If you’re searching for answers and think you might have post-concussion syndrome (PCS), the path to diagnosis can be challenging. Few medical professionals are experts on the condition, and many lack the most sophisticated diagnostic tools. Many doctors will make a diagnosis based on concussion symptom history and a quick physical examination. Others will supplement their findings with imaging or computerized testing.
At Cognitive FX, we exclusively test for and treat conditions stemming from mild traumatic brain injury (mTBI). Our patients often show concussion damage to multiple regions of the brain, and many also suffer from autonomic nervous system (ANS) dysregulation.
We understand that obtaining a post-concussion syndrome diagnosis can be both stressful and a relief, all at the same time. Many patients have been to more than one doctor before getting their diagnosis. To make the process a little easier, we’ve put together a post that explains what methods are in use today to diagnose PCS, what their strengths and weaknesses are, and how the best testing methods enable you to get better treatment.
If you’re looking for something specific, you can use these links to navigate the post:
If you’re experiencing symptoms that won’t resolve after a concussion, you’re not alone. And you’re not crazy. 90% of our patients show symptom improvement after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation with our team.
Ruling Out Other Causes (Why PCS Tests Are Necessary)
In order to receive a post-concussion syndrome diagnosis, you must have had a precipitating event — meaning you must have experienced some kind of head trauma, be it physical impact, whiplash, or heavy jostling. Were you in a car accident? Did you fall and hit your head? Did you have a bad experience on an amusement park ride?
Most PCS patients can point to a specific incident that caused their symptoms. Others may have had a series of previous concussions (which is actually one of the risk factors for developing PCS). However, it’s important to note that loss of consciousness at the time of injury is NOT required for a concussion to occur. Many people mistakenly believe that their head injury couldn’t be a concussion because they didn’t lose consciousness. In reality, 90% or more of concussion patients do not experience a loss of consciousness.
On the other hand, if you are experiencing some symptoms of PCS but did not have head trauma of some kind, it is unlikely that PCS is the cause. That said, there are certain ways to injure your brain aside from traumatic brain injury. Some of the patients we’ve successfully diagnosed and treated suffered persisting symptoms from carbon monoxide poisoning, "chemo brain", bacterial and viral encephalitis, COVID-19, and transient ischemic attack.
Your doctor will need to know your medical history to make a PCS diagnosis and treatment plan. Some common symptoms of concussion can be caused by other conditions, and sometimes patients have post-concussion syndrome plus other difficulties. Patients might develop post-concussion depression and anxiety after their injury, or those conditions may have been pre-existing.
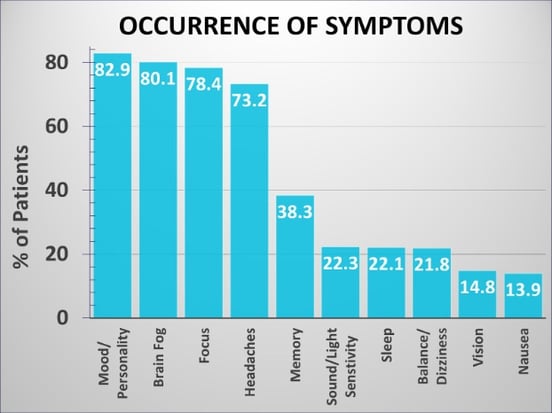
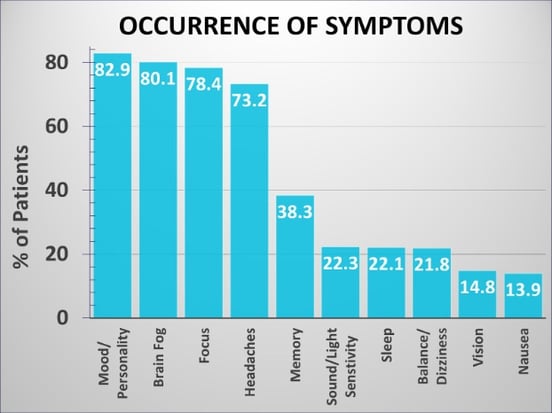
Nearly 83% of patients who come to us report mood or personality changes from post-concussion syndrome. It’s very easy for them to see a mental health professional first and completely miss the PCS diagnosis. But doctors also have to make sure that PCS — and not an underlying issue — is at the heart of those changes.
You can help your provider by making clear distinctions between symptoms you experienced before the traumatic event vs. after the injury. This can affect the outcome of your treatment, so it’s important to provide any information your physician requires to the best of your ability.
Types of Doctors Involved in Post-Concussion Syndrome Testing
Some types of doctors are better suited for diagnosing post-concussion syndrome than others. You can read more about head injury doctors here, but we’ll summarize some key points below:
- Many patients’ first thought is to visit their primary care doctor (or for adolescents, their pediatric doctor). While primary care doctors can coordinate testing and bloodwork, they are often not trained extensively in diagnosing and treating post-concussion syndrome. To find the right care and a clear diagnosis, you need to find a concussion specialist.
- If you visit a neurology practice, your neurologist may or may not be well equipped to diagnose PCS. In fact, in a 2017 survey of 289 neurologists revealed that the majority of neurologists who responded didn’t believe effective treatment was available for post-concussion syndrome. They are more likely to prescribe medications to alleviate certain PCS symptoms, such as post-traumatic headaches, than to address the root issue.
Further read: What Can a Neurologist Do for Post Concussion Syndrome?
- You might need more than one doctor to contribute to the diagnosis. A neuro-optometrist can diagnose post-concussion vision problems, for example. An appropriately trained sports medicine physician or physical therapist can diagnose vestibular dysfunction related to the concussion and provide vestibular therapy for PCS. A good endocrinologist can check your post-concussion hormone levels and provide appropriate therapy if they’re out of the healthy range.
Your best option is to find a clinic like Cognitive FX which specializes in the diagnosis and treatment of post-concussion syndrome. Our interdisciplinary team includes a clinical neuropsychologist, a neurosurgeon, a neuroradiologist, neuroscientists, clinical psychologists, neuromuscular therapists, cognitive therapists, occupational therapists, and others. We also have good relationships with local providers of vision therapy, hormone testing, and more. Click here if you want to discuss your symptoms with our team.
Note: If you visit a neurology or a psychiatry practice to address mental health symptoms after a concussion, exercise great caution. Many of them recommend antidepressants and strong headache medicines even though these medications are poorly tolerated by head injury patients and may make your symptoms worse overall. To learn more about treatment options for mental health changes after a concussion, please see our other posts on the topic:
Five of the Most Common Post-Concussion Syndrome Tests
In this section, we cover five common diagnostic methods: the SCAT5, CT scans, MRI scans, qEEGs, and baseline testing. We’ll also highlight and explain which practices we think are best.
SCAT5 and Self-Reported Concussion Symptoms
 Most doctors do not have advanced equipment at their disposal, so they rely on clinical expertise, the patient’s description of symptoms, and an in-person examination to make their diagnosis.
Most doctors do not have advanced equipment at their disposal, so they rely on clinical expertise, the patient’s description of symptoms, and an in-person examination to make their diagnosis.
A common way to do this is to use the SCAT5, short for Sport Concussion Assessment Tool 5. But that doesn’t mean it can’t be used on non-sport-related concussions. It can be used to diagnose any mild traumatic brain injury. The SCAT5 is primarily used to diagnose the initial injury but may be used to help with a post-concussion syndrome diagnosis as well.
The Post-Concussion Symptoms Scale
The test begins with a PCSS, or Post-Concussion Symptoms Scale. The patient rates his or her symptoms on a scale from 0 to 6, where six is the most severe. The symptoms you can report on this questionnaire include:
For the majority of concussion patients, these symptoms go away in six weeks or less. But for those with post-concussion syndrome, persistent symptoms become the norm. Most of the time, post-concussive symptoms that do not disappear within three months will not go away without treatment.
If you think you have post-concussion syndrome, this article covers all the basics of post-concussion syndrome, including diagnosis, treatment, patient stories, and more.Patients often have a mix of physical and cognitive symptoms. You may have balance and memory problems, along with chronic pain from headaches. Another person might have nausea and dizziness every time they work out, plus a general feeling of fogginess when they try to work.
That’s because PCS doesn’t look exactly the same in each person; different regions of the brain may be affected in different ways. Treatment of post-concussion syndrome is most effective when it takes those differences into account (more on that later).
Physical Evaluation
After determining patient symptoms, the SCAT2 has several sections that look at physical symptoms.
The test looks at physical information such as:
- Reflex response
- Vision tracking
- State of consciousness (if administered immediately after head trauma)
- Balance
- Hand-eye coordination.
The test also gives healthcare professionals guidelines as to how the patient should perform if concussed or not concussed.
Cognitive Evaluation
The SCAT5 has questions that look for cognitive impairment. It isn’t in-depth and is meant to be a quick assessment of things such as difficulty focusing or remembering. It covers abilities such as remembering what the month and day is, remembering a group of words and numbers (immediate recall), and then later in the test, remembering the words again (delayed recall).
Overall Usefulness of SCAT5
The SCAT5 was designed for use soon after a concussion. Unfortunately, that means it is not well-optimized for someone who has been experiencing post-concussion symptoms for a long period of time. That said, the PCSS (self-reported symptom scale discussed above) is a good starting point for any diagnosis effort.
CT Scans for Post-Concussion Syndrome
Doctors may order a CT Scan when a traumatic brain injury (TBI) is suspected. CT (or Computerized Tomography) scans are used to take 2D images of bones and organs that can be collated to produce 3D images. A CT machine uses X-rays that are rendered in a specific way by the computer.
CT scans by themselves cannot diagnose a concussion, but they can rule out other causes of your symptoms. For example, let’s say you were a backseat passenger in a car accident and your head slammed into the side of the car. If you suffered a skull fracture or your brain was bleeding from the impact, a CT scan would detect that. Or if you’ve experiencing PCS-like symptoms but don’t remember having brain trauma, a CT scan might reveal that you have a brain tumor causing those symptoms.
Because concussion symptoms don’t come from the kind of structural damage that a CT scan can detect, a CT scan cannot positively diagnose PCS. But it can rule out major injuries like the ones described above.
A major downside to CT scans is radiation exposure. Patients are often given a liquid called “contrast” that is used to help technicians get a better image. If you’re concerned about radiation from a CT scan, talk to your doctor about risks vs. benefits and whether or not there are alternatives to get the information they need.
MRI Scans for Post-Concussion Syndrome
It’s not uncommon for a concussion patient to wind up in the emergency department, waiting for an MRI (short for “magnetic resonance imaging”). And in some situations, getting an MRI makes sense (for example, if the treating physician wants to check for internal bleeding).
An MRI shows soft tissue, so it can confirm whether or not your brain is intact. It doesn’t show bone well, so it’s not a great diagnostic option if you think you fractured your skull, for example. Regular MRI scans are powerful diagnostic tools for serious issues such as strokes, aneurysms, tumors, bleeding in the brain, and so forth. Plus, they don’t come with any radiation risk.
Most of the time, a regular, structural MRI cannot detect post-concussion syndrome. But functional neurocognitive imaging (fNCI), which is a special type of MRI, can detect brain damage sustained from a mild TBI.
We’ve written at length in another post why MRIs aren’t good enough for a PCS diagnosis and why fNCI works. In short, fNCI is able to look at whether each region of the brain is using its resources (primarily oxygen) in a normal, efficient way.

The ability to pinpoint neuronal communication problems is very important for our patients' recoveries. In our research, we’ve collected thousands of both healthy and PCS-patient brain scans. Using this database, we’ve calculated what “normal” is for most patients. From there, we can see which regions of your brain are behaving the way they should — and which will need attention. Our team can use that information to tailor each patient’s treatment plan accordingly.
Note: If you think you have post-concussion syndrome, schedule a consultation with our staff. They can help you understand if PCS is a likely cause of your symptoms and determine if an fNCI scan is the right next step for you.
Quantitative EEG for Post-Concussion Syndrome

Some treatment facilities use a quantitative EEG (qEEG) to make PCS diagnoses. EEGs detect electrical activity coming from your brain (more specifically, from your neurons). Normal brains usually have certain patterns that injured brains may deviate from. qEEG is sometimes a helpful test, and sometimes not. Here’s why.
With any EEG, one of the main difficulties to overcome is noise. Since the electrodes sit on the patient’s scalp, they’re often placed over hair, which can interfere with the quality of the measurement. But even if you use qEEG on a bald patient, it won’t be able to evaluate the brain completely accurately.
Why? The electrodes detect too much signal from the surface and just below the surface of the brain. That makes it extremely difficult, if not impossible, to distinguish where the signal is coming from. So if concussion damage is affecting neurons deep within your skull, a qEEG probably can’t tell you whether there’s anything wrong with them. If the damage is closer to the skull, you may have better information.
Information gleaned from qEEG can support a PCS diagnosis. Unfortunately, that’s the extent of its helpfulness:A qEEG can sometimes indicate a problem, but not what that problem is, where the problem is, or how it is best resolved.
Baseline Testing for Concussion
Some people — particularly athletes — will take a baseline test to assess their pre-injury cognitive abilities. A baseline test is often just a cognitive assessment (usually computerized) designed to establish the normal cognitive ability for a particular person. Some tests also include visual and balance/physical testing as well, making them more useful. If you take a baseline test and then sustain a concussion, taking the same test may reveal cognitive deficits caused by the head injury.
Sometimes, this information is helpful. If you show a decrease in attention span, memory, and conversation tracking that persists beyond a few weeks, then the test is something you can use to prove the effect your concussion had.

Unfortunately, baseline testing also has its limitations. It’s not uncommon for athletes to sandbag the test (i.e., intentionally doing poorly on the initial test so that they will be quickly approved to return to play after a future concussion, should they sustain one). In addition, baseline tests are not always administered in a consistent manner. If they are administered differently, then a change in results can’t be exclusively attributed to the concussion. Finally, a baseline test is only helpful if you took one before your head injury — something many people don’t bother to do.
While baseline tests are popular in sports medicine, their contribution to a post-concussion syndrome diagnosis is limited.
How We Test for and Treat Post-Concussion Syndrome
At Cognitive FX, we diagnose post-concussion syndrome with a combination of imaging, physical tests, cognitive tests, and self-reported symptoms.
Post-Concussion Symptom Scale (PCSS)
We use information from the PCSS to get a quick idea of how much symptoms are impacting the patient in their everyday lives. We also ask them about other symptoms and have a conversation about what they’ve experienced. We review their medical history and make sure PCS seems like a reasonable explanation for what they’re facing.
Physical Tests
We also have patients perform some quick physical maneuvers to check their balance, reflexes, vision, and so forth. For example, you might have to balance on one foot with the other leg bent while your eyes are closed. Your clinician will be observing you to see what difficulties, if any, you have with the task. For vision, we might hold out two fingers and have patients track the movement with their eyes only. Many patients will become dizzy from that exercise! We also strongly encourage patients to get a full vision evaluation from Dr. Devin Duval, whose practice is close to our clinic.
Cognitive Tests
These form the minority of the testing we do, in part because the cognitive effects of PCS can vary so much from person to person. For one person, even basic logic exercises and reading could be extremely difficult. For another, complex thinking is within reach — for a short time, before they exhaust themselves.These issues are better described by the patient than evaluated with neuropsychological tests during a diagnostic visit.
Functional Neurocognitive Imaging (fNCI)
For every patient who pursues treatment at our clinic, we take one “before” and one “after” fNCI scan. Doing so accomplishes several goals:
- It is an excellent method to confirm diagnosis of PCS by clearly identifying abnormalities in blood flow throughout the brain.
- It shows us exactly which regions of your brain were affected by a head injury (so we can tailor treatment to your specific needs).
- It allows us to quantify your improvement after treatment.
The scan gives us an insider look at how your head injury affected communication in 56 regions of your brain. We then use targeted physical and cognitive therapy paired with aerobic exercise to encourage neuroplasticity. This treatment pushes the brain to establish (or re-establish) more efficient communication pathways that resolve or greatly lessen PCS symptoms. You can read more about our clinic’s post-concussion neurorehabilitation program and why it works here.
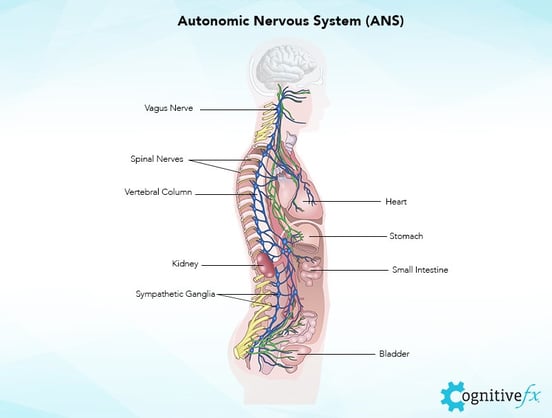
What About the Autonomic Nervous System?
The autonomic nervous system (ANS) controls all the processes you don’t think about: breathing, heart rate, blood pressure, vascular (blood vessel) constriction and dilation, your fight or flight response, and more. It’s a bit like your body’s operating system: It’s behind the scenes, making sure things are working the way they’re supposed to.
Many patients don’t realize that, after a concussion, your ANS may become dysregulated. As you can imagine, having an autonomic nervous system that’s “off” can lead to a variety of common symptoms.
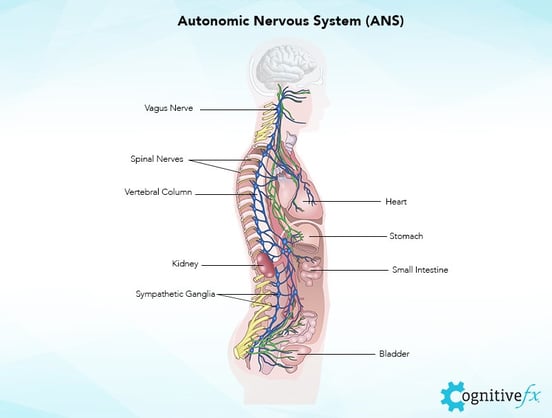
If you’ve ever had a pressure headache that made you feel like your head was swelling up like a balloon, or gotten really dizzy or nauseated after exercise, or been agitated for a long time after a small scare, then you’ve probably experienced what it’s like to have your ANS thrown off by a concussion.
But because the ANS is a system spread throughout your body, it doesn’t show up on normal post-concussion syndrome tests. Unfortunately, there aren’t many options for objective testing of ANS function. However, an experienced concussion specialist can work with you to discuss your symptoms and determine if your autonomic nervous system was affected by your concussion(s).
When we treat patients at our clinic, we build in therapy for the ANS as well as for the brain so we can rehabilitate both. ANS recovery can vary a lot for each patient; at the moment, there is no “standard” recovery time. You can learn more about ANS dysfunction (dysautonomia) symptoms and recovery options here.
Do You Have Post-Concussion Syndrome?
If you...
- Have had some kind of brain trauma (be it a blow to the head, heavy jostling, or whiplash), and
- Experience symptoms in multiple SCAT2 categories
...then there is a good chance you have post-concussion syndrome. However, it is not possible to know for sure without consulting a medical professional who has experience with post-concussion syndrome. (Note: Many general practice health care providers, sports medicine doctors, and even neurologists do not have the experience or knowledge needed to diagnose and treat PCS effectively — find someone with a proven track record and clear specialization in the field.)
If you’re experiencing symptoms after a concussion, you’re not crazy. Post-concussion syndrome is a real condition that has real solutions. It does not have to be permanent. If you think you may have post-concussion syndrome, schedule a consultation with our staff. They will help you understand your diagnosis and treatment options.

 Most doctors do not have advanced equipment at their disposal, so they rely on clinical expertise, the patient’s description of symptoms, and an in-person examination to make their diagnosis.
Most doctors do not have advanced equipment at their disposal, so they rely on clinical expertise, the patient’s description of symptoms, and an in-person examination to make their diagnosis.