12 Recovery Tips for Patients with Post-Concussion Syndrome
Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can result from post-concussion syndrome (PCS).
Patients with PCS-induced stuttering struggle to keep a normal flow of speech, often repeating words, pausing mid-sentence, or getting stuck on specific sounds. Not surprisingly, this can lead to frustration, anxiety, and withdrawal from social interactions.
To make matters worse, stuttering rarely appears in isolation. It often occurs alongside other lingering PCS symptoms such as brain fog, headaches, dizziness, balance problems, and mood changes, to name just a few. These symptoms can persist for months or even years without proper treatment.
At Cognitive FX, speech-language pathologists are essential members of our multidisciplinary team. Our PCS rehabilitation program, Enhanced Performance in Cognition (discussed below), includes addressing speech disorders and communication challenges resulting from brain injury.
In this article, we’ll cover:
If you’re experiencing persistent symptoms such as speech problems, headaches, brain fog, fatigue, vision changes, and more, months or years after a concussion, you’re not alone—and you’re not crazy. These are real symptoms caused by changes in the brain and autonomic system, and they can be helped. Over 90% of our patients experience significant recovery after treatment in our clinic.To determine if our program is right for you, please schedule a consultation with our team.
While not one of the most common PCS symptoms, stuttering can emerge after a traumatic brain injury. This speech dysfluency is often accompanied by other language impairments, including slow or disorganized speech, trouble finding words, and difficulty coordinating vocal movements. Physical signs may include rapid eye blinks, lip tremors, facial tension, and head nodding.
Stuttering is more likely in patients who are also experiencing neurological fatigue or cognitive impairments. If the brain is under strain or not functioning efficiently, even basic tasks like speaking fluently become difficult.
Common stuttering behaviors include:
The two primary types of stuttering after a traumatic brain injury are neurogenic and psychogenic stuttering.
This form is caused by physical damage to brain regions involved in speech and language. Unlike developmental stuttering (common in children), neurogenic stuttering affects speech throughout a sentence and is generally less influenced by emotional state. However, stress and fatigue can still increase symptoms.
Associated communication disorders may include:
Psychogenic stuttering is linked to emotional trauma or psychological stress, rather than physical brain damage. It often emerges as a coping response, and typically occurs without other language impairments. Anxiety or emotional overload may trigger or worsen the symptoms.
Patients often describe their stutter as frustrating and unpredictable. They know exactly what they want to say but can’t get the words out. One patient said, “My mouth couldn’t keep up with my brain.” Many report their stuttering worsens with fatigue or stress and becomes more frequent later in the day.
As a result, some avoid conversations or withdraw from social situations. One patient described how her stutter became particularly noticeable at the beginning of sentences, leading her to avoid workplace interactions and choose solo tasks instead. Another patient felt frustrated that while her stutter was the most visible symptom, it wasn't the most debilitating—yet others assumed she was “better” once it improved.
Stuttering is just one aspect of PCS. Patients also contend with symptoms like dizziness, fatigue, sensory overload, and mood changes. Even if speech improves through therapy, those other challenges can persist. That’s why Cognitive FX treats PCS holistically, rather than targeting symptoms in isolation.
There’s no single cause of stuttering after a concussion. In most cases, it’s a combination of neurological, cognitive, and emotional factors, including:
Speech relies on multiple brain areas, including:
Left temporal lobe: Responsible for speech production and comprehension. Damage here can lead to aphasia, fragmented sentences, repeated words, and difficulty retrieving language.
Motor cortex, cerebellum, and basal ganglia: These areas coordinate the motor aspects of speech. Injury can cause slurred speech, poor coordination of the tongue or lips, or disruptions in speech rhythm. For example, damage to the cerebellum impairs motor coordination, while basal ganglia injury disrupts speech timing.
Neurovascular coupling ensures brain regions receive the blood flow needed to perform tasks efficiently. After a mild TBI, this process is often disrupted. When NVC disruption affects speech-related areas, fluency can suffer.
The autonomic nervous system (ANS) regulates many essential bodily functions like breathing, heart rate, and blood pressure. It has two key components:
In a healthy body, the sympathetic and parasympathetic nervous systems work in balance, shifting smoothly between states of alertness and relaxation. However, after a brain injury, this balance is often disrupted—a condition known as dysautonomia.
As a result, the sympathetic nervous system may remain overactive, keeping the body in a constant state of tension. This heightened physiological stress can interfere with cognitive function and speech fluency, particularly during emotionally charged or demanding situations.
Further reading: Dysautonomia after a head injury
It’s common for PCS patients to experience a variety of cognitive symptoms, including memory and concentration difficulties, brain fog, problems with executive function, and difficulty with problem-solving and decision-making.
While these problems can’t directly trigger a stutter, they may aggravate the severity and frequency of stuttering symptoms. If the brain struggles to process information, patients may struggle to maintain fluent speech, resulting in stuttering symptoms.
For example, if patients struggle with word retrieval, it can affect speech as patients can’t think of the words they want to say. This can lead to pauses and repetitions, which are typical stuttering behaviors.
Although anxiety doesn’t directly cause stuttering, it can intensify it. Patients who are anxious about speaking may stutter more frequently, especially in public or high-pressure settings.
A differential diagnosis is key to determining whether a patient’s stuttering is neurogenic, psychogenic, or both. The right treatment depends on the type of stuttering a patient is experiencing:
With neurogenic stuttering, patients benefit most from specialized speech-language pathology (SLP) focused on fluency modification techniques, such as:
These methods are practiced both in isolation and during cognitive tasks, helping patients speak fluently even when under cognitive load.
Ideally, therapy should be administered by speech therapists experienced in both fluency disorders and brain injury rehabilitation.
Cognitive Behavioral Therapy (CBT) is often effective for psychogenic stuttering. Cognitive behavioral therapists can help patients reframe negative thoughts, reduce anxiety, and build confidence in social interactions.
CBT can also be combined with traditional speech techniques to address both the psychological and physical components of speech disfluency.
At Cognitive FX, we treat stuttering as part of a larger pattern of neurological dysfunction. Our treatment combines speech-language therapy with cognitive training, physical therapy, and neurorehabilitation.
Our therapists use:
Patients also engage in:
While completing these exercises, patients apply fluency techniques like slowed speech, diaphragmatic breathing, and gentle articulatory contact. Practicing these strategies during challenging tasks builds resilience and improves real-world communication.
Stuttering is rarely the only concern for post-concussion syndrome patients. That’s why we address all symptoms together through our Enhanced Performance in Cognition (EPIC) program.
Every patient starts with a comprehensive assessment, including:
A meeting with one of our doctors to review the patient’s medical history and symptoms.
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health disorders.
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before starting.
A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected.
Rather than relying solely on patient interviews like most concussion clinics, we take a more precise approach by scanning the brain. We use Functional Neurocognitive Imaging (fNCI) to map how different areas of the brain are functioning after a concussion or brain injury.
This advanced fMRI scan measures two key things:
Regional Brain Activity: How much oxygen each brain region uses during specific cognitive tasks (indicating underactive, normal, or overactive function).
Connectivity Between Regions: How well different parts of the brain communicate with each other.
The scan results are visualized through intuitive charts and brain maps. These help us identify whether a patient is experiencing hypoactivity (under-functioning), hyperactivity (over-functioning), or a mix of both—and in which areas.
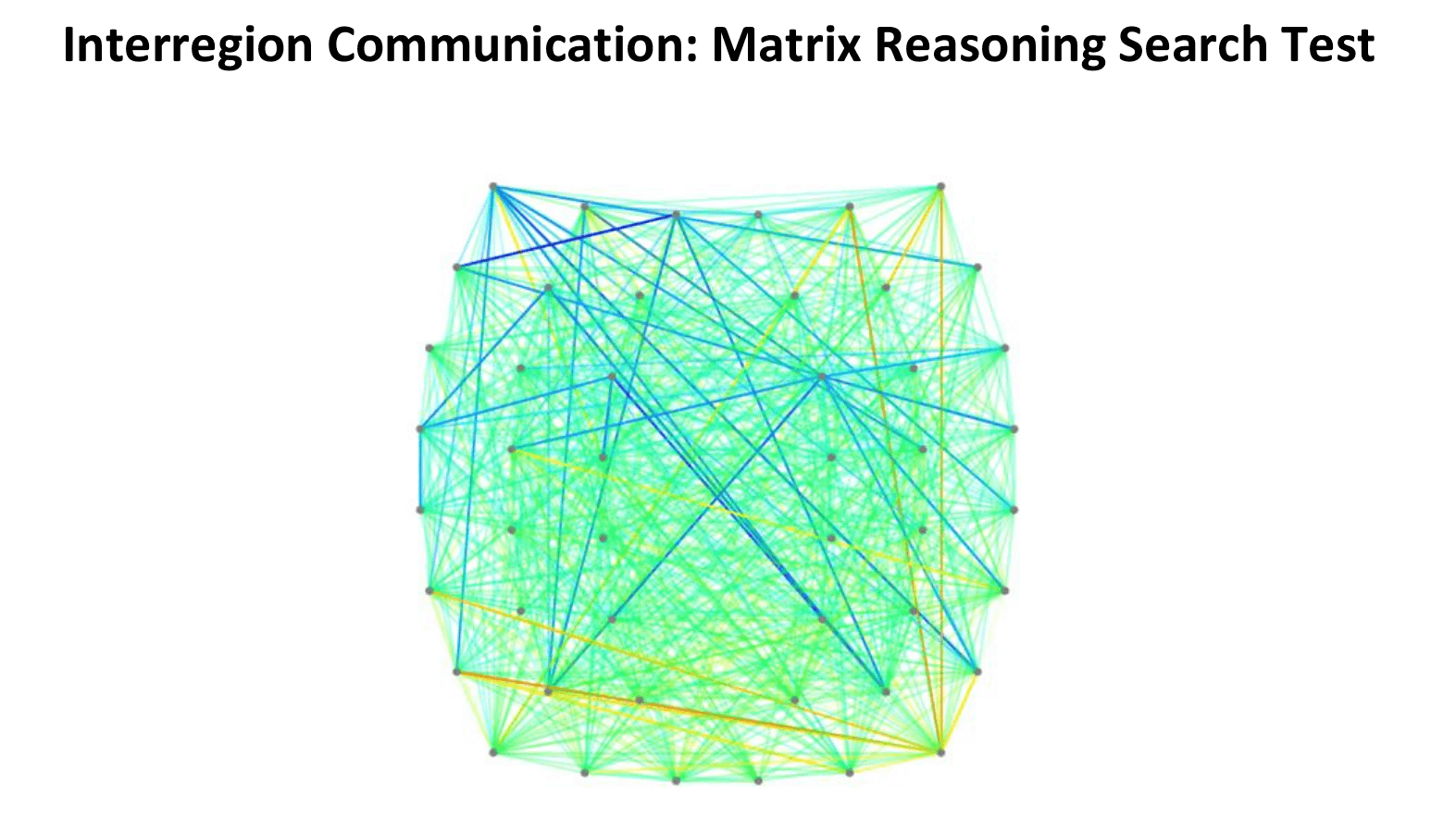
In this connectivity map, cooler colors (blues) indicate areas of hypoactivation (underactivity), while warmer colors (reds, oranges, yellows) indicate areas of hyperactivation (overactivity).
We’ve organized the results into six clear cognitive domains (like memory, attention, and executive function) to make them easier to understand and to better guide individualized treatment. For example:
Someone with hypoactivity may need brain stimulation and cognitive endurance training.
Someone with hyperactivity may benefit from therapies that reduce neural “noise” and promote regulation.
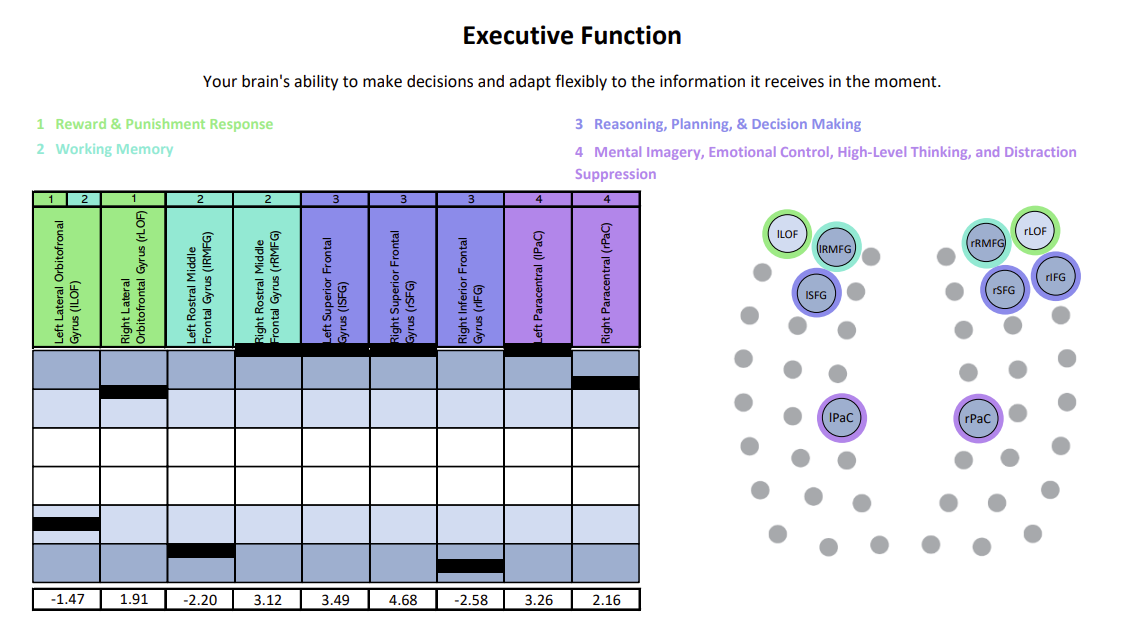
Each chart shows how a specific brain region is functioning compared to normal. The white area represents the normal range, with the center marking the average. Light and dark blue zones show increasing levels of abnormality. A black line marks the patient’s result for that region—ideally landing within the white. Lines in the light and dark blue zones suggest that the region is either hyperactive (blue zones above the white) or hypoactive (blue zones beneath the white, pictured above).
In the graph above, for example, a patient had hyperactivity in certain brain regions, and hypoactivity in others.
This detailed view of brain function lets us tailor therapy to each person’s precise needs—one of the core things that sets Cognitive FX apart.
Each day follows a three-step rhythm:

Therapy starts with short bursts of aerobic exercise, usually on a treadmill or stationary bike. Exercise triggers the release of important chemicals in the brain, which help the patient's brain become more flexible and boost the effects of subsequent therapy.
Even patients who struggle with physical activity due to their balance problems can make remarkable progress in these sessions. Our therapists are trained to help patients exercise according to their needs and without triggering severe symptoms.

After exercise, patients attend a variety of therapies, including cognitive therapy, sensorimotor therapy, neuromuscular therapy, Dynavision therapy, occupational therapy, neurointegration therapy, vision and vestibular therapy, and psychotherapy.
Patients typically receive most or all of these therapies during their visit, with a regimen tailored to their individual needs.
Rest periods are an important part of our treatment. Some examples of scheduled brain breaks include:
Neuromuscular massage: Therapists massage the neck and shoulders to relieve chronic pain and tension, relax muscles involved in vision, improve circulation, and alleviate headache pain.
Brainwaves: The binaural beats app we use produces two frequencies that are very close together. If you listen to a different frequency in each ear, your brain will average them together to produce one frequency. We set the parameters so that the frequency your brain creates is the same frequency you would experience through meditation. This frequency will propagate in your brain waves as you listen. As a result, you gain some of the restorative benefits of meditation without being a meditation expert.
Mindfulness: Patients learn mindfulness techniques during their time at the clinic.
At the end of treatment, patients undergo a second brain imaging scan to track their progress. Then, they meet with one of our therapists to review results and receive a series of at-home exercises.
These usually include physical activities, cognitive tasks, visual and vestibular exercises, and relaxation techniques. We recommend patients perform these exercises about an hour per day, five times per week initially, with the frequency decreasing as symptoms improve.
For patients needing further therapy, we provide referrals to appropriate specialists.
Stuttering after a concussion is a visible but complex symptom. It often coexists with other physical, cognitive, and emotional challenges. Treating it in isolation may offer short-term relief, but real recovery comes from addressing the whole brain.
At Cognitive FX, we combine cutting-edge brain imaging with a personalized, integrative therapy program to restore not only fluent speech but also the patient’s overall quality of life. We are one of — if not the only — healthcare clinics in the world with third party peer-reviewed research backing up the effectiveness of our treatment.
Over 90% of our PCS patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.

If you’ve suffered a concussion, you may have already encountered the Post-Concussion Symptom Scale (PCSS). This self-report questionnaire is one of the most widely used tools for documenting...

Traumatic brain injuries (TBIs) can change how a person experiences and expresses their sexuality. For some, the effects are subtle. For others, head injuries can cause dramatic changes to their sex...
.png?height=175&name=image2%20(5).png)
Have you ever caught yourself holding your breath while doing something challenging? Or feeling lightheaded and breathing faster when you stand up after sitting for a long time? Maybe you often have...


After a concussion or other brain injury, your loved one may start exhibiting some behaviors that are considered inappropriate and childlike. They may be prone to crying (emotional lability), angry...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY