Severe traumatic brain injury (TBI), concussion (mild traumatic brain injury or mTBI), and other head trauma can cause high blood pressure, low blood pressure, and other circulatory system changes. Head injury may disrupt autonomic function (leading to a condition known as dysautonomia), which in turn can cause blood pressure dysfunction and other symptoms to persist for months or years after the injury. Some patients experience a particular type of dysautonomia known as postural orthostatic tachycardia syndrome (POTS), which we discuss further in the post.
In our post-concussion clinic, we treat patients with symptoms that persist for months or even years after a head injury, a condition known as post-concussion syndrome (PCS).
Some of them have surprising symptoms related to blood pressure changes. They wonder if they’re going crazy because they haven’t heard of these symptoms stemming from concussion before and can’t find information about their condition before arriving at our clinic.
So in this post, we hope to remedy that difficulty. We cover what’s happening to your body and what types of treatment are available, including:
If you've experienced one or more concussions and your symptoms persist, you're not alone—and you're not imagining it. Help is available. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, schedule a consultation.
How Blood Pressure May Change After Concussion

In a healthy body, blood pressure works to achieve homeostasis between the amount of blood in an area and the localized need for what the blood is transporting. In other words, it tries to maintain “normal” no matter what activity you’re performing. It accommodates rapid changes such as bending over or breathing heavily, adjusting based on local signals from nerve bundles called baroreceptors.
Your blood pressure is designed to keep the right amount of oxygen, electrolytes, white blood cells (WBCs), and other micronutrients in your tissues at all times. It increases or decreases via vasodilation (blood vessels expanding) and vasoconstriction (blood vessels shrinking).
Vasodilation and vasoconstriction — and by extension, blood pressure — are governed, in part, by the autonomic nervous system. When you have dysautonomia, normal signaling can be skewed.
Think of blood pressure regulation like the fuel gauge in your car: When everything’s working properly, you know when the tank is full and when it’s empty. Imagine the chaos if the meter showed a full tank of gas when you started driving, but it was actually almost empty! Or, if it looked empty, but when you tried to fill the tank, it overflowed with gas.
Similarly, if dysautonomia causes a mix-up in your body’s signaling, you may have high blood pressure when you need it to be lower, or low when you need it high, and so forth. And that could happen throughout your body or in specific areas.
That’s the key to understanding these commonly asked questions about blood pressure.
By the way — some people mistakenly think that long-term symptoms only stem from a severe brain injury or from a concussion that caused loss of consciousness. You don’t have to have a severe head injury to have long-lasting symptoms. Many of our patients had seemingly mild head injuries, only to have serious symptoms until receiving treatment.
Can a Concussion Cause Low or High Blood Pressure?
Yes. Dysautonomia could drive blood pressure up or down after a concussion. One of our patients had a healthy average blood pressure that doubled after a head injury. Another had hypertension (high blood pressure) before injury that dropped to a normal range after the injury. Some see an increase or decrease only in their systolic reading, some in diastolic, and some in both.
We’ve even seen patients with different blood pressure readings on each half of their bodies!
In addition, low or high blood pressure is often situational. Some patients present with post-concussion exercise intolerance that results from dysfunctional blood pressure homeostasis and other symptoms and changes that come with the injury.
For example, maybe you try to go for a run, which requires an increase in blood pressure to push oxygen-rich blood through the body. It doesn't come, and then you feel awful. Or, perhaps you try to exercise, only to find your blood pressure dropping in response, causing a pounding headache, dizziness, and nausea.
Both concussion and severe TBI patients may have blood pressure changes immediately after injury. It’s clear that hypotension following injury worsens patient outcomes if untreated, but it’s unclear whether hypertension is good or bad immediately following injury. In either case, make sure you see a doctor immediately if you injure your head and notice a sudden change in your blood pressure.
Can a Concussion Cause a Flushed Face?
Yes, a concussion can cause a flushed face. What we call a “blush” is actually vasodilation just beneath facial skin. Some patients have a flushed face when the ANS mistakenly dilates those blood vessels.
You might see other skin changes (such as drained, splotchy, changes with exercise, etc.). It might even cause rashes. One of our patients would get a large patch of flushed skin from the shoulder through the chest whenever their dysautonomia symptoms were about to increase.
Can a Concussion Cause Fainting and POTS?
Yes, a concussion can lead to fainting and POTS (postural orthostatic tachycardia syndrome). This happens if the blood pressure and heart rate changes are tied to posture changes (sitting vs. lying down vs. standing). Concussion-related dysautonomia could result in several posture-related issues, including:
- Orthostatic hypotension (low blood pressure while standing).
- Orthostatic hypertension (high blood pressure while standing).
- Orthostatic tachycardia (increased heart rate while standing).
Key POTS symptoms occur from orthostatic tachycardia, which is your heart’s attempt to counteract orthostatic hypotension (lowered blood pressure while standing). If you have orthostatic intolerance, you might experience lightheadedness, fainting, and heart palpitations when you stand quickly after lying down or sitting.
POTS is a common diagnosis, even if you haven’t taken a tilt-table test (considered the standard for POTS or neurocardiogenic syncope diagnosis). But it’s somewhat lacking because it’s only based on cardiovascular anomalies, which don’t explain the many symptoms that come with it, such as anxiousness, brain fog, blurry vision, sleep problems, and fatigue. These are all post-concussion symptoms.
If you begin experiencing common POTS symptoms after a head injury, there’s a strong possibility you have post-concussion syndrome with resulting autonomic dysfunction.
It’s important to treat any neurological issues that may be contributing to your symptoms.
Note: Some doctors use the labels “POTS” and “dysautonomia” interchangeably, though it’s most accurate to think of POTS as a type of dysautonomia.
What Other Blood Pressure-Related Symptoms Might You Experience?
Here are a few other issues we’ve seen in patients that are related to dysautonomia and blood pressure changes after a head injury:
- Problems with extremities. This can present as Reynaud’s syndrome, always-cold fingers and feet, peeling skin or lesions on fingers and toes, or loss of fingernails due to lack of oxygen (hypoxia) in your fingers and toes.
- Decreased blood flow in the GI system. This can result in GI upset, food sensitivities, bloating, constipation, and even liver inflammation.
- Headaches and sinus pressure.
- Burst blood vessels in the eye.
- Sexual dysfunction. Males may suffer from erectile dysfunction; females from vaginal dryness and decreased arousal.
Concussion and Dysautonomia Go Hand in Hand

Researchers have established a link between concussion and dysautonomia. This comes as no surprise to us because many of the patients we treat in our post-concussion clinic present with symptoms of head injury and dysautonomia.
Dysautonomia is a dysfunction in the autonomic nervous system (ANS). The ANS reaches into nearly every organ system in the body, so it causes wide-ranging and often confusing symptoms when something goes wrong.
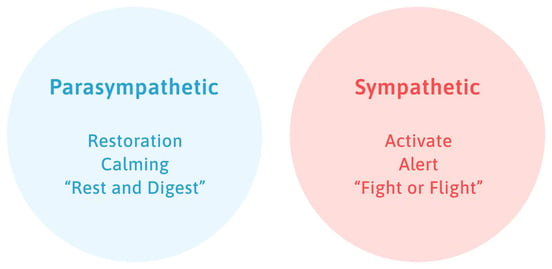
Two prongs of the ANS — the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) — balance each other out in a normal functioning ANS. The SNS handles your response to perceived threats (think fight or flight response); the PNS calms things down (think rest and digest).
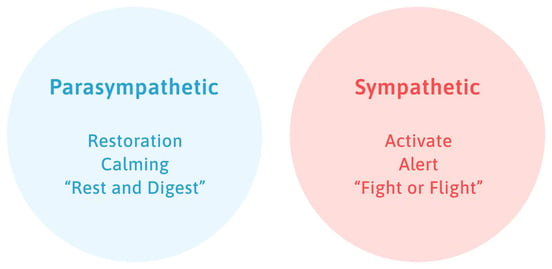
After injury, many patients have an ANS that is strongly skewed toward the SNS. They may feel neck and shoulder tension, anxiety, stronger reactions to stimuli like a shattering plate or a horror movie, and so forth.
You can read more about dysautonomia and what symptoms it causes here.
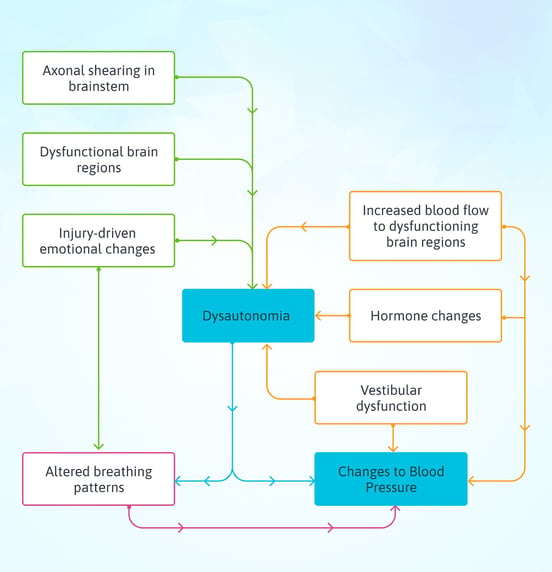
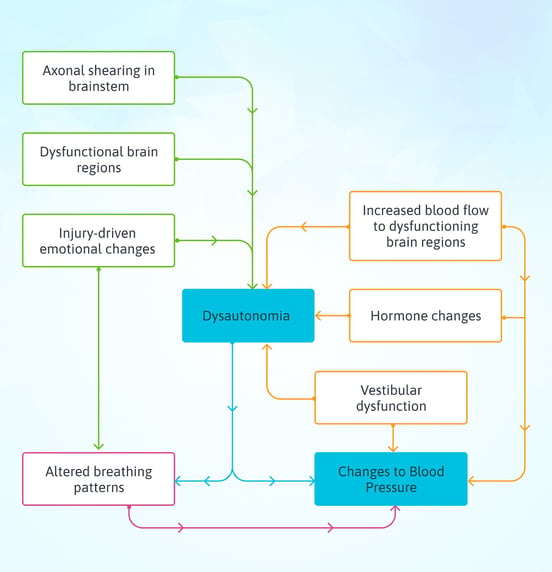
So what does this have to do with blood pressure changes? Many post-injury blood pressure changes are tied to dysautonomia. But how head injury leads to dysautonomia, which leads to dysfunctional blood pressure, is like a Rube Goldberg machine: Extremely complicated.
