How Head Injuries Cause Vertigo Years Later
Vertigo is acommonsymptom after a mild traumatic brain injury (mTBI). Most patients describe it as feeling like either the room is spinning or they are.Almost halfof those who sustain a...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
After headaches, dizziness is the second most common symptom patients experience after a concussion. Although this symptom often resolves by itself, it becomes persistent and debilitating for some patients. If patients experience dizziness or other concussion symptoms for more than three months, they may have post-concussion syndrome (PCS).
Patients describe their dizziness in a variety of ways. Descriptions range from lightheadedness or unsteadiness to feeling like the room is spinning. Differences in what’s causing the dizziness may drive these varying experiences.
Understanding what is causing the dizziness is the key to recovery. Many factors — from post-concussion brain dysfunction to vision and vestibular issues — can cause dizziness. We’ll explore these and other major causes in this post, along with various treatment options.
In this article, we’ll cover:
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.

Dizziness is a common symptom of acute concussion and post-concussion syndrome. Some studies suggest that experiencing dizziness is predictive of prolonged recovery from a mild traumatic brain injury (mTBI).
Despite its prevalence, the experience of dizziness is not easy to define. Patients sometimes struggle to describe this symptom and may feel it differently from other patients with similar problems. Over the years, we’ve heard symptoms of dizziness being described in many ways by our patients, including:
Medically, the term dizziness is used to describe a sense of disorientation in space. Dizziness isn’t a disease by itself, but rather a symptom of something else.
Dizziness can be subdivided into 4 main subtypes: vertigo, presyncope, lightheadedness, and disequilibrium.
These feelings are often triggered (or worsened) by walking, standing up quickly, or moving your head. Some patients have to lie down to recover.
As mentioned earlier, dizziness can be accompanied by nausea and vomiting. Other post-concussion symptoms may include:

To understand dizziness, it helps to understand how the body keeps us balanced and coordinated when we move.
The main systems involved in this process include the vestibular system (inner ear), vision (movements of the eyes), and proprioception (body’s ability to sense movement). In addition, two areas in the brain called the brainstem and cerebellum process the information coming from these three input systems to coordinate a balanced and organized response.
The vestibular system, located in the inner ears, can detect our movements (forwards and backwards, side to side, and up and down). This system consists of a complex series of passageways and chambers within the skull. Within these passageways are tubes (semicircular canals) and fluid-filled sacs (a utricle and saccule).
The semicircular canals are located roughly at right angles to one another, and each one corresponds to one dimension in a 3D space. These canals send information to the brain about how quickly and in what direction the body is moving. When the vestibular system on both sides of the head is functioning properly, it sends complementary and matching information to the brain.
The second part is the vestibule, which is formed by the saccule and utricle. In simple terms, these structures provide information about gravity and linear acceleration thanks to small calcium crystals located inside the saccule and utricle. This includes, for example, going up and down in an elevator or traveling in a car, respectively.
The visual system tracks where the body is in space and in what direction it is moving. As we move, our brain reassesses our relationship with objects in our vicinity. For example, if an object seems to be getting smaller, the brain “understands” that it’s because we’re getting further away.
There is also a complex system of communication between the visual and the vestibular systems; this is called the vestibular-ocular reflex (VOR). This ensures that when your head moves, your eyes can automatically stay fixed, avoiding blurred vision. That way, when you walk, your head may move up and down but your visual field remains constant.
The proprioceptive system — briefly, formed by sensors in the skin, bones, and muscles — tells the brain which part of the body is touching the ground and which parts (if any) are moving. This allows the body to maintain a stable upright position balance when moving.
As described above, the three elements of the balance system send signals to each other and to the brain about body movements.
If the system is operating normally, the brain receives consistent information from all components and generates coordinated movement accordingly.
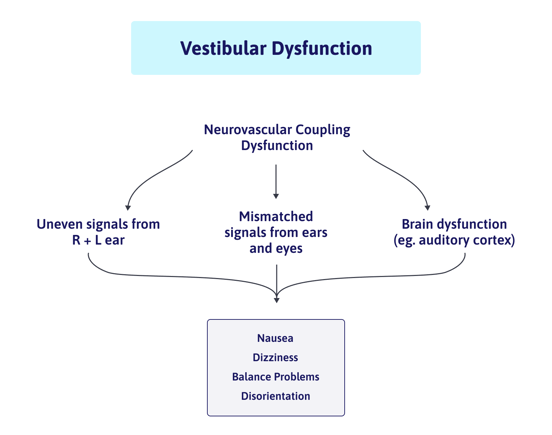
Dysfunction or impairment in one of these systems after a mild head injury can create instability. For example, vestibular issues may cause the ears to send a stronger signal from one side than the other. If one side is sending one message to the brain, and the other side doesn’t quite send the same message, then it may cause dizziness and lightheadedness.
Curiously, the parts of the brain involved in this process also interact with the parts of the brain that can trigger nausea and heart rate changes, which explains why problems with balance can also create additional symptoms.

Some patients experience dizziness immediately after a concussion or whiplash, while others begin to feel it a few days later. If the head injury affected multiple areas in the brain, patients may only feel the most severe symptoms at first. While the impact on vestibular and/or visual systems is present immediately after the head trauma, patients may only feel dizzy a few days later as the brain deals with more serious symptoms. Your brain needs to prioritize what needs to be “fixed” first, and vestibular issues may not be at the top of the list. This phenomenon is sometimes present during treatment as well; patients who make great strides in therapy may start to notice dizziness only after the severe headaches resolve, for example.
About 90% of concussion patients will stop feeling dizzy within a week or two after the injury (although they may continue to experience other symptoms), but a small proportion of patients will still experience dizziness (and other symptoms) for months or even years afterwards.
For some patients, dizziness is a constant feeling that can happen when they’re moving, standing still, or even lying down. For others, symptom onset coincides with a particular activity, such as exercising or being in a car.
Dizziness can have many possible causes. In most PCS patients, it’s likely that more than one factor is at play. These are the most common causes for dizziness in post-concussion syndrome patients:
Dizziness can be caused by dysfunction of the autonomic nervous system.
The autonomic nervous system (ANS) is part of the nervous system and operates without us even noticing it’s there. It includes the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which regulate vital body functions such as blood pressure, heart rate, sweating, and breathing rate. Faulty regulation of the ANS — called dysautonomia — leads to autonomic symptoms, such as dizziness, vertigo, and imbalance.
For example, ANS dysfunction causes problems with breathing and blood pressure. Your body may incorrectly perform the minute adjustments needed to blood pressure (BP) when you sit down or stand up. It overreacts and increases or decreases BP too much, which in turn causes dizziness and lightheadedness.
Further reading: The Patient’s Guide to Post-Concussion Autonomic Dysfunction (Dysautonomia)
As described earlier, maintaining balance involves two areas in the brain: the brainstem and the cerebellum. Not surprisingly, if the brain injury affected either of those areas or the cranial nerves that connect the vestibular and visual systems to these areas, you might experience posttraumatic vertigo or lightheadedness.
Concussion can disrupt the relationship between nerve cells in the affected areas and the surrounding blood vessels. In a healthy brain, nerve cells receive what they need (nutrients and oxygen) from a network of blood vessels in a dynamic relationship called neurovascular coupling (NVC).
However, concussions can disrupt this mechanism, resulting in areas that no longer function normally. When these regions experience NVC dysfunction, it leads to many of the physical and cognitive symptoms you experience, such as headaches, brain fog, difficulty tracking conversations, and dizziness, to name just a few.
Neurovascular coupling dysfunction is one of the core causes of concussion deficits and is a key area of focus at our post-concussion treatment center, Cognitive FX.
Further reading: What is neurovascular coupling?
Your dizziness may also be caused by a mismatch between visual and vestibular systems. This is called a visual-vestibular mismatch.
In simple terms, it means that your brain is getting conflicting information because the information coming from your eyes does not match the information coming from your ears. Without reliable information, the brain has a hard time figuring out which is moving: you, or the things around you.
A good example to demonstrate this mismatch is when you’re sitting at a red light and the car next to you starts to move. For a split second, your brain thinks that your car is moving and you instinctively press the brake. This mismatch between vision (you see the other car moving) and vestibular (your inner ear does not detect movement) causes your brain to play a trick on you, telling you that you’re moving when you’re still stopped. In a healthy brain, these moments are harmless and dissipate quickly, but PCS patients with this type of dizziness experience this feeling frequently.
This mismatch can be triggered by anything that overwhelms your vision. Common situations may include:
Affecting more than half of post-concussion patients with dizziness, the most common vestibular disorder after a concussion is Benign Paroxysmal Positional Vertigo (BPPV). Patients suffering with BPPV often describe their dizziness as if they’re in a merry-go-round. This is called rotary vertigo, and it typically happens with specific movements, such as sitting up in bed, bending down to pick something up, or a sudden head movement.
This condition develops when the calcium crystals — which should be located in the vestibule — move into your semicircular canals and get trapped inside. When your head position changes, these small particles move around the semicircular canals and send confusing information to the brain.
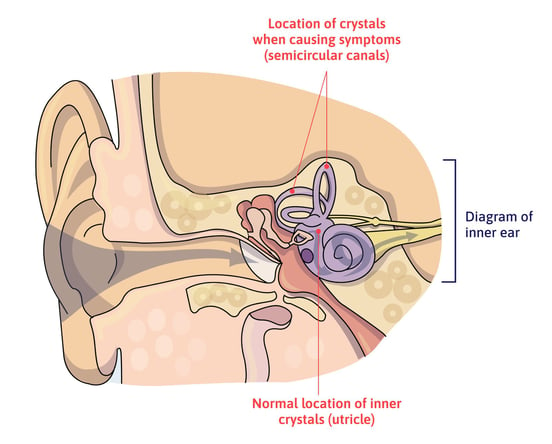
Many cases resolve without treatment, but patients with persistent symptoms may need a technique called the Epley maneuver (or another canalith repositioning maneuver) to dislodge the crystals from the canals and return them to the vestibule.
Feeling dizzy or lightheaded is a side effect of many prescription drugs. For example, medications to control blood pressure and low blood sugar levels can trigger dizziness. Not surprisingly, the more medication you take, the higher the chances of triggering dizziness.
Further reading: Medication for post-concussion syndrome
Not all cases of dizziness are caused by visual or vestibular problems. Sometimes, patients describe feelings of mild imbalance, lightheadedness, or other hard-to-describe feelings which may indicate other disorders. For example, around 10% of patients experience post-concussion pituitary dysfunction, which can cause dizziness. If your symptoms persist for a long time despite treatment, consider getting an appointment with an endocrinologist, a neurologist, or another healthcare provider for a full hormone analysis.
Further reading: Post-concussion hormone dysfunction
Note: While it’s unclear whether post-traumatic stress disorder is causative of dizziness, patients who have PTSD often also suffer from dizziness and related symptoms. Learn more about PTSD and concussions here.

Although symptoms are similar, sometimes it’s possible to differentiate between dizziness caused by vision issues versus vestibular woes.
If the problem is vision-related, patients often wake up feeling fine in the morning after a good night's sleep, but symptoms begin and increase as the day goes on. In contrast, if it’s a vestibular-related issue, patients might feel dizzy and off balance when they wake up, but as the vestibular system activates, they feel better until they take actions that trigger symptoms again.
When traveling in a car, patients with vision problems more often prefer to be a passenger than to drive because driving is a visually demanding task and they need to pay constant attention to their surroundings. In contrast, patients with vestibular problems prefer to be the driver because they can focus on the road and know what motions to expect (slowing down, speeding up, turning, and so forth).
With regards to vestibular problems in general, it’s also possible to differentiate between problems in the inner ear itself versus in the areas in the brain that process the information. If the problem is in the inner ear, onset tends to be sudden and very often patients remember exactly when it started. In contrast, if the problem is in the brain, symptoms develop slowly and patients are not able to pinpoint exactly when it started.

Since every patient is different, our treatment process starts with a detailed and in-depth evaluation with our team. This includes a review of your medical history, an assessment of your symptoms, and a series of physical exams, including a close examination of your balance and posture.
We also have access to state-of-the-art brain imaging technology to determine exactly how the concussion affected your brain. This tool is called functional Neurocognitive Imagining (fNCI), and it shows which regions in the brain are suffering from neurovascular coupling dysfunction. In practical terms, it looks at blood flow dynamics in 56 different areas in your brain, as well as how these areas communicate with each other.

We also use structural MRI to check for brain and neck injuries that go beyond the scope of concussion.
After the initial evaluation, our therapists combine the results from the scan and the medical review to design a custom-made treatment plan for each patient. We call our treatment program Enhanced Performance in Cognition, or EPIC for short.
During treatment, you’ll follow a three-step process to ensure your brain can cope with the demands of treatment:

You’ll go through this three-step sequence repeatedly during the week(s) to restore healthy neurovascular coupling, recover ANS function, and eliminate (or at least reduce the incidence) of physical and neurological symptoms, including dizziness.
Our program includes multidisciplinary therapy sessions, including cognitive, sensorimotor, neuromuscular, occupational, vestibular, vision, and physical therapy, among others.
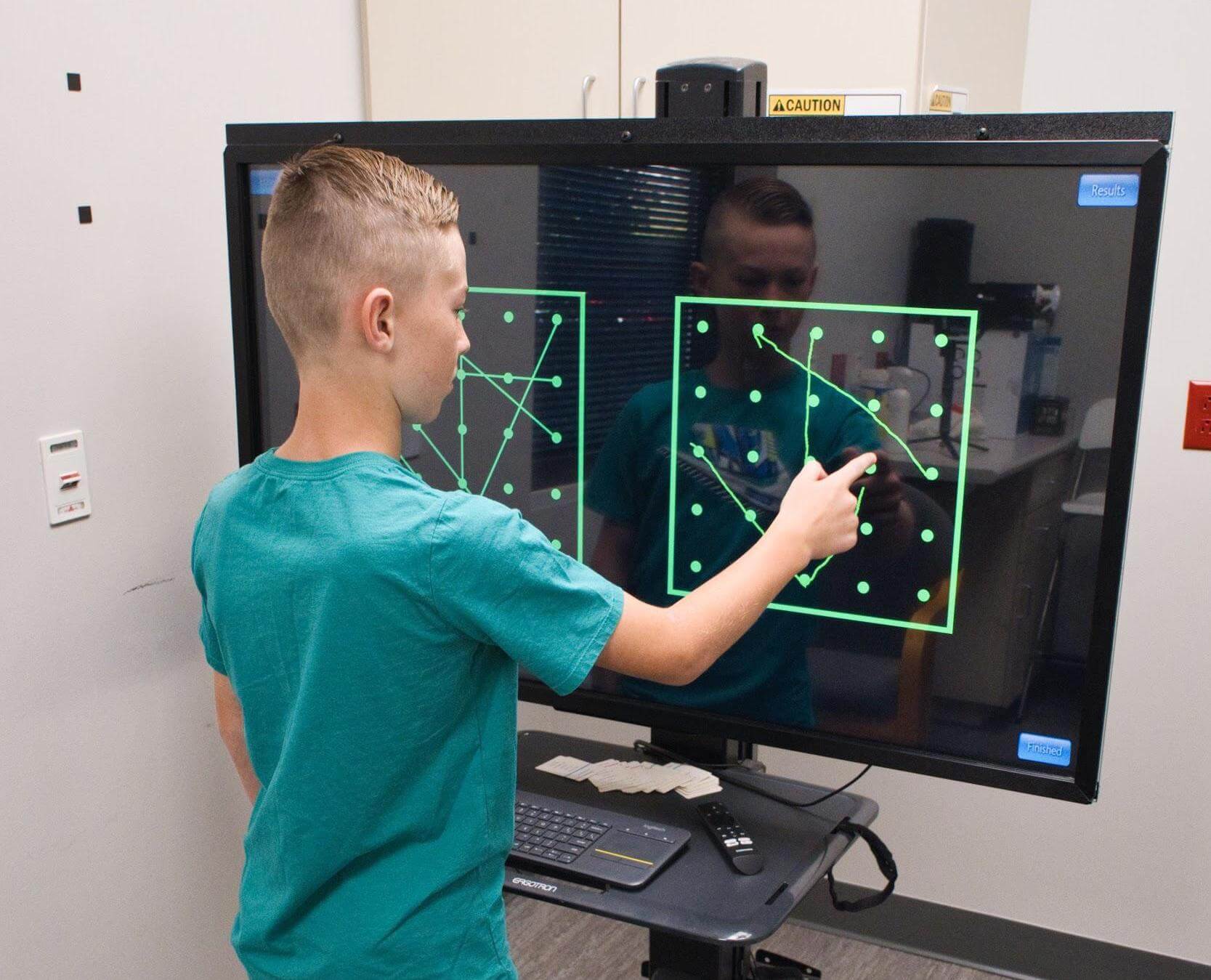
Neurointegration therapy is where we address dizziness the most directly. During that time, your therapist will lead you through exercises to help your vision and vestibular system recover and communicate better with each other and the brain.
For vision, you might do eye tracking, gaze fixation, eye saccades, eye movement exercises, and the Brock string (which helps your eyes to work together and focus on objects at different distances).
Vestibular rehabilitation therapies might involve gaze stabilization exercises like nodding “yes” or shaking your head “no” while focusing on a letter on the wall. While many clinics only treat the left and right ear equally, we differentiate between the level of dysfunction in each ear. Our therapists assess each semicircular canal and each side separately. If they find a specific problem with a particular canal, patients may need to do “half no” or “half yes” exercises: not a full nod or shake with the head, but short movements to the left/right, up/down, or diagonal with just one side of the head.

We also integrate therapy for the vision and vestibular systems. At this stage, you’ll step inside a device called the Maverick, which is shaped like a giant diamond. In each vertice there’s a light and a letter or a number. Patients need to follow a particular sequence by touching each light; the aim is to integrate head and body movement to get all the systems “talking” to each other in a healthy way.
If you’ve tried both vision therapy and vestibular therapy with limited success, neurointegration could be the missing piece you need for the vision and vestibular systems to work together again.
If that’s the case, why not schedule a consultation with Cognitive FX to see what we can do for you? We offer integrated therapies from numerous disciplines all under one roof, and our treatment is informed by careful assessment of your physical state and your brain imaging results. There’s no other clinic in the world that can offer such a comprehensive treatment for post-concussion syndrome.

You can’t always stop the feeling of being dizzy, but there are some steps you can take at home to lower the frequency of dizzy spells and minimize the risks to you until you’ve completed treatment. For example:
90% of our patients show symptom improvement after just one week at our clinic. To see if you are eligible for treatment, sign up for a consultation.

Andy is a Certified Athletic Trainer (ATC) and Z-Health Performance Master Trainer. He began his career in Orthopedics, then worked as Head Athletic Trainer and Director of Human Performance at a specialty physical therapy clinic. Here, his passion for innovative human body approaches ignited. In 2010, he founded Fitness Evolved in Berkeley, CA, focusing on a neurologically informed health and exercise paradigm. Andy mastered the Z-Health Performance Solutions system, creating brain-centric training and rehab at Fitness Evolved, serving diverse clients, including pro athletes and brain injury survivors. He's an accomplished Z-Health instructor, having trained professionals worldwide. Andy is thrilled to join Cognitive FX, contributing to our revolutionary concussion and TBI recovery techniques.

Vertigo is acommonsymptom after a mild traumatic brain injury (mTBI). Most patients describe it as feeling like either the room is spinning or they are.Almost halfof those who sustain a...

Eye twitching is typically mild and short-lived, but for some patients with post-concussion syndrome (PCS), it can become a persistent and uncomfortable symptom. While often overlooked, eye twitching...

Balance is a complex physiological process involving multiple systems in the body, which can be easily disrupted following a concussion. Between 40 and 60% of patients experience balance and...

Dizziness. Nausea. Balance problems. Car-sickness. These are a few of the unpleasant symptoms of vestibular dysfunction after a head injury. Fortunately, they don’t have to be permanent; most...

Tinnitus—a buzzing, hissing, or ringing in the ears—is a common and frustrating symptom after a mild traumatic brain injury (mTBI). While it often resolves within days, for some patients it lingers...

Whiplash can cause physical and neurological damage that results in long-term symptoms. In addition, the same event that caused whiplash could also have caused a concussion. (The sudden motion can...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY