Sleep Problems After a TBI: Causes & Treatment
Sleep disturbances are a common yet often overlooked consequence of traumatic brain injuries (TBI). Many patients struggle with insomnia — having trouble falling asleep or waking up frequently during...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
When you get a concussion, you may worry about when it’s safe to sleep. You might even have a friend or a family member wake you up every few hours. And while that is sometimes necessary (if you have a severe injury and have not yet received medical attention), most of the time, it’s better to sleep as much as you can while you heal.
But that’s easier said than done: Many patients experience post-concussion sleep problems. Some patients experience hypersomnia — in which they sleep far more than normal and may be extra drowsy after a head injury. Others experience insomnia — in which they have difficulty falling asleep or staying asleep.
Even worse, post-concussion symptoms may not simply go away with time and rest (if that happens, it’s known as post-concussion syndrome, or PCS). If you sustained a mild traumatic brain injury (or even a traumatic brain injury) and find that you can’t sleep the way you did before your injury, you’re not alone.
Soon after injury, around 30% of people report insomnia symptoms. Weeks to months later, 36% of people who have experienced a brain injury show circadian rhythm shifts, 30-70% show continued sleep disruption, and 43-73% of these people report fatigue (Mosti, Spiers, & Kloss 2016).
Sleep disturbances can be part of a vicious cycle that causes your symptoms to worsen over time. So how do you find some relief? Is there a concussion treatment that improves sleep quality? And why is this happening to you in the first place?
We aim to answer those and other commonly asked questions about post-concussion syndrome sleep and recovery in this post. Here’s a cheat sheet to what we’ll cover:
Note: If you've experienced one or more concussions and symptoms such as sleep issues persist, you're not alone — and help is available. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, schedule a consultation.
Most post-concussion syndrome sleep disorders can be bucketed under the following issues:
Hypersomnia and insomnia are actually related to the same brain system but are opposite expressions of the same problem. These two symptoms are by far the most common out of the five we’ll cover here. The other three are less common, and their disease etiology (meaning how and why they happen post-injury) has not yet been established. Nevertheless, we’ll explain each as best we can.

Post-concussion patients with hypersomnia:
Of the patients we see at Cognitive FX who experience hypersomnia, many are sleeping 12+ hours per day. That might mean sleeping eight hours at night plus extra naps during the day, or it could mean the reverse — only a few hours of sleep at night and many long naps during the day.
Despite all this sleep, patients with hypersomnia always feel tired. The extra sleep helps them get a bit further through their day but ultimately does not provide enough recuperation for them to function well and feel OK without napping. Many decide that it’s better to nap and get a few productive hours in rather than put up with overwhelming fatigue all day. Some patients experience excessive daytime sleepiness that effectively forces them to nap.
These patients might describe this as feeling like a phone that won’t charge past 50% — they have a lower amount of time they can function before going back to sleep. And when they are awake, they’re never as rested as they should be.
We’ve also noticed that some of our patients with hypersomnia don’t dream at night. This may indicate that, in their sleep cycle, they never pass the threshold into restorative sleep (discussed more below).

Post-concussion patients with insomnia:
When asked what their post-concussion insomnia is like, many of our patients reply, “It’s like the off switch didn’t get clicked.” Falling asleep is just difficult. They may have some string of thoughts in their minds as they attempt to fall asleep, but it doesn’t follow a logical sequence. It’s like your brain is still on and working without a reason, leaving you frustrated and oh-so-tired.
For other patients, falling asleep is the easy part due to their fatigue. It’s staying asleep that’s the problem. They may jolt awake for seemingly no reason, or awaken at external stimuli they used to sleep through without difficulty. They’re often on high alert and are more sensitive to the sounds and events around them.
In both instances, insomnia is often made worse when combined with other symptoms. For example, let’s say you experience mood swings, headaches, and insomnia persistently after sustaining a mild TBI (aka, concussion). At first, you sleep about six hours per night — not a terrible number, but not ideal (especially for someone who is recovering). The extra fatigue and frustration you feel from not sleeping enough starts making the headaches worse, and that rolls over into the mood swings.
As the headaches and mood swings make your life more difficult, you have more to keep you awake at night. Over time, the downward spiral continues, and you’re only sleeping 2-3 hours per night — a dangerously low number.
While every patient’s experience is unique, the situation described above is, unfortunately, quite common among those with concussion-driven insomnia. As one of our patients said dryly, “I have emotional incontinence.”
The good news is that you don’t have to live that way forever. We can help you recover. To learn more about your options, schedule a consultation with our team.
Unfortunately, there isn’t much extra we can tell you about these three symptoms. They are considerably more rare than the first two, but they can stem from mild traumatic brain injury (mTBI).
If you experience these or other unusual sleep disturbances post-TBI and have no medical history or known risk factors for them, they may indeed stem from your injury. While we don’t fully understand what causes them, we do know that they can (but don’t always) resolve after successful post-concussion treatment.
To learn if treatment for post-concussion syndrome could help you resolve your sleep problems, book a free consultation with our medical team.
Sleep is not a settled science. There’s a lot we know, and even more that we don’t know. Fortunately, we know enough to explain roughly how healthy sleep works and how concussion damage can disrupt that process.
Sleep follows a set process every night. These stages are termed 1, 2, 3, and REM.
Stage 1 initiates the sleep sequence. You close your eyes, start calming down, and “drift off.” If you’ve ever jerked awake right before falling asleep, that most likely happened during Stage 1. You might not feel completely asleep during this stage.
In Stage 2, the autonomic nervous system decreases your heart rate and body temperature. You are still more likely to react to your surroundings, but this still counts as being asleep.
In Stage 3, your muscles relax and your blood pressure decreases. Stage 3 occurs around 30 minutes from when you first laid down (assuming you started Stage 1 right away). This time involves dreamless, deep sleep. If you suffer from hypersomnia, you may not be getting past this sleep stage.
The last stage of sleep is rapid eye movement sleep (REM). It doesn’t happen immediately after Stage 3 — Stage 2 and 3 sleep happen multiple times throughout the night, and REM actually happens less often. When you enter REM sleep, body paralysis sets in, your eyes move around behind your eyelids (hence the name of this sleep stage), and you may experience dreams.
Scientists believe that REM sleep is when your brain processes memories and generally cleans things up. If you aren’t getting enough REM sleep, it will definitely affect your cognitive processes.
A properly functioning sleep cycle depends on various parts of the brain and body working together to achieve sleep. Which system is affected depends on your specific injury. Here are a few possible scenarios.
Often, subcortical areas (like the thalamus or the basal ganglia) are not metabolically normal after injury. Technically, your hypothalamus is the region in control of sleep. But even if the hypothalamus was unaffected by your injury (and there’s no guarantee of that), it can be “tricked” by other regions into failing the sleep cycle.
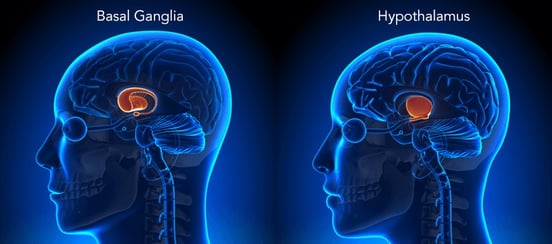
Think of it this way: Imagine that you (the hypothalamus) are in a group with three other students (for our purposes, the other brain regions involved in sleep). You’re pretty sure you have a group project due on Friday like you always do. But the other three insist that the professor didn’t assign anything, so you don’t turn in any work. But as it turns out, there was a group project and the others were wrong.
In a similar way, the hypothalamus might be guiding the changes your body needs for sleep, but if the areas coordinating with it (like the thalamus) aren’t doing their part, it will abandon the project of sleep at some point along the sleep cycle (or at least, not do a very good job). As a result, you experience poor sleep.
Any region in your brain can be affected by a TBI (mild or not), including regions that govern hormone production and regulation. For example, it has been shown that any kind of neurotrauma can change your production of melatonin and serotonin, two neurotransmitters involved in sleep (Shekleton et al., 2010; Yue et al., 2017). A head injury could affect the hypothalamus (a region right at the bottom and near-center of the brain), which controls the creation of melatonin. Dysfunction in other sleep-control areas, like the thalamus (which is right above the hypothalamus) could also prevent the brain from having a normal sleep architecture.
Head trauma can also affect your autonomic nervous system (ANS). The ANS controls all the bodily processes you don’t think about — like breathing, heart rate, fight or flight response, and more. Many of the concussion patients we treat have an over-activated sympathetic nervous system (meaning their bodies are stuck closer to “fight or flight” mode than normal).
But those systems are the same ones involved in calming down and sleeping peacefully! Your body relies on an internal clock to know when to go to sleep and when to wake up. It gets information from multiple sources — blue light exposure, body temperature, hormonal fluctuations, and so forth.
If those are off because of a head injury, then your internal clock can be confused, having you sleep more or less and at different times than you normally should.
In another post, we explained what causes post-concussion syndrome, how it’s diagnosed, and how it’s treated. We recommend reading that post to get a better overall understanding of PCS.
In this post, we’d like to dig deeper into how that treatment can resolve sleep issues. Here’s a quick overview of how we approach treatment:
So, what aspects of concussion treatment will help you sleep better?
First, the changes in your brain that occur during treatment (read more about that here) will help regions that could be affecting sleep adjust and behave normally. If you have hormone dysregulation that does not get better with treatment, we can pair you with an endocrinologist who will work with you to obtain replacement doses for what you need.
Second, getting physically active makes a huge difference when it comes to sleep. But many of our patients experience worse symptoms when they exercise, so they quit exercising altogether. During treatment, we will rehabilitate your ability to exercise. Continuing with the at-home exercises we recommend ensures the positive changes continue.
Third, we have therapy specifically for patients whose ANS is dysregulated. We’ll go over mindfulness and breathing techniques, plus teach you how to use helpful apps like Brainwaves and Binaural Beats to continue helping your autonomic nervous system.
Finally, all patients have at least two sessions with a psychologist. She will equip you with the tools you need to heal emotionally — another important change if you want a good night’s sleep.

We’ve had patients come into our clinic on all kinds of sleep medicine — Ambien, Diazepam, Doxepin, Trazodone, etc.
Note: If you’re taking Benadryl to sleep better, please see a doctor for help with stopping its use immediately. It is not safe to use long-term.
Sleep medication almost always has side effects or long-term consequences. We do our best to advise you, but the choice is ultimately yours. If you’re only sleeping three hours per night and your symptoms are out of control, then sleep medication makes sense until you can seek treatment. But if you’re able to get a handle on your symptoms without resorting to medication (whether over-the-counter or prescribed), it’s almost always better to do so.
For example, some patients love ZzzQuil (it’s basically Nyquil without the cold medicine). But for many patients, it will actually prevent you from going into REM sleep. So while you’re technically asleep for longer, the sleep quality is not what it needs to be.
The one pill we do recommend is melatonin. Our patients have varying success with melatonin, for two main reasons:
In the next section, we’ll discuss what you can do to improve your sleep without the use of sleep medication.
If you’re trying to improve your sleep patterns, one of the best places to start is self-awareness. What is making it more difficult for you to sleep at the time you’re supposed to sleep? Are you experiencing concussion symptoms that keep you from calming down? Is your sleep schedule inconsistent? Is your stomach often upset?
Try to jot down what you think is interfering with your sleep each night. If a pattern emerges, it will be that much easier to identify what’s wrong and adjust your routine. It’s also helpful to note the amount of sleep you get each night if you can.

One of the best things you can do to help your body through the proper sleep sequence is to make your own Stage 0 of sorts. Look for ways to make your bedtime routine a) consistent, and b) calming.
Here are a few behavioral changes you can make to encourage a good night’s sleep:
Sleep and nutrition are closely linked. Make sure your body has the components for making neurotransmitters: magnesium, folate, inositol (vitamin B8), calcium, iron, and good fatty acids. A diet high in sugar and/or trans fat has been associated with poor quality sleep.

It’s worth experimenting to see if certain food groups help you sleep better. If you notice you always sleep well after eating yogurt, for example, then you may benefit from eating more foods that contain tryptophan.
Sleep problems are always worth addressing, but some require more extensive medical intervention. If you find that you continually sleep more and more over time, or that you’re incapable of sleep, seek medical attention immediately. Your healthcare provider may order an MRI, CT scan, and/or sleep study in case you have a life-threatening condition.
As long as your brain is structurally sound, the next best thing is to pursue treatment for a mild traumatic brain injury. At Cognitive FX, we work with many concussion patients who have experienced sleep disturbances. They frequently let us know after treatment that they are sleeping better. We love getting calls when a patient is finally able to dream again!
If you would like to learn more about how to recover from post-concussion syndrome sleep problems, schedule a consultation with our team.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Sleep disturbances are a common yet often overlooked consequence of traumatic brain injuries (TBI). Many patients struggle with insomnia — having trouble falling asleep or waking up frequently during...

You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.
.png?height=175&name=image2%20(5).png)
Have you ever caught yourself holding your breath while doing something challenging? Or feeling lightheaded and breathing faster when you stand up after sitting for a long time? Maybe you often have...

Returning to work after a concussion—especially if you’re still experiencing symptoms—can be a difficult and uncertain process. There’s no one-size-fits-all answer. For many patients, it’s possible...
.png?height=175&name=Why%20Post-Concussion%20Syndrome%20Causes%20Tingling%20Hands%20(And%20What%20to%20Do).png)
Tingling hands following a concussion (mild traumatic brain injury, or mTBI) might sound relatively minor, but for anyone who’s had the misfortune to experience this symptom, it can be painful,...
Perhaps this sounds familiar: You wake up from a relaxing nap expecting to feel refreshed, but instead, your heart is pounding for no reason. Or you stand up after a few hours on the couch and feel...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY