary significantly depending on the individual, the severity and complexity of their condition, and the type of treatment they receive. Some patients notice substantial improvement within weeks of starting targeted treatment, while others require several months of ongoing therapy.
Research shows that symptoms are more likely to worsen than resolve on their own over time. One study found that 72% of concussion patients had worsening symptoms after five years. This underscores the importance of seeking appropriate treatment rather than waiting for symptoms to resolve spontaneously.
Many patients come to us after unsuccessful treatment elsewhere. This often happens because post-concussion syndrome requires specialized expertise that not all healthcare providers possess. A treatment approach that works well for acute concussions may not be appropriate for persistent symptoms. Additionally, treatment must be tailored to each patient's specific brain function patterns to be maximally effective. If you haven't responded to previous treatment, it doesn't mean you can't recover; it may simply mean you haven't found the right approach yet.
Post-concussion syndrome can be permanent if you do not receive treatment, but often resolves or improves with the right therapy. It can be more difficult to treat for some people due to other underlying factors, including cervical spine problems, that contribute to the symptoms of PCS they are experiencing.
In one of our published research articles, we collected and analyzed data from 270 concussed patients. We were able to confirm the effectiveness of the fNCI-based and accelerated concussion treatment approach that we founded Cognitive FX on. (It was this research that inspired the founders to develop the clinic into the fully functional treatment center that it is today.)
Patients who underwent four days of EPIC Treatment demonstrated significant improvement in both objective and subjective data. On average, patients improved by 75% on the severity index score (severity of the dysregulation of blood flow in the brain). Of the 270 concussed patients, 62% percent of the patients reported an improvement in their post-concussion symptoms after those four treatment days. Many of our patients continue to report decreased symptoms and increased quality of life over time.
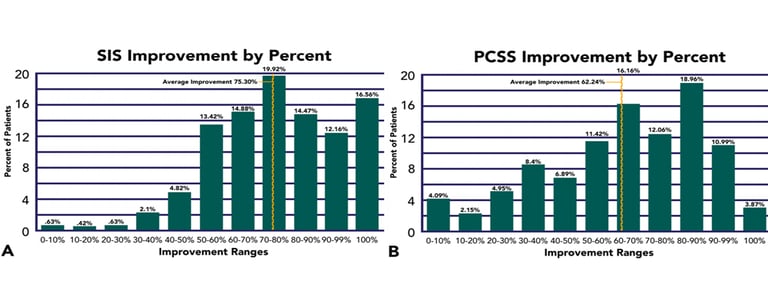
SIS stands for "Severity Index Score," which describes the severity of brain dysfunction as identified via an fNCI scan. PCSS stands for "post-concussion symptom scale." It describes self-reported symptom severity.
In our most recent research publication, we explain the fNCI (functional neurocognitive imaging, a type of functional MRI) that we use to “see” the dysfunctional brain regions of each patient. Using that information, we can develop a custom treatment program for our patients struggling with PCS.
This research shows how the treatment program we offer can target and repair the dysregulations found in post-concussion syndrome thanks to neuroplasticity (our brain’s natural ability to adapt and recover).
Further reading: How neuroplasticity treatment can help you recover from a brain injury
Note: To read the research papers mentioned above, visit our publications archive.
Multiple concussions will not necessarily cause post-concussion syndrome, but they are a risk factor for developing PCS. We do not know why some individuals develop PCS symptoms and others do not, but we do know that you have a chance of developing PCS after each concussion.
That said, a previous concussion is not a reliable indictor of whether you will develop post-concussion syndrome. Some other indicators are more reliable. For example, women and those with pre-existing depression have a higher risk of developing PCS regardless of concussion history.
Up to 30% of all concussion patients develop lasting post-concussion symptoms and sequelae to some degree — a much higher incidence than you might expect given the current lack of awareness in the medical community.
Further reading: The long-term effects of multiple concussions
We compiled a list of the most common emotional, physical, and cognitive symptoms of post-concussion syndrome reported by patients:
The symptoms from your initial injury may not be the same as the symptoms you experience over time. For example, you may find that initial confusion goes away, but exercise becomes increasingly difficult.
Your specific symptoms may vary from the norm, or they may be quite similar to what other patients experience. The good news is that it’s usually still treatable. As we work on patient education, we’ve developed resources to help patients understand specific post-concussion symptoms:
Concussions lead to emotional symptoms, too. Brain injuries can damage connections that go from the cerebral cortex (the part of the brain that has a role in memory, attention, perception, cognition, and awareness) to the limbic system (the part of the brain that supports functions such as emotions, behavior, and motivation). Changes in mental health are some of the most common symptoms of PCS.
A brain injury is emotionally traumatic as well as cognitively debilitating. People can respond with frustration, anger, anxiety, and depression to their changed capabilities and life circumstances. Even a mild head injury can lead to mental disorders like post traumatic stress disorder (PTSD).
Making matters worse, an injury affects how the brain interprets the information it receives and how it processes this information. This can make it difficult for someone to understand and express what they are feeling to others. Psychological factors can also increase the severity of other, non-emotional symptoms like sleep problems and headaches.
By the way, we created an online course that covers which types of headaches you can get after a concussion, as well as specific techniques for coping with those types of headaches. If you want to learn how to manage your headaches at home, visit our course.
We have written several guides for people struggling with mental health changes after injury:
Often, patients with emotional symptoms are given prescriptions for antidepressants, mood stabilizers, or other psychoactive drugs. A brain injury makes you more susceptible to negative side effects, so monitor your symptoms carefully. It is best to treat the brain injury with active therapy (something we’ll discuss below) and resolve any persisting mental health issues at a psychiatry practice. Your doctor can determine whether additional pharmaceutical intervention is necessary.
If you’re experiencing symptoms that won’t resolve after one or more concussions, you’re not alone. And you’re not crazy. On average, our patients improve by 75% after treatment at our center specializing in post-concussion therapy. To see if you are eligible for treatment, schedule a consultation.
Post-concussion symptoms can persist or recur years after the original injury. In general, PCS symptoms tend to stay the same or get worse over time until they are properly treated. Some patients also develop new symptoms due to complications from their condition.
In adults, as the brain ages, there is a natural decline in mental function. When you add a complication such as post-concussion symptoms onto this natural decline in function, the two cause a decrease in mental capability. History of concussion is also linked to structural and functional alterations in aging individuals, even in those that may present with “normal” neuropsychological performance.
In addition, post-concussion symptoms often feed into each other. For example, if you have migraines and trouble sleeping, the two will make each other worse over time. The concussion headaches can make it harder to sleep; the sleep disturbances (insomnia, waking up a lot at night, poor sleep quality, etc.) make you more likely to have headaches. And with those, other symptoms such as brain fog, fatigue, ability to focus, and so forth, can all get worse as well.
Patients often find themselves in a slow, downward spiral that they can’t escape without help. Not only does it take a severe toll on their quality of life, but it can also worsen any existing psychiatric disorders or emotional symptoms they experience. This is why it is so important to get the right diagnosis and treatment, especially if your concussion symptoms are worsening.
The good news is that we’ve detected no difference in recovery rates whether you’ve had post-concussion syndrome for just a year or over a decade. The brain is still capable of healing all those years later!
Further reading: Former figure skater finds relief after fourteen years of post-concussion syndrome and Businessman recovers from persistent symptoms 33 years after his brain injury

