If you’ve suffered a concussion, you may have already encountered the Post-Concussion Symptom Scale (PCSS). This self-report questionnaire is one of the most widely used tools for documenting concussion symptoms and tracking recovery.
Patients typically complete a PCSS:
- Immediately after injury (to establish symptom severity).
- Multiple times during recovery (to track improvements or setbacks).
Because it’s quick, easy, and standardized, the PCSS can help support diagnosis, monitor recovery progress, and predict long-term outcomes.
However, as we’ll discuss below, the PCSS has real limitations and is insufficient as a standalone diagnostic tool. Many concussion-related issues fall outside of its scope and more advanced tools are needed, particularly for patients with longer-lasting symptoms.
In this article, we’ll explore:
What is the Post-Concussion Symptom Scale?
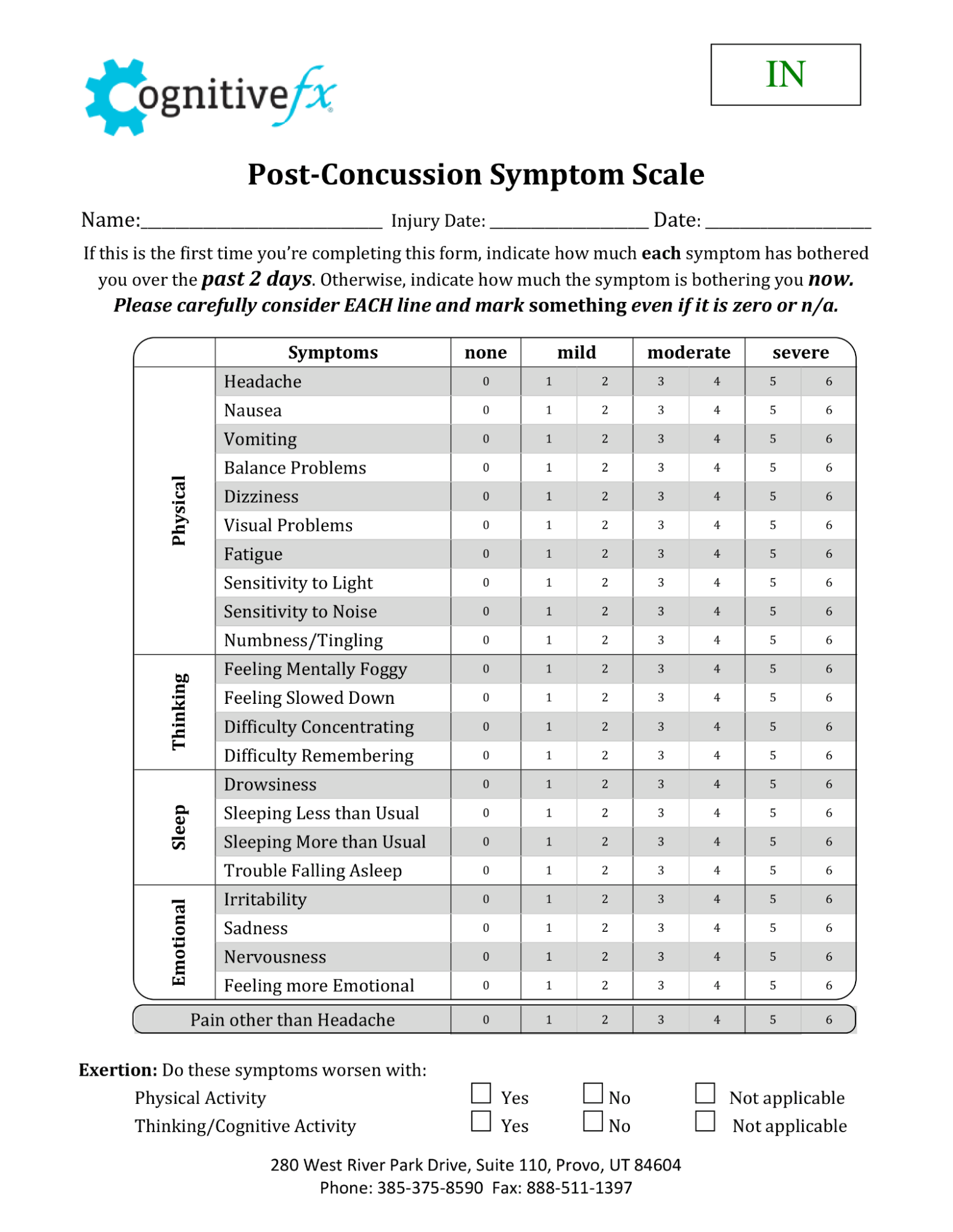
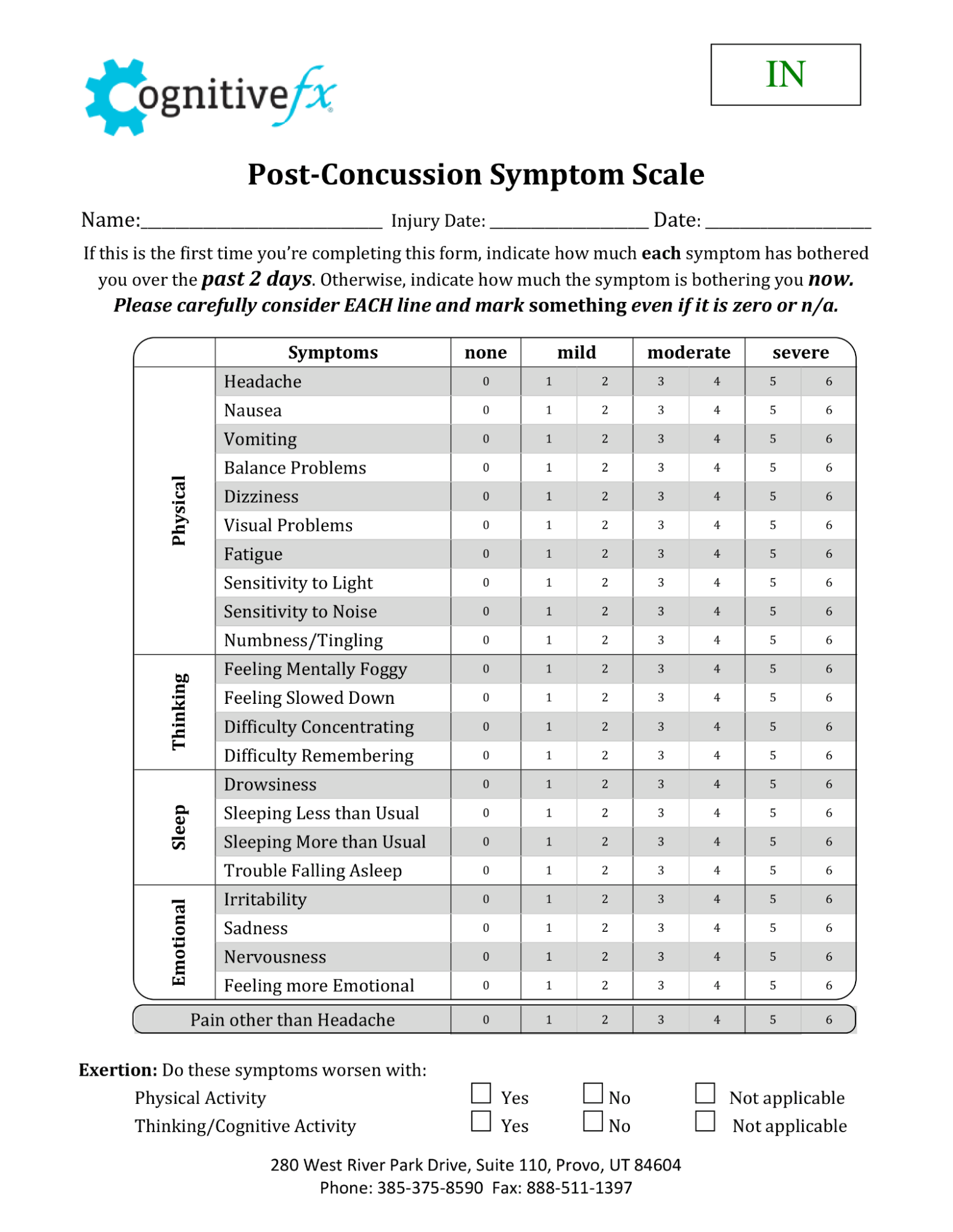
The PCSS is a 22-item self-report questionnaire that patients complete after experiencing a head injury. While commonly used in the SCAT5 protocol (Sport Concussion Assessment Tool 5th Edition) to assess sports-related concussions, it can be used as a diagnostic tool for any mild traumatic brain injury (mTBI).
-
Each symptom is rated on a 0–6 Likert scale (0 = none, 6 = severe).
-
The symptom score ranges from 0 to 132.
-
A PCSS score above 7 may indicate a concussion (especially if cognitive and emotional symptoms are present).
-
Higher total scores suggest more severe symptoms and a possible delayed recovery, whereas lower scores indicate milder injuries that will typically (but not always) heal more quickly.
To provide more nuance, the symptoms are often grouped into a 4-Factor Model:
-
Cognitive: confusion, difficulty concentrating, difficulty remembering, brain fog.
-
Physical (Somatic): fatigue, headaches, dizziness, nausea, blurred vision, sensitivity to light, sensitivity to noise, balance problems, etc.
-
Affective (Emotional): irritability, nervousness, anxiety, depression, sadness, feeling “off.”
-
Sleep/Arousal: insomnia, excessive drowsiness, or disrupted sleep patterns.
Since it was introduced, multiple studies have shown its accuracy and consistency in tracking symptom changes and predicting outcomes after a concussion.
Studies also show that this post-concussion symptom inventory can distinguish between concussed and non-concussed patients and identify patients with multiple concussions and pre-existing conditions.
For the majority of concussion patients, symptoms go away in six weeks or less. For others, persistent symptoms can lead to a condition known as post-concussion syndrome (PCS). Most of the time, post-concussive symptoms that do not disappear within three months will not go away without treatment.
This article covers all the basics of post-concussion syndrome, including diagnosis, treatment, patient stories, and more. Patients often have a mix of physical, cognitive, and emotional symptoms. You may have balance and memory problems, along with chronic pain from headaches and symptoms of depression. Another person might experience nausea and dizziness from physical activity, brain fog when they try to work, and increased anxiety.
That’s because PCS doesn’t look exactly the same in each person; different regions of the brain may be affected in different ways. Treatment of post-concussion syndrome (discussed below) is most effective when it takes those differences into account.
When and How PCSS is Used
The Post-Concussion Symptom Scale isn’t limited to one stage of care. Instead, it plays a role throughout the entire journey of concussion management—from establishing a baseline before injury, to supporting diagnosis, to monitoring recovery, and even predicting long-term outcomes.
Before a Concussion: Establishing a Baseline
In sports medicine, many athletes complete the PCSS at the start of the season. These “baseline” scores serve as a snapshot of their normal brain function. If a head injury occurs later, doctors and trainers can compare the new results to the pre-injury baseline. This comparison helps confirm the presence of impairments, guide return-to-play decisions, and track progress more accurately than relying on memory or subjective impressions alone.
Helping with Diagnosis
After a suspected concussion, patients often fill out the PCSS as part of the initial evaluation. A higher score may suggest a concussion. However, healthcare providers typically do not use the scale in isolation.
Because many of the symptoms overlap with other conditions, the PCSS must be interpreted alongside physical and neurological exams, cognitive testing, and the patient’s medical history. In practice, the questionnaire helps flag potential concerns and provides a framework for deeper clinical inquiry.
Tracking Recovery
During recovery, the PCSS is repeated at regular intervals. By comparing scores over time, clinicians can see whether symptoms are improving, holding steady, or worsening. This ongoing monitoring helps determine if patients are ready to return to school, work, or sports, or if further treatment is needed. For example, if the post-concussion scale shows persistent or worsening symptoms, it may indicate the need for more specialized interventions.
Predicting Long-Term Outcomes
Finally, the PCSS can provide early warning signs about who might struggle with prolonged symptoms. Patients with high scores—especially those dominated by cognitive and emotional complaints—are more likely to experience post-concussion syndrome (PCS). Recognizing this risk early allows healthcare professionals to recommend targeted rehabilitation.
Strengths of the PCSS
The PCSS has become one of the most widely used tools in concussion care because it’s both practical and effective. Patients can complete it quickly and without special equipment, making it practical in almost any setting—from a busy sports sideline to a doctor’s office or even a telehealth visit. Beyond convenience, the scale also improves consistency across different providers and settings, creating a common language for describing concussion symptoms.
Some of the most notable strengths include:
-
Simplicity and accessibility: The questionnaire is quick to complete and can be administered almost anywhere, even remotely.
-
Standardization: Using a common scoring system makes the measurement of symptoms easier over time and across providers.
-
Global recognition: Because it’s used worldwide, results are broadly understood in sports medicine and clinical settings.
-
Improved communication: The structured format helps patients, doctors, and therapists talk about symptoms more clearly.
These qualities have made the PCSS an invaluable part of concussion care and research, especially in sports medicine, where clear and rapid assessments are crucial.
Weaknesses of the PCSS
Despite its usefulness, the PCSS has clear limitations. Its biggest drawback is subjectivity: because it relies entirely on patients’ self-reporting, scores can be influenced by mood, motivation, or even external pressures. Without additional clinical testing, it’s impossible to know whether the numbers accurately reflect the patient’s true condition.
Other limitations include:
-
Limited range of symptoms: The PCSS focuses on 22 items, but many concussion-related issues (such as hormonal changes or subtle visual problems) fall outside its scope.
-
Lack of baseline data: If no pre-injury score exists, it’s difficult to judge how much the patient has deviated from their normal state post-injury.
-
Non-specific symptoms: Some common symptoms of concussion (e.g. headaches, fatigue, or sleep issues) can be caused by other conditions, which complicates interpretation.
In other words, while the PCSS is a valuable starting point, it cannot and should not be used as a standalone diagnostic tool. Instead, it works best when paired with other assessments that provide more objective measures of brain function.
How the PCSS Fits Into Our Evaluation & Treatment at Cognitive FX
At Cognitive FX, we specialize in treating the smaller subset of concussion patients whose condition develops into post-concussion syndrome (PCS). Our treatment program is unique from most other clinics in two key ways:
-
Use of Functional Neurocognitive Imaging (fNCI): Unlike CT and normal MRI scans, our advanced fMRI scan maps how different brain regions are functioning and communicating with each other. This allows our team to identify the exact areas of brain dysfunction for each patient and tailor treatment accordingly.
-
Coordinated multidisciplinary treatment under one roof: Many PCS patients have frustrating experiences piecing together care through different providers and therapists who don’t coordinate with each other. They often have to wait weeks between appointments, and progress is slow to nonexistent. At Cognitive FX, our multidisciplinary team includes a clinical psychologist, a neurosurgeon, a neuroradiologist, neuroscientists, neuromuscular therapists, cognitive therapists, occupational therapists, and others—all of whom coordinate closely to optimize care for each patient on an accelerated treatment schedule.
Note: We are also the only post-concussion clinic we know of with third-party validated, peer-reviewed outcome data showing that our treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants.
Patient Evaluation
The PCSS informs how we gain an initial understanding of our patients’ current symptoms when they come to us. This shared starting point helps frame conversations with patients and provides a benchmark we can revisit later in treatment.
However, because the PCSS is limited to self-reported symptoms, we combine it with a much more comprehensive evaluation. This ensures we capture both the subjective experience of the patient and the objective evidence of how their brain is functioning.
Our initial evaluation includes:
-
A meeting with one of our doctors to review the patient’s medical history and symptoms of post-concussion syndrome.
-
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
-
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
-
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
-
A brain imaging scan called Functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected by the injury.
The fNCI Scan
Instead of strictly conducting interviews with the patient about their symptoms, as you’d experience at most concussion clinics, we use an advanced fMRI scan to pinpoint exactly where the brain is showing signs of dysfunction.
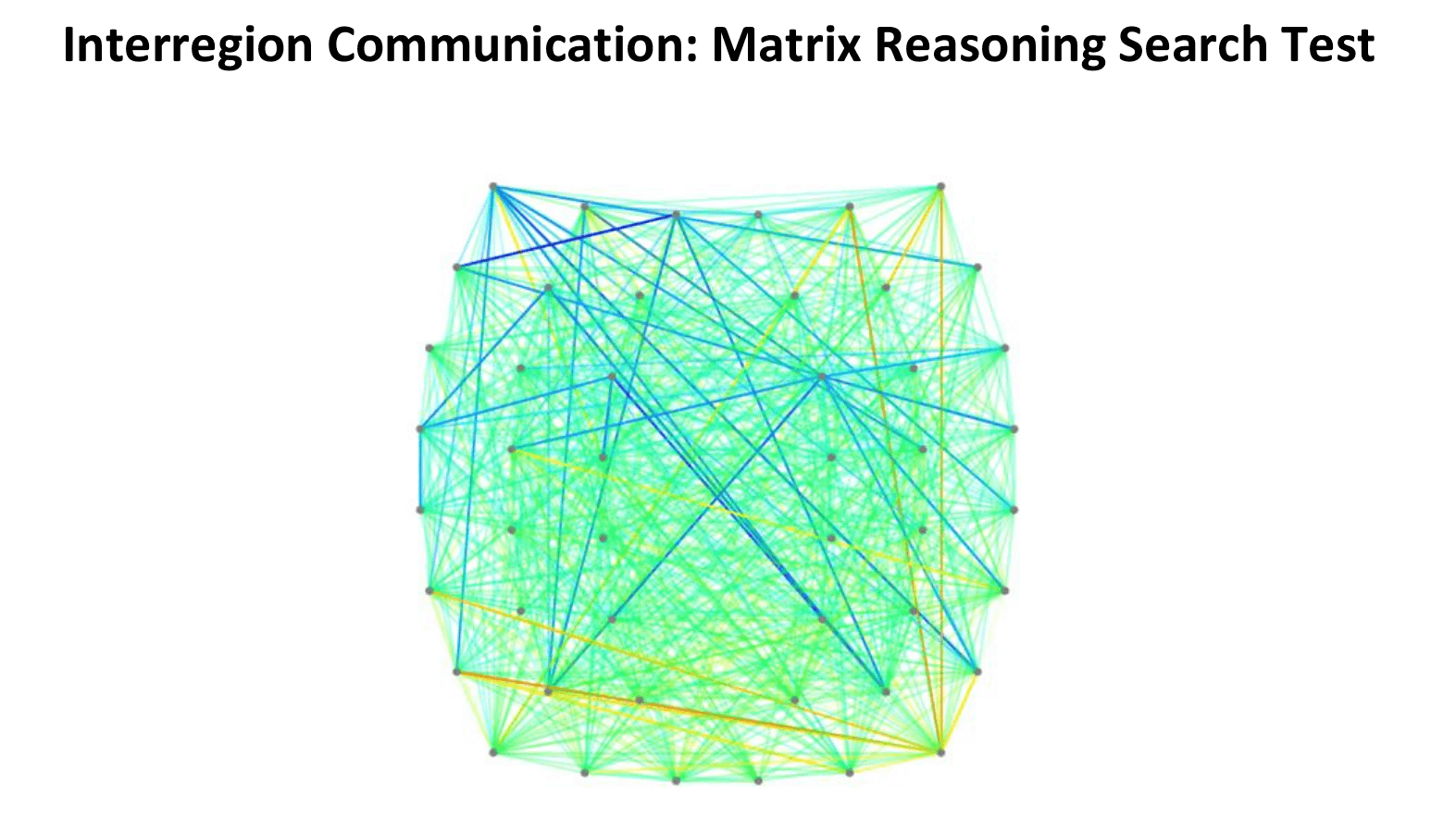
We use Functional Neurocognitive Imaging (fNCI), which measures two key things:
-
Regional brain activity: How much oxygen each brain region uses during specific cognitive tasks (indicating underactive, normal, or overactive function).
-
Connectivity between regions: How well different parts of the brain communicate with each other.
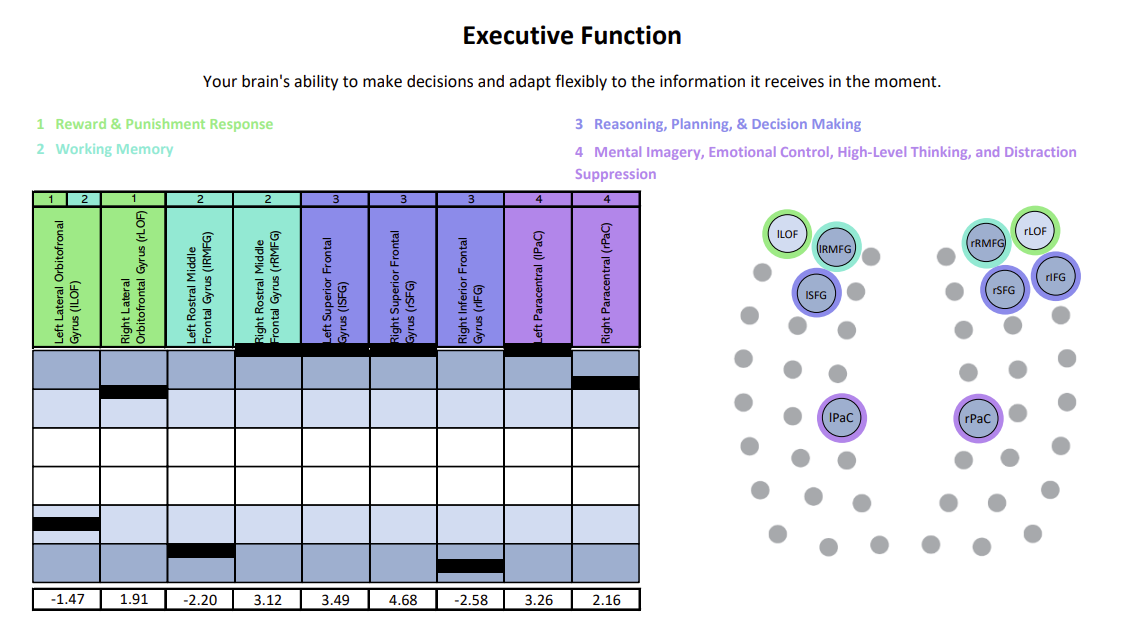
The scan results are visualized through intuitive charts and brain maps that help us identify whether a patient is experiencing hypoactivity (under-functioning), hyperactivity (over-functioning), or a mix of both—and where.
This detailed view of brain function allows us to tailor each person’s therapy precisely.
For example:
-
Someone with hypoactivity may need therapies that target various brain regions with stimulation and cognitive endurance training.
-
Someone with hyperactivity may benefit from therapies that reduce neural “noise” and promote regulation.
We’ve organized scan results for regional activity into six clear cognitive domains—like memory, attention, and executive function—to make them easier to understand and better guide individualized treatment.
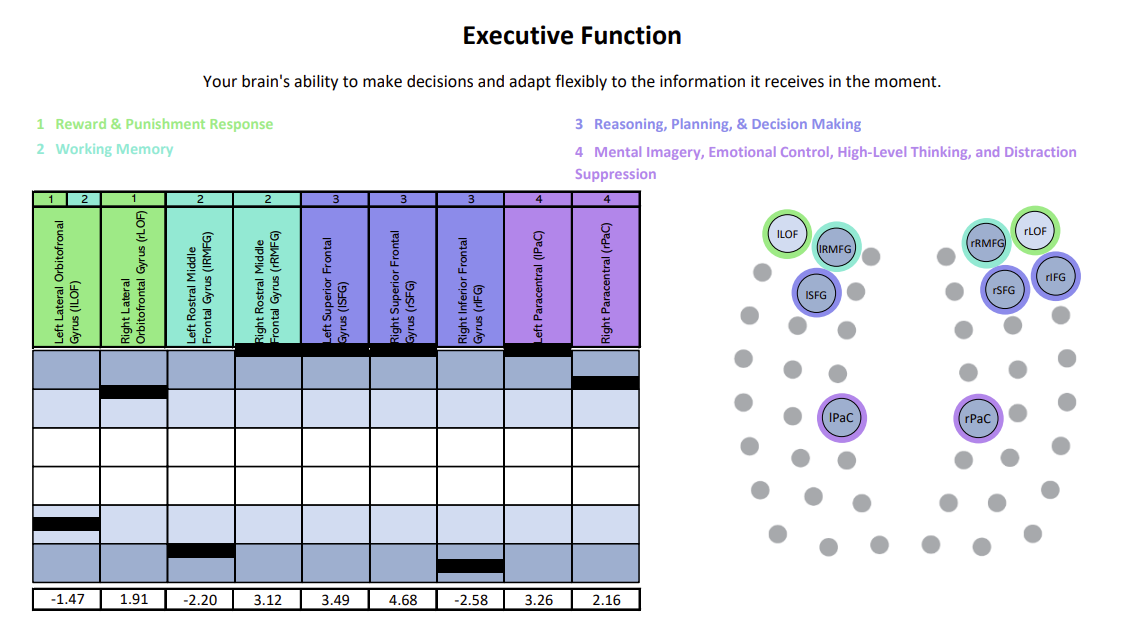
Each chart shows how specific brain regions are functioning compared to a normal brain. The white area represents the normal range, with the center line marking the average. Light and dark blue zones show increasing levels of abnormality. A black line marks the patient’s result for that region—ideally landing within the white. Lines in the light and dark blue zones suggest that region is either hyperactive (blue zones above the white) or hypoactive (blue zones beneath the white). In this example, the patient was experiencing both hypoactivity and hyperactivity within different key regions linked to executive function.
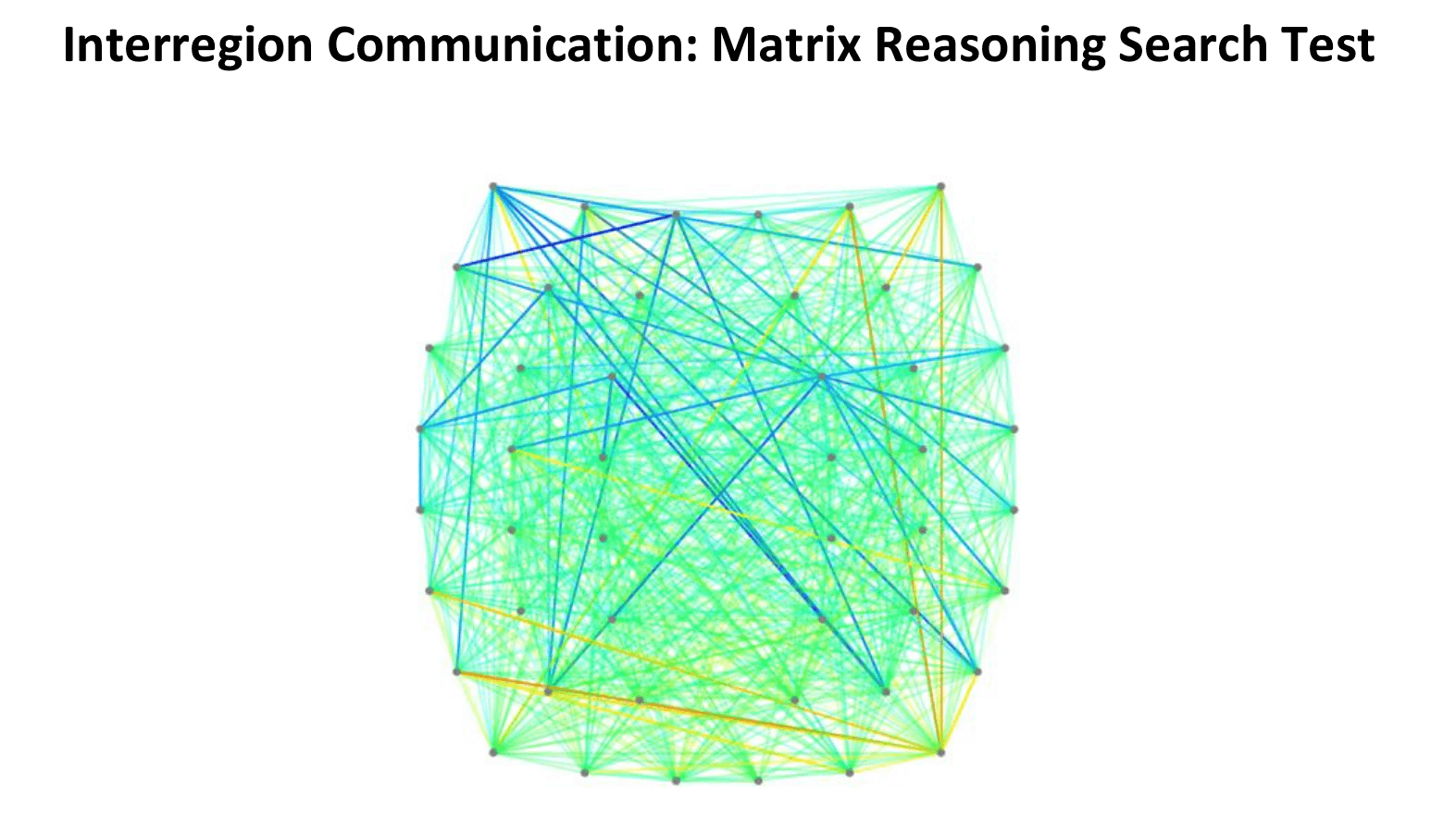
In this connectivity map, cooler colors (blues) indicate areas of hypoactivation (underactivity), while warmer colors (reds, oranges, yellows) indicate areas of hyperactivation (overactivity).
What Treatment Involves
After patients complete this evaluation, our team combines all the information and designs a customized treatment plan to target exactly the areas of the brain that show dysfunction for each patient.
Treatment for persistent post-concussion syndrome involves a three-step cycle that repeats: Prepare, Activate, and Recover.
Prepare

Therapy starts with short bursts of aerobic exercise, usually on the treadmill or stationary bike. As described earlier, exercise triggers the release of important chemicals in the brain, which help the patient's brain become more flexible and boost the effects of subsequent therapy.
Our therapists are trained to help patients exercise according to their needs without triggering severe symptoms. Even patients who struggle with physical activity due to balance problems can make remarkable progress in these sessions.
Activate

After exercise, patients attend a variety of therapies, including cognitive therapy, sensorimotor therapy, neuromuscular therapy, Dynavision therapy, occupational therapy, neurointegration therapy, vision and vestibular therapy, and psychotherapy, to name just a few. Patients receive all or most of these therapies during their visit, but the exact regimen for each one is unique to them.
Our therapists often combine exercises from different disciplines for greater effect.
For example, you might balance on a Bosu ball to engage your vestibular system and brain’s balance center while tossing color-coded tennis balls to work hand-eye coordination and reflexes. Meanwhile, you’ll add or subtract from a running tally based on which ball you catch, challenging memory, problem-solving, and attention.
During neurointegration therapy, you might draw a mirror image of a pattern while answering simple questions from your therapist.
Recover
Rest periods are an important part of our treatment. Some examples of scheduled brain breaks include:
-
Neuromuscular massage: Therapists massage the neck and shoulders to relieve chronic pain and tension, relax muscles involved in vision, improve circulation, and alleviate headache pain.
-
Brainwaves: The binaural beats app we use produces two frequencies that are very close together. If you listen to a different frequency in each ear, your brain will average them together to produce one frequency. We set the parameters so that the frequency your brain creates is the same frequency you would experience through meditation. This frequency will propagate in your brain waves as you listen. As a result, you gain some of the restorative benefits of meditation without being a meditation expert.
-
Mindfulness: Patients learn mindfulness techniques during their time at the clinic.
At the end of treatment, patients undergo a second brain imaging scan to check on their progress. They then meet with one of our therapists to review the results and receive a series of at-home exercises. These typically include physical activities, cognitive tasks, visual and vestibular exercises, and relaxation techniques. We recommend patients perform these exercises for about an hour, five times a week initially, with the frequency decreasing as symptoms improve.
For patients needing further therapy, we provide referrals to appropriate specialists.
Over 90% of our PCS patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.
Conclusion
The Post-Concussion Symptom Scale is a practical, accessible tool that helps clinicians capture the patient’s experience and monitor recovery after a head trauma. It’s not perfect—on its own, it cannot diagnose a concussion or predict the full scope of challenges a patient may face—but it remains an important part of a broader diagnostic process.
For most people, concussion symptoms fade within a few weeks. But for those who continue to struggle with lingering issues, post-concussion syndrome requires specialized evaluation and treatment. At Cognitive FX, we use self-reported symptoms alongside advanced brain imaging and a multidisciplinary approach to understand each patient’s unique challenges and guide their recovery.
If your symptoms haven’t resolved as expected, you don’t have to face them alone. Effective treatment is possible, and we’re here to help.