Plus, not every factor is present in every patient. Here is a very rough overview of common causes of blood pressure dysfunction after a head injury:
- Mild damage to nerves (axonal shearing) in the brainstem, where the ANS command center is located (note that this is especially common in whiplash injuries).
- A sharp increase in blood flow demanded by the brain, confuses the ANS and results in changes throughout the body.
- Dysfunction in the brain region that interacts most closely with the ANS (the anterior insula, which is hypoactive for many of our patients).
- Post-injury emotional changes such as anxiety, depression, and PTSD can reinforce ANS dysfunction.
- Altered hormone levels after injury (please have your hormone levels checked if you have lingering symptoms after a head injury).
- Vestibular dysfunction (problems with your body’s ability to sense where it is in space after the injury).
- Altered breathing patterns (from the post-injury autonomic dysfunction), which in turn affect the dilation and contraction of blood vessels throughout the body.
You might be surprised to see emotional changes on the list of causes. The ANS and our emotions affect each other strongly. Your dysautonomia could trigger feelings of anxiety, and feelings of anxiety could worsen the dysautonomia. They’re closely connected, which is why some patients find therapy from a psychologist helpful in addition to traditional treatment interventions. This association is also why some doctors mistakenly diagnose only a mental health disorder while failing to notice the dysautonomia.
This is not to say that your mindset “causes” the symptoms you experience. But your thinking patterns and feelings can be caught up in a web of symptoms that only the right therapies and time can untangle.
If you’d like to discuss your symptoms, their possible causes, and your treatment options, schedule a call with our team.
Treatment for Concussion and POTS Symptoms

Many POTS patients are told that their condition isn’t treatable. They might be advised to drink more water, increase their salt intake, and reduce stress. But beyond that, they’re often given very little assistance.
Successful POTS treatment depends on the cause. If the cause is nerve death, it’s not treatable. If it’s from an increase in norepinephrine (from hyperadrenergic POTS), then there are some pharmacological solutions. And if it’s a secondary response to injury, then it can be treated with the same methods that post-concussion syndrome and post-injury dysautonomia are treated with.
Before we jump into those treatment methods, know that certain SNRIs may cause common post-concussion and POTS symptoms. Common drugs for depression, anxiety, obsessive-compulsive disorder, social phobia, migraines and headaches, chronic pain, and fibromyalgia fall into this category. If your symptoms started or worsened after you began taking an SNRI, tell your health care provider and investigate alternative medications.
Therapy for Concussion and Dysautonomia
If your symptoms arose after a severe or mild traumatic brain injury (or another brain trauma, such as serious illness or carbon monoxide poisoning), then it’s important to treat the root cause of symptoms: brain dysfunction and dysautonomia.
At CognitiveFX, we start with a functional neurocognitive imaging (fNCI) scan, which looks at cerebral blood flow in over 60 brain regions. This shows us which areas likely suffered impairment of healthy brain function. We can then provide multidisciplinary treatment targeted to the unique needs of each patient.
Each patient receives neuromuscular therapy, cognitive therapy, occupational therapy, sensorimotor therapy, vestibular rehabilitation, and more. You can read more about why this helps post-concussion patients here.
Some of the specific techniques we use to help patients with dysautonomia include:
- Physical therapy and physical activities designed to help your ANS function better.
- Breathing techniques.
- Meditation/mindfulness training.
- Two or more sessions with a psychologist.
- Therapies that target the anterior insula (which is activated whenever you exercise impulse control).
- Brainwaves (auditory pattern to help you destimulate between therapy sessions).
Will treatment for post-concussion syndrome erase all your symptoms? It’s possible. But it’s more likely you’ll experience rapid improvement of some symptoms and a longer recovery journey for others. Each patient is unique, and some issues take longer to resolve than others.
For example, your ANS might recover during treatment week, but if you still have vision problems, you might still have ANS-related symptoms from those vision problems until you complete your vision therapy course.
Note: We accept patients with a history of head injury or other significant trauma. We are only equipped to help patients make progress with dysautonomia that stems from an injury (and that does not involve nerve death). We are not well equipped to help dysautonomia patients without that history of injury, as the cause may not be something we can treat.
What You Can Do
Finding treatment providers who take you seriously is key to making progress. If your doctor dismisses your concerns, find one who will listen to you. If your doctor runs out of ideas, ask for referrals to a new one.
In the meantime, whenever you experience a symptom that might be related to your injury, write it down — even if it feels crazy. Dysautonomia can cause unexpected symptoms! But that information will come in handy when you’re being evaluated for treatment.
Every week, we help post-concussion patients recover from persistent symptoms. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, schedule a consultation.