Sleep disturbances are a common yet often overlooked consequence of traumatic brain injuries (TBI). Many patients struggle with insomnia — having trouble falling asleep or waking up frequently during the night — while others experience excessive sleepiness, finding themselves sleeping more than usual. These disruptions can significantly impact recovery, especially when combined with other TBI-related symptoms such as cognitive difficulties, emotional changes, and chronic pain.
Research suggests that between 30% to 70% of TBI patients experience sleep problems, with symptoms appearing immediately after the injury or developing months later. Interestingly, sleep difficulties are more prevalent in those with mild traumatic brain injuries compared to those with moderate or severe injuries. This may be due to increased awareness of symptoms in mild cases, as well as the pressure to return to normal activities, which can lead to stress-induced sleep issues.
While therapy and sleep medications are common treatments, they may not be enough for many TBI patients, whose sleep challenges are deeply intertwined with other neurological and physiological dysfunctions. For effective recovery, it’s crucial to address these problems holistically.
In this article, we’ll cover:
Understanding the connection between TBI and sleep is the first step toward finding effective solutions that promote healing and long-term well-being.
If you've had one or more head injuries and experience common symptoms such as headaches, brain fog, sleep-wake disorders, and more, you're not alone and you're not imagining it. Help is available. Peer-reviewed research shows that 77% of patients treated at our clinic experienced significant improvement in their post-head injury symptoms.Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. Schedule a consultation to see if you’re eligible for treatment.
Types of Sleep Problems After a TBI
Under the umbrella term “sleep problems”, TBI patients may experience many different types of sleep disturbances. Some of the most common types include:
-
Insomnia: This is the most common sleep issue, affecting about 50% of TBI patients. It involves difficulty falling asleep, frequent nighttime awakenings, or waking too early feeling unrested. Insomnia can worsen cognitive and behavioral symptoms but often improves over time.
-
Hypersomnia: Excessive sleepiness or prolonged sleep, known as posttraumatic hypersomnia or narcolepsy, affects ~20% of TBI patients. It’s often linked to concentration issues, memory impairment, and fatigue.
-
Parasomnia: About 25% of TBI patients experience abnormal sleep behaviors, such as sleepwalking, talking during sleep, teeth grinding, nightmares, and dream-enacting behaviors.
-
Disrupted sleep patterns: Some patients develop irregular sleep-wake cycles, making it difficult to maintain a routine. In severe cases, sleep patterns become erratic, with multiple sleep-wake disturbances throughout the day, often leading to excessive daytime sleepiness and disruptions unrelated to natural light cycles.
-
Sleep-related breathing disorders (sleep-disordered breathing): Sleep apnea, with a prevalence of ~20% among TBI patients, causes pauses in breathing during sleep, leading to snoring, frequent awakenings, morning headaches, and fatigue due to reduced oxygen flow to the brain.
These sleep disturbances can significantly impact recovery, making proper diagnosis and treatment essential.
What Causes Sleep Problems After a TBI?
Sleep problems can be caused by a variety of factors, including:
Direct Impact on Parts of the Brain Involved in Sleep Regulation
Any injuries to parts of the brain involved in sleep regulation can trigger sleep disorders. Damage to the hypothalamus, brain stem, or reticular activating system can trigger changes in the sleep-wake cycle. For example, if the connection between the eyes and the hypothalamus is disrupted, it can lead to abnormal circadian rhythms. In addition, brain and neck lesions caused by whiplash can also cause hypersomnia, breathing difficulties, and sleep apnea.
Neurovascular Coupling (NVC) Disruption
In a healthy brain, nerve cells rely on neurovascular coupling (NVC) — a dynamic process where blood vessels deliver oxygen and nutrients precisely when and where they are needed. This ensures the brain can function efficiently.
After a TBI, this process is often disrupted. When NVC dysfunction affects areas responsible for sleep regulation, the brain struggles to maintain a normal sleep-wake cycle, leading to sleep disturbances and disorders.
Autonomic Nervous System (ANS) Dysfunction
The autonomic nervous system (ANS) regulates essential bodily functions like breathing, heart rate, and blood pressure. It has two key components:
-
The sympathetic nervous system (SNS), which triggers the "fight or flight" response.
-
The parasympathetic nervous system (PNS), which controls "rest and digest" functions.
In a healthy body, these systems work in balance, shifting between alertness and relaxation as needed. However, even a mild TBI can disrupt this equilibrium, often causing the SNS to remain overly active. This heightened state of alertness interferes with sleep by preventing the smooth transition from wakefulness to rest.
Normally, as a person falls asleep, the body shifts from SNS dominance to PNS control, lowering heart rate and blood pressure to promote relaxation. Later, during REM sleep, the SNS briefly reactivates. After a TBI, this transition is often impaired, leading to insomnia, sleep apnea, and other sleep disturbances.
Further reading: Dysautonomia after a head injury
Hormonal Imbalances
A TBI can disrupt the hormonal systems that regulate sleep, leading to significant sleep disturbances. Studies show that TBI patients often have deficits of hypocretin, histamine, and melatonin, which play key roles in sleep regulation:
-
Hypocretin & Histamine: These neurotransmitters promote wakefulness. Low levels are linked to hypersomnia, causing excessive sleepiness and fatigue.
-
Melatonin: This hormone regulates the sleep-wake cycle. Reduced melatonin levels are associated with poor sleep quality and decreased REM sleep in TBI patients.
These hormonal imbalances can make it difficult to achieve restful, restorative sleep, further complicating recovery.
Other TBI Symptoms Affecting Sleep
Sleep problems can also stem from other TBI-related symptoms, creating a cycle that worsens overall recovery. For example:
-
Pain and low mood can make falling asleep difficult.
-
Fatigue may lead patients to take frequent naps, disrupting their ability to sleep at night.
Sleep disturbances can lead to a worsening of these symptoms, prolonging recovery and significantly impacting quality of life. This is why addressing both sleep issues and underlying TBI symptoms is essential for effective treatment and overall well-being.
Medication Side Effects
Certain medications prescribed after a TBI can disrupt sleep, causing insomnia or excessive drowsiness, which can further impact neuropsychological function such as memory, concentration, and mood. For example:
-
Antidepressants and stimulants may lead to insomnia, especially if taken too close to bedtime.
-
Over-the-counter painkillers sometimes contain caffeine, a stimulant that can interfere with sleep.
In many cases, adjusting medication timing or switching to an alternative can help minimize sleep disturbances. Always consult your doctor before making any changes.
How Are Sleep Problems Treated?
Most patients with sleep problems go through a series of steps covering different treatment options until they find one that can help.
Sleep Hygiene and Lifestyle Changes
Improving sleep hygiene is the first step in addressing sleep problems after a TBI. Simple lifestyle adjustments can significantly enhance sleep quality.
Daytime Tips
-
Wake up at the same time daily to regulate your sleep cycle.
-
Stay engaged in meaningful activities to keep your mind active.
-
Limit screen time, especially in the evening, to reduce blue light exposure.
-
Exercise regularly, but avoid intense workouts close to bedtime.
-
Get natural light exposure during the day. If sunlight is limited, consider light therapy.
-
Take short 20-30 minute naps to avoid disrupting nighttime sleep.
Nighttime Tips
-
Stick to a consistent bedtime to reinforce a healthy routine.
-
Follow a relaxing pre-sleep routine, such as reading or listening to calm music.
-
Avoid caffeine, nicotine, and alcohol in the evening, as they can interfere with sleep.
-
Skip heavy meals before bed to prevent discomfort.
-
Create a restful sleep environment — keep your room cool, quiet, and dark.
-
If you can't sleep within 30 minutes, get out of bed and do a quiet, non-stimulating activity until you feel drowsy.
These small changes can lead to noticeable improvements in sleep quality for TBI patients.
Cognitive Behavioral Therapy for Insomnia (CBTi)
When lifestyle changes aren’t enough, Cognitive Behavioral Therapy for Insomnia (CBTi) is a highly effective, non-pharmacological treatment.
CBTi helps patients identify and change negative thoughts and behaviors that interfere with sleep. Studies show it can improve sleep quality by reducing the time it takes to fall asleep, decreasing nighttime awakenings, and promoting deeper rest.
The American College of Physicians recommends CBTi as the first-line treatment for insomnia before considering medication.
Light Therapy
Light therapy, or phototherapy, is another non-medication approach that can help regulate circadian rhythms and improve insomnia in TBI patients.
This therapy involves sitting in front of a light box emitting up to 10,000 lux for 30 minutes to an hour daily, as recommended by a doctor. The goal is to stimulate melatonin production, promoting a healthier sleep-wake cycle.
However, some TBI patients are sensitive to light, making this treatment unsuitable for everyone. A healthcare provider can help determine if light therapy is a good fit.
Medications & Supplements
When other treatments fail, sleep medicine or supplements may be needed, including:
-
Prescription sleeping pills: These can help patients fall asleep and stay asleep, but they are not a cure. They are often used short-term, especially in severe TBI cases where cognitive impairment makes lifestyle changes difficult. Common options include antidepressants, barbiturates, and benzodiazepines for insomnia, while stimulants and wakefulness-promoting agents may help with hypersomnia.
-
Natural supplements: Some patients prefer melatonin or valerian to avoid medication side effects. Melatonin can enhance sleep quality, duration, and efficiency in TBI patients, while valerian may support sleep, though its effectiveness in TBI patients is unproven.
A doctor should always guide medication or supplement use to ensure safety and effectiveness.
Why Sleep Medications and Therapy Alone May Not Be Enough
TBI patients rarely experience sleep disturbances in isolation. Many also struggle with headaches, dizziness, fatigue, memory and attention difficulties, depression, and anxiety — all of which can worsen sleep problems and slow recovery. For example, chronic headaches can disrupt sleep, which in turn impairs cognitive function and increases fatigue, creating a frustrating cycle.
Since these symptoms are deeply interconnected, treating sleep problems alone is often ineffective. A comprehensive approach that addresses both sleep disturbances and their underlying causes is essential for meaningful recovery.
At Cognitive FX, we focus on whole-brain rehabilitation, targeting the root causes of sleep disturbances alongside other TBI-related challenges to promote long-term healing.
Receiving TBI Treatment at Cognitive FX
We begin with a comprehensive evaluation to understand how your TBI has affected your brain and body. A member of our team will review your medical history and symptoms, including any sleep disturbances.
To gain a deeper understanding, we conduct a series of specialized tests, including:
-
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
-
A neurocognitive test to assess memory, concentration, reasoning, and other cognitive functions.
-
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
-
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
-
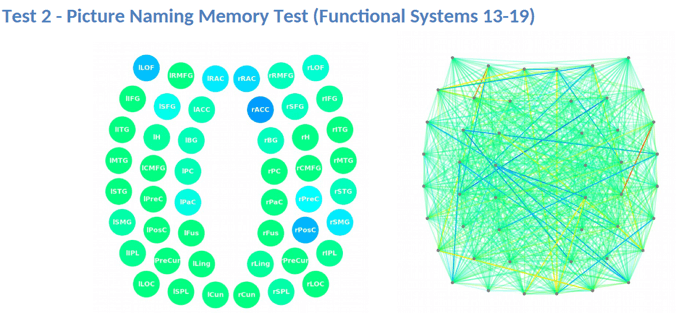
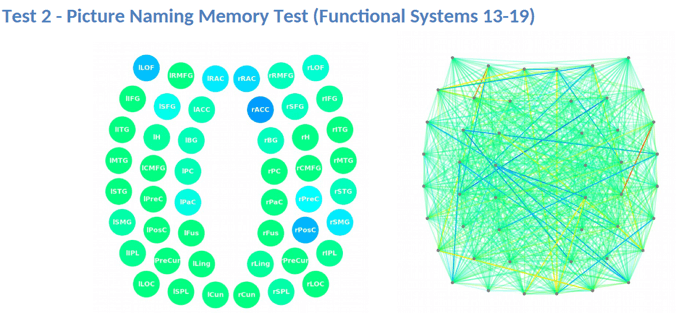
A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how your brain was affected by the injury.
The fNCI scan measures blood flow in 100 brain regions while patients perform standardized cognitive tasks. These real-time images are then compared to scans from healthy individuals to identify areas with neurovascular coupling (NVC) dysfunction.
Brain regions are grouped by function and scored:
-
Green indicates normal function.
-
Yellow and red highlight areas with NVC dysfunction, signaling impaired brain activity.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
After the evaluation, our team analyzes the results and creates a customized treatment plan tailored to each patient’s specific areas of dysfunction. The goal is to restore normal neurovascular coupling and improve overall brain function.
What EPIC Treatment Is Like
During treatment week, patients follow a structured program combining aerobic exercise and targeted therapies to enhance brain function. Each session begins with aerobic exercise to boost blood flow, followed by a personalized mix of therapies designed to support brain healing. The specific treatments vary based on each patient’s scan results, ensuring a tailored approach to recovery.
Therapy typically consists of a mix of the following:
-
Cognitive therapy: The aim of cognitive therapy is to rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning. Sessions include cognitive activities, such as solving logic puzzles and identifying word patterns
-
Occupational therapy: Patients engage in exercises that help the brain, body, and eyes coordinate with each other. The aim is to help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
-
Neuromuscular therapy: The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity. Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
-
Sensorimotor therapy: Patients follow exercises to improve cognitive and physical skills and reduce symptoms of depression. This includes, for example, simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms
-
Vision therapy: The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity. Our therapists use different exercises, including Dynavision, visual tracking exercises, the Brock String, and some other computerized technologies.
-
Neurointegration therapy: The aim is to assess the visual, vestibular, and proprioceptive systems, and integrate them to improve patients’ ability to function in the world. Patients receive help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well, such as saccades, near/far focusing, convergence/divergence, peripheral awareness, and hand/foot/eye coordination.
-
Psychotherapy: Patients meet with a clinical psychologist to evaluate their mental health status and learn mindfulness exercises and other relaxation strategies to improve their quality of life. For those suffering from depression and anxiety, our therapists recommend cognitive behavioral therapy (CBT). We do not offer this type of therapy but can refer them to a specialist.
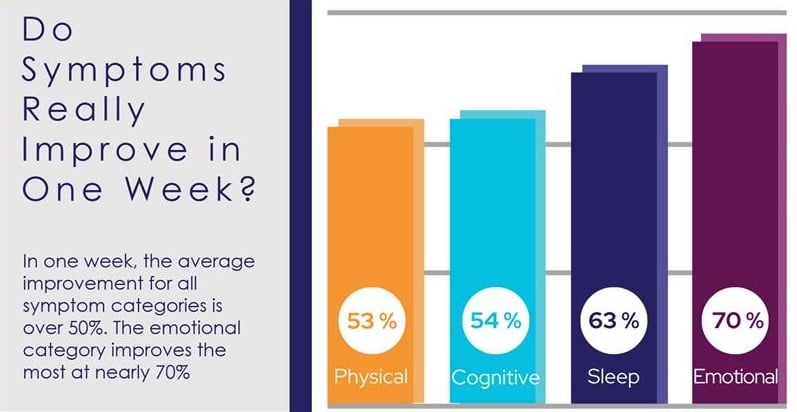
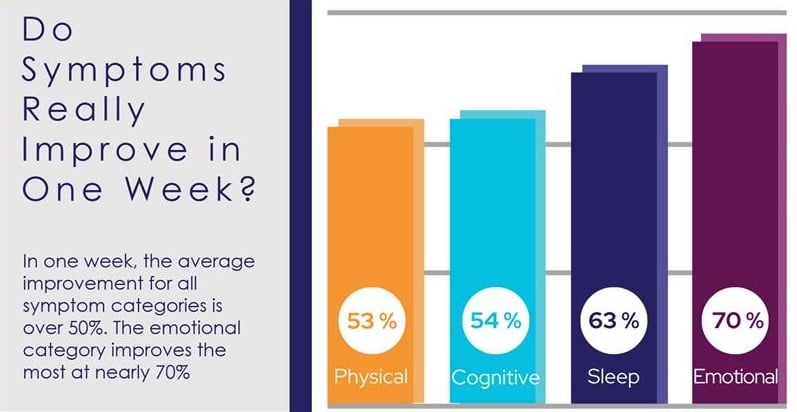
At the end of treatment, patients undergo a follow-up scan to see how the brain is responding to therapy. While some experience immediate, significant improvements, others may need more time for changes to take effect. 90% of our patients report symptom improvements during treatment, with continued progress at home.
Following treatment, our team reviews your scan results and provides a personalized recovery plan, including aerobic exercise, cognitive games, and cognitive rest to support long-term healing.
On average, our patients’ symptoms improve by over 50% after just one week of treatment. To see if you are eligible for treatment, sign up for a consultation.





.png?height=175&name=image2%20(5).png)




.jpg?height=175&name=Slow%20Concussion%20Recovery%20(6).jpg)