There is no one test available to prove you have post-concussion syndrome. Your doctor might want to order a scan of your brain to check for serious damage. A computerized tomography scan (CT scan) or magnetic resonance imaging (MRI) may be performed to detect structural brain abnormalities or damage to the bone. That said, these scans will not identify the presence of PCS. If you're experiencing dizziness, you could be referred to a medical professional who specializes in ear, nose, and throat complaints.
Your doctor may recommend a psychologist or licensed counselor if your symptoms include anxiety or if you're having problems with memory.
Fortunately, there are more tests for post-concussion syndrome than that. The fNCI we offer, various physical and neuropsychological testing, and symptom reporting can all be used in diagnosis.
Further reading: Post-concussion syndrome tests
In most cases, an MRI cannot detect post-concussion syndrome. An MRI uses magnets to look at protons (positively charged particles) in water. In regards to a brain scan, that means the image is of the soft tissue in your head.
An MRI doesn’t show the skull bones well, but it will show the structure of your brain because that’s where the water is. The protons in water respond to a magnetic field differently based on what kind of tissue they’re in. By using MRI technology, we can look at those differences to determine what kind of tissue is being observed and the shape of that tissue. Because of this, a regular MRI is powerful at detecting serious issues in the brain such as strokes, aneurysms, tumors, bleeding, and so forth.
Unlike structural damage caused by tumors or brain bleeds, mild traumatic brain injuries do not show up on standard brain imaging tests because the tissue is not damaged in an obvious way. Head trauma impacts the ability of neurons to signal for the right amount of blood to accomplish certain processes but does not impact the structure of the cells themselves.
To learn more about the difference between an MRI scan and an fNCI scan, read our post: Can an MRI Detect Post-Concussion Syndrome?
At this point, you may be wondering why fNCI is effective since it’s a type of MRI. fNCI is a type of functional MRI rather than a structural MRI. Functional MRI is designed specifically to show blood flow in an organ rather than the structural integrity of that organ. So, if you get a functional MRI of the brain, you can see which regions of the brain are calling for increased blood flow (generally indicative of increased activity).
By having patients complete the same set of tasks in the MRI machine, we can tell the difference between patients who have a healthy response to those tasks and those who don’t (post-concussion syndrome patients).
That information not only helps us diagnose PCS but also tailor treatment to the specific needs of each patient.

Typically, healthcare professionals will diagnose someone with post-concussion syndrome (PCS) when their symptoms last longer than three months and other potential causes for the symptoms have been observed but ruled out as the cause of the patient’s persistent symptoms.
At Cognitive FX, we look at several indicators, including...
With the second generation of fNCI, we’re able to assess 56 brain regions for neurovascular coupling dysfunction as mapped to 27 functional descriptions:
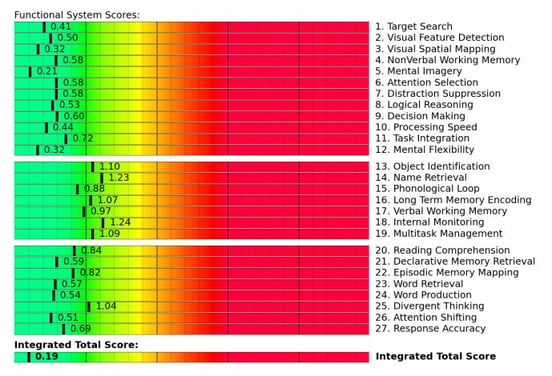 An example of second-generation fNCI results for a healthy patient.
An example of second-generation fNCI results for a healthy patient.
Note: While the fNCI is a key diagnostic tool, we also obtain a structural MRI of the brain and cervical spine for each patient. If we find any structural issues, we will refer you to a neurosurgery practice so you can get the help you need.
We use all of the data we collect to inform a personalized treatment plan that targets the specific physical and cognitive deficits you’re suffering from.
If you are diagnosed with post-concussion syndrome, what should you do next? The best treatment for post-concussion syndrome involves physical exercise and therapy from multiple disciplines. Some doctors try to manage PCS symptoms with medication, but this approach has serious downsides. There are also some natural remedies that can help, although they can’t fully treat the condition by themselves. We’ll share some resources regarding each in this section, along with where to find doctors who treat post-concussion syndrome.
Further reading: Post-concussion syndrome treatment options

At our post-concussion treatment clinic, we use a combination of exercise and multidisciplinary therapy. Our patients benefit from a phenomenon called the Post Exercise Cognitive Boost (PECB).
In short, aerobic activity brings on an increase of essential neurotransmitters and proteins in your brain that help develop and promote blood flow. One example is brain-derived neurotrophic factor, BDNF, which has been shown to increase post-exercise and help PCS patients in their recovery. Due to this increase, your brain is more able to perform complex cognitive challenges for longer periods of time.
Essentially, the PECB provides a window of time after exercise in which cognitive abilities are sharpened. Exercising consistently over time also has long-term benefits for your cognitive function.

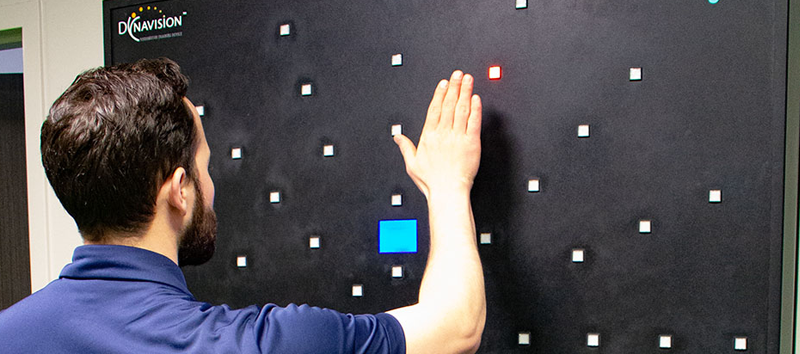
At our clinic, we combine the PECB with a range of multidisciplinary therapies, including neuromuscular therapy, occupational therapy, cognitive therapy, neurointegration therapy, sensorimotor therapy, vestibular therapy, dynavision, and more. Patients also have scheduled rest with Brainwaves and at least two sessions with a psychologist.
To learn more about our approach to neurorehabilitation for post-concussion symptoms, you can also visit our EPIC (Enhanced Performance in Cognition) Treatment page.
Medications often come with side effects and/or long-term consequences, especially for brain-injured patients. And unfortunately, many patients find that their medications are minimally effective — if at all. Plus, if you’re taking multiple medications to manage post-concussional symptoms, that puts extra strain on your liver. Sadly, they are also the main solution many doctors turn to for PCS patients.
Adolescents face unique challenges with medications because they can have more serious side effects (such as suicidal feelings while using antidepressants) and we don’t know the long-term effect of these medications on the developing brain.
Anything you can do to relieve or minimize symptoms without medication is usually better for your overall health.
Further reading: Medications for post-concussion syndrome symptoms
There are a few natural remedies we have seen our patients taking that you may find helpful as well:
Do not start or stop taking supplements without consulting your doctor.
We have another post that takes a comprehensive look at natural remedies for post-concussion syndrome, including approaches like acupuncture, physical activity, diet, tea, and more.
We understand that you may not be able to travel to our office in Provo, Utah for post-concussion syndrome therapy. Instead, you may want to see what your options are for clinics in your local area.
Because we want to help you make an informed decision about your health care options, we have created a blog explaining how to find the best concussion clinics in the United States. The blog post answers questions such as “Do I need to go to a concussion clinic,” “What types of services does a clinic offer,” and “How can you tell if a concussion clinic is good or not?”
Further reading: How to Find the Best Concussion Clinics Near You
There are many types of doctors you could visit for post-concussion medical care, including family physicians/pediatricians, sports medicine practitioners, emergency department doctors, neurologists, neuroradiologists, neuropsychologists, physical medicine and rehabilitation (PM&R) physicians (physiatrists), endocrinologists, and more.
Further reading: Types of head injury doctors
Keep in mind that not all health care providers are capable of treating PCS well:
Do your research and don’t be afraid to ask questions or find a new doctor if the one you’re seeing isn’t getting results.
If you haven’t yet had testing for hormone imbalances, you can ask your primary care doctor, OB/GYN, or endocrinologist to run some tests based on your symptoms. For more information, including questions to ask your doctor, read our article: How to talk to your doctor about hormone imbalance.
Sometimes, clinicians and researchers use the phrase “persistent post-concussion syndrome” to describe what patients experience when their post-concussion symptoms aren’t going away. But since most post-concussion syndrome cases don’t go away without treatment, we treat the terms as synonymous.
That being said, we’ve spoken with plenty of patients who were frustrated because they didn’t get better after treatment by other doctors or at other clinics. In that sense, their PCS really is persistent — symptoms remained even after treatment.
One of our patients, Sam Pembleton, tried all of the concussion clinics she could get to in Ontario with no luck. She even flew to a clinic in Boston, and they sent her home because she wasn’t responding to treatment. She suffered through five years of persistent post-concussion symptoms before she came to Cognitive FX. After treatment at our clinic, she was able to work and finish school, go out with friends, and simply enjoy life again.
One of our other patients, Myrthe van Boon, was told by her doctors that she would never recover from her skiing head injury. After treatment, her quality of life improved rapidly; she felt like she could finally be present in her daughters’ lives the way she’d dreamed.
So how can you go through treatment at multiple facilities and still not recover from PCS? As it turns out, most cases of post-concussion syndrome are treatable, but not all patients respond well to one specific treatment protocol. Post-concussion syndrome is not one-size-fits-all. The brain regions affected by your brain injury are likely not the same as the regions that were damaged in someone else.
But most treatment programs don’t take these differences into account, in part because they often don’t have the ability to determine precisely how and where the patient experienced neurotrauma. Making matters worse, not all doctors have the same familiarity with traumatic brain injuries and how best to treat them.
As a result, some patients are only given medication or maybe some occupational therapy to help them adjust to life with symptoms. Others are given therapy — some of which can be truly excellent — but not at the right pace or intensity for neuroplasticity to kick in. Others may provide perfectly good regimens that simply aren’t tailored enough to the needs of the patient.
That’s why providing each patient with an fNCI scan is so important to our work. It tells us which brain regions were affected, and in what way, which in turn lets us know exactly what kind of treatment to provide. And that’s why patients like Sam and Myrthe, who tried many different doctors, were able to make progress under our care but not elsewhere.
If you’re experiencing symptoms that won’t resolve after one or more concussions, you’re not alone. And you’re not crazy. On average, our patients improve by 75% after treatment at our center specializing in post-concussion therapy. To see if you are eligible for treatment, schedule a consultation.
Many studies have found that PCS recovery time varies drastically. Some patients recover after a couple of weeks without any long-term side effects; others struggle with symptoms for the rest of their lives. Some studies even go as far to state that “PCS may be permanent if recovery has not occurred by 3 years” (DOI: 10.1089/neu.2016.4677).
A recent study found that only 27% of post-concussion syndrome patients meeting diagnostic criteria at three months post-injury made a full recovery. The article "Early Clinical Predictors of 5-Year Outcome After Concussive Blast Traumatic Brain Injury" states that many concussion patients experience the evolution of symptoms five years after mild TBI, not the resolution of symptoms. 72% of patients had worsening symptoms after five years. Their findings indicate that concussion symptom prevalence is likely to increase over time, rather than resolve. This can leave PCS sufferers with little or no hope of recovery.
What we’ve found is that it doesn’t matter how old your injury was: The key to recovery is getting the right treatment.
On average, our patients report a 60% improvement in their symptoms in one week. We also performed follow-up research using fNCI scans on 28 previous EPIC patients approximately one year post-EPIC treatment. The average amount of time between the completion of EPIC and the follow-up fNCI was 329 days. We found that patient’s scores, on average, continue to improve — indicating that EPIC Treatment makes permanent changes in the brain to regulate neurovascular coupling and restore healthy brain function.
Further reading: Recovering from post-concussion syndrome and How to tell the difference between post-concussion syndrome, chronic traumatic encephalopathy (CTE) and sudden impact syndrome (SIS)

It’s one thing to learn about the neuroscience behind EPIC Treatment (the program we offer), but we understand that it’s important to hear about real recovery stories, too. In addition to filmed testimonials, we have posts about several patients who wanted to share their recovery stories. We’ll keep adding more stories to our blog, but in the meantime, you can catch up on these stories:
If you've been experiencing concussion symptoms that haven't resolved, you're not alone, and you're not imagining things. Post-concussion syndrome is a real medical condition with real treatments that work.
At Cognitive FX, we've treated hundreds of patients who thought they would never feel normal again. Our research shows that 77% of patients experience significant improvement after treatment at our clinic. We're the only post-concussion treatment center with third-party validated outcomes.
Want to know if EPIC Treatment is right for you? Schedule a consultation. We would be happy to discuss what options are available to you as a PCS patient.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

You used to power through 10-hour workdays. Now you're exhausted after emptying the dishwasher.
In post-concussion syndrome (PCS), a patient with a mild traumatic brain injury (mTBI) experiences persistent symptoms from the injury. If left untreated, the symptoms might last months, years, or...

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
Living with the lingering symptoms of a concussion for months or even years is life-changing. Patients with post-concussion syndrome (PCS) can feel worthless, misunderstood, lonely, and frustrated....

“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:

If you’ve suffered a concussion, you may have already encountered the Post-Concussion Symptom Scale (PCSS). This self-report questionnaire is one of the most widely used tools for documenting...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY