Can Post-Concussion Syndrome Cause Stuttering?
Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Have you ever caught yourself holding your breath while doing something challenging? Or feeling lightheaded and breathing faster when you stand up after sitting for a long time? Maybe you often have rosy cheeks without a reasonable cause, like exercise.
These are all signs of respiratory issues in patients suffering from post-concussion syndrome (PCS). Post-concussion syndrome occurs when symptoms of concussion linger beyond three months after the injury. Some patients suffer from PCS for years before getting a diagnosis and treatment.
After a concussion, your body can “forget” how to breathe properly. Under normal circumstances, the brain adjusts breathing rates based on what you need in the moment. Take exercise, for example: Your muscles need more oxygen when you’re active, so the brain tells the lungs to increase breathing rates.
In some concussed patients, this communication between the brain and lungs is disrupted. If the brain can’t react with accuracy and precision to the body’s changing needs, patients suffer from breathing disturbances, causing symptoms such as shortness of breath, dizziness, flushing, and fatigue.
Breathing problems can be difficult to recognize after a traumatic brain injury (TBI). They often aren’t noticeable as breathing problems; instead, they contribute to other symptoms, such as exercise intolerance, headaches, fatigue, and sleep disruption, which can severely affect your normal activities.
Rehabilitating the connection between the brain and the lungs isn’t straightforward, either. It needs to be part of an overall effort to help the brain and autonomic nervous system recover from the long-term effects of brain injury.
At our post-concussion syndrome treatment clinic, we provide a combination of physical and cognitive therapies designed to rehabilitate the brain and body after a concussion or other brain injury. During this period of time, we also teach patients exercises to help retrain their breathing patterns.
In this article, we explain:
If you’re experiencing emotional, cognitive, and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, sign up for a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
-1.jpg?width=1000&name=image4%20(1)-1.jpg)
Breathing is an automatic action controlled by a part of the brain called the brainstem. This control is continuous and involuntary; you don’t have to consciously think about it for it to happen.
An important aspect of the respiratory system is its ability to adjust to changes in carbon dioxide (CO2) and oxygen (O2) levels in the blood.
This flexibility stems from sensors located throughout the body. In simple terms, these sensors send signals to the brainstem, which in turn adjusts breathing patterns as needed.
For example, when you exercise, carbon dioxide levels increase in the blood. This change triggers those sensors to signal the brain to increase breathing rates. As a result, carbon dioxide levels decrease and oxygen levels increase—a necessary change during exercise. When you stop physical activity, breathing rates and oxygen levels gradually return to normal.
.jpg?width=1000&name=image1%20(1).jpg)
After a concussion, the brainstem may incorrectly detect and react to different levels of carbon dioxide and oxygen in the blood. As a result, it may respond inappropriately to your body’s needs. This is when breathing problems arise.
The two most common respiratory problems after brain damage include:
It can be difficult to determine if you are experiencing one or the other. In fact, it’s likely that you shift between the two types during different activities and different times of the day. A trained therapist, like the ones at Cognitive FX, will be able to tell you what’s happening with your breathing and suggest exercises to help you.
Not every person will have all of these symptoms. And the symptoms you do have may come and go. Stress often produces an increase in symptoms.
Most patients with dysregulated breathing feel tired and struggle with physical exercise. You may experience shortness of breath, lightheadedness, and dizziness even after light exercise. More strenuous exercise can trigger severe symptoms like wheezing or tightness in your chest. This is all because your body is not getting enough oxygen to cope with the increase in activity.
We also notice that many of our patients hold their breath when they’re concentrating on cognitive tasks, like word games or puzzles. If this happens to you, it’s because your brain is struggling to complete both tasks at the same time. So, it tries to solve the problem by putting one of those activities (breathing) “on hold.”
Facial flushing is another common symptom. If you take shallow breaths, carbon dioxide starts accumulating. Since carbon dioxide is a vasodilator, it leads to increased blood flow in the face, thus explaining the rosy cheeks.
For the same reason, some patients experience an increased incidence of headaches and migraines. They often happen in the morning after waking up due to a buildup of carbon dioxide in your blood while you sleep.
-1.jpg?width=1000&name=image6%20(2)-1.jpg)
It’s common for PCS patients to experience respiratory issues, but research in this area is very limited.
Most of the work done in this area focuses on potentially life-threatening respiratory problems after a severe traumatic brain injury (TBI). TBIs can cause a skull fracture, brain swelling, blood clots, brain tissue damage and localized hemorrhage, and loss of consciousness. Many patients with these complications need immediate medical care and ventilatory support to breathe.
PCS patients who suffered a mild TBI don’t experience such extreme symptoms. The most likely ways in which a concussion may cause breathing issues include:
Neurovascular Coupling Dysfunction
Despite its relatively small weight (around 2% of total body weight), the brain needs a disproportionate amount of oxygen. Under normal circumstances, nerve cells in the brain use about 20% of the total oxygen used by the body.
To further complicate matters, the brain's energy needs vary greatly depending on neural activity. It’s vital to ensure that oxygen-rich blood is delivered to the right place, in the right amount, at the right time. To meet these ever-changing demands, the brain relies on a network of blood vessels that bring oxygen and nutrients to the areas that need it. This dynamic is known as neurovascular coupling (NVC).
After a head trauma, however, NVC is disrupted. As a consequence, areas of the brain affected by the concussion don’t use oxygen efficiently. The oxygen might not be delivered to the region that needs it most, or the brain region might consume far more oxygen than normal to complete its tasks. To compensate, the body attempts to pump more blood to the brain, which may lead to shallow breathing.
If you’re experiencing emotional, cognitive, and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, schedule a consultation.
Problems Regulating Blood Pressure
Every time you stand up or move around, your body needs to make small increases in your blood pressure to keep a constant blood flow to the brain at all times.
PCS patients, however, often experience dizziness and lightheadedness when the brain fails to make these adjustments and blood accumulates in the lower part of the body as they stand up. The most common causes of this dysfunction are not yet fully understood, but poor blood pressure regulation can also lead to respiratory problems, including abnormally fast breathing.
Autonomic Nervous System (ANS) Dysfunction
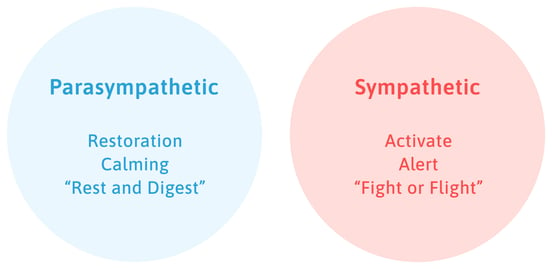
The autonomic nervous system is involved in regulating a variety of body functions, such as blood pressure, digestion, pupillary response, and breathing rates.
The ANS has two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system. The SNS is called the "fight or flight" system, while the PNS is considered the "rest and digest" system. In many cases, these systems have opposite actions. One system activates a physiological response, and the other inhibits it.
This is also the case during cycles of inhaling and exhaling: As you inhale, the SNS triggers a brief acceleration of your heart rate, and as you exhale, the PNS brings heart rate back to normal. As PCS patients often experience problems with their autonomic nervous system (which we’ve described in detail in another blog post), it may not be able to adjust heart rate as needed, leading to respiratory problems.
Problems with Interoception
Interoception is a scientific term to describe how you feel what’s happening inside your body, such as a growling stomach when you’re hungry or a racing heart when you exercise.
After a head injury, this process may be disrupted and the brain then becomes less able to understand and react appropriately to some of the signals it receives. For example, patients may start fixating on their headache and fail to realize their breathing patterns changed.
On the other extreme, if patients are in a situation which may have caused breathlessness in the past or are watching somebody experiencing shortness of breath, they can actually start feeling respiratory problems. For example, you may start to feel shortness of breath even before you start climbing the stairs because that’s what your brain expects to happen.
Dysfunction in the Brainstem
Located at the base of the skull, directly above the spinal cord, the brainstem is viewed as one of the most important areas in the brain. This area is responsible for all the functions that keep you alive, including heart rate, blood pressure, breathing patterns, and consciousness, among others.
Inevitably, any damage to this area will affect many of these functions, including breathing. For example, if a damaged brainstem can’t detect levels of carbon dioxide and oxygen in the blood, it can’t increase or decrease breathing patterns when needed.

In addition to breathing problems, PCS patients experience a wide range of other symptoms, such as brain fog, blurry vision and other vision problems, memory loss, emotional changes, and difficulty concentrating. Many healthcare providers approach PCS care by treating individual symptoms. They might not make the connection between what you’re experiencing and your mild traumatic brain injury.
Instead, our approach is to address the root cause of all these symptoms: changes in neurovascular coupling.
Understanding this mechanism and how it’s affected by concussions is key to treating patients with post-concussion syndrome. That’s why all our patients undergo an fNCI (functional Neurocognitive Imaging) brain scan before starting their treatment program at Cognitive FX.

An fNCI is a special type of MRI scan that measures blood flow to different areas in the brain while patients complete a series of cognitive tasks. This scan allows our team to identify what regions in the brain are dysfunctional. With these results, we can then tailor the treatment offered to the needs of each patient.
Treatment includes several types of therapy, including but not limited to:
Some other examples of therapy include sensorimotor therapy, dynavision, and occupational therapy.
-1.jpg?width=1999&name=image9%20(1)-1.jpg)
At the end of treatment, patients undergo a second fNCI to assess how much they’ve improved. They also receive a series of exercises to do at home to maximize their chances of a full recovery.
Throughout these sessions, there are many ways our therapists can offer extra help for patients dealing with breathing problems:
We teach all our patients a few breathing exercises to help them relax and breathe better. Breathing in through the nose is the best way to get the diaphragm to initiate the breath, which pulls more air into the lower lungs and activates the PNS. Mouth breathing creates a more shallow breath, keeps air in the upper chest, and is part of the "fight or flight" cycle, increasing SNS activity.
Our treatment also includes periods of rest and relaxation to allow your brain to recover before the next set of therapy sessions. We promote meditation or the use of Brainwave apps, which use sequences of binaural tones to stimulate brainwave frequencies associated with various states of mind. For example, our therapists can set the app for the alpha pattern (frequency of 7–13 Hz) or theta pattern (4-7Hz) to encourage relaxation and meditation.
We sometimes use physical devices to help our patients learn to breathe more effectively. One of these is called a breathing belt. The breathing belt wraps around the lower ribs and diaphragm to give patients feedback around their breathing mechanics. They often wear it throughout the day to give the brain the reminder of how they are supposed to breathe in order to make the new pattern more habitual more quickly.
We also use a Relaxator to help slow down the breath and provide a proper ratio of inhale to exhale. It provides resistance to the exhale, forcing the breath to slow down and restore balance. As patients' competency and ability to control their breath improves, the resistance is increased to continue to build and strengthen that pattern.
Another technology we use is Aftershokz bone conduction headphones. Research has shown specific frequencies activate the vestibular system via sound waves vibrating through the bones of the skull to the vestibular organs. We test to find the frequency and side (Left, Right, or Both) that each patient needs to restore balance to the vestibular system and decrease ANS dysregulation symptoms.
If patients are struggling during their therapy sessions, they can have a short break to perform a few breathing exercises to relax and then resume when they can.
We find that some patients experience breathing and swallowing problems at the same time. This is not surprising, given that both functions are regulated by the brainstem. These patients need special therapy exercises to re-train their tongue and learn how to swallow and drink. We teach many of them in Neural Integration Therapy, but will refer you for further work with a specialist if needed.
Note: Many COVID long haulers suffer from a similar phenomenon (breathing dysfunction after COVID). Breathing problems are often more pronounced in post-COVID patients than in PCS patients. Treatment approaches for both are very similar. Our research is ongoing, and we’ve only treated a limited number of COVID long haulers, but we’ve had good results so far. Not surprisingly, many of our COVID long haulers experience shortness of breath more directly than PCS patients. But PCS patients can suffer a wider range of respiratory issues. If you or family members are suffering from long-lasting symptoms after COVID, we offer a consultation to determine if they could benefit from treatment at our clinic.
.jpg?width=1000&name=image3%20(1).jpg)
The best way to keep your breathing problems under control is to continue performing breathing exercises at home. The same way long-term physical exercise improves heart function and strengthens muscles, breathing exercises improve lung function and promote healthier blood flow.
If you have a sudden increase in breathing symptoms or find it so difficult to breathe that you feel dizzy or nauseated, seek immediate medical attention.
If you’re experiencing emotional, cognitive, and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, schedule a consultation.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...

Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect...

Brain fog is one of the most common symptoms of concussions and post-concussion syndrome (PCS). Some people experience brain fog immediately after a concussion; for others, it might come days, weeks,...

Traumatic brain injuries (TBIs) can change how a person experiences and expresses their sexuality. For some, the effects are subtle. For others, head injuries can cause dramatic changes to their sex...


Oxygen is good for the brain. A lack of oxygen is bad for the brain. So is getting more than normal levels of oxygen better for the brain?
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY