A Patient’s Guide to TBI Physical Therapy
Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Dizziness. Nausea. Balance problems. Car-sickness. These are a few of the unpleasant symptoms of vestibular dysfunction after a head injury. Fortunately, they don’t have to be permanent; most patients make rapid improvement with a good therapist.
The vestibular system, which helps your brain determine your position in space, is one of several systems in your body that can become dysfunctional after a head injury. Others include your brain itself and the autonomic nervous system (which may also contribute to symptoms such as nausea).
While many people feel better within two weeks after their concussion, up to 30% of concussion patients have persistent symptoms that last months or years after their injury. This condition, known as post-concussion syndrome, can develop after any mild traumatic brain injury (mTBI) and may include lingering vestibular issues.
Vestibular therapy is one of many therapies we provide at our clinic for patients with post-concussion syndrome; while it’s not enough to resolve all concussion symptoms, it will help with issues that stem from vestibular dysfunction. In this article, we explain:
If you’re experiencing persistent symptoms after a head injury, you’re not alone. And there is hope for recovery. 95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. To learn more about getting treatment, schedule a consultation with our team.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
The vestibular system is what your brain uses to determine your location in space. It’s a tiny organ located in your inner ear. Both sides work together to keep you balanced and help your vision stay clear. Your vestibular system, body (via the proprioceptive system, which is the body’s awareness of where it is in space), and eyes all send information to your brain, which interprets the data. As a result, you understand your position relative to everything else around you — the coffee cup on your desk, the cat walking by, the trees swaying outside the window. You know what’s up, down, left, right, far, and near.
Think of it like neural GPS: Your brain is the phone, and your eyes, ears, and body are the three satellites needed to triangulate your position.
You don’t have to experience loss of consciousness to have a concussion. A concussion can arise from any blow or jolt to the head or from whiplash. It can damage any part of your brain, including the inner ear.
The damage from a concussion isn’t structural and therefore won’t show up on a regular MRI. Think of concussion brain damage like a struggling business. If you look into the window, you see lights on during the workday and employees at their computers. But just because the physical components needed for the business are present doesn’t mean the business is doing well. Maybe the employees keep miscommunicating, or the computer software keeps glitching and slowing down operations. Similarly, just because all of the parts of your brain are present doesn’t mean they are working well together.
A concussion disrupts the delicate but important communication patterns between neurons and the blood vessels that supply them (called neurovascular coupling, or NVC). Sometimes, this inefficient communication is only temporary as you recover from the immediate bruising and inflammation following brain trauma. But for up to 30% of concussion patients, NVC dysfunction continues, causing symptoms for months or even years after the injury.
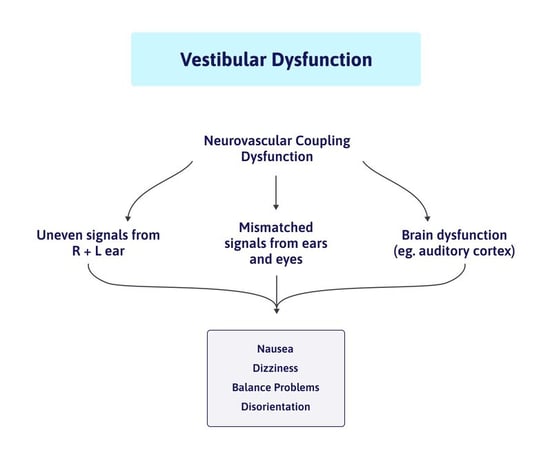 This dysfunction makes it so that some brain regions are hyperactive (either doing more than they should or using up too much of the brain’s resources) or hypoactive (not doing their fair share of the brain’s work). It can occur anywhere in the head, including the vestibular system. Dysfunctional neurovascular coupling exhausts the brain and results in any number of common concussion symptoms such as headaches, neck pain, brain fog, sleep issues, and more.
This dysfunction makes it so that some brain regions are hyperactive (either doing more than they should or using up too much of the brain’s resources) or hypoactive (not doing their fair share of the brain’s work). It can occur anywhere in the head, including the vestibular system. Dysfunctional neurovascular coupling exhausts the brain and results in any number of common concussion symptoms such as headaches, neck pain, brain fog, sleep issues, and more.
If you have vestibular problems after a head injury, it’s often because one side is sending a stronger signal than the other. When one ear is telling your brain one thing and the other ear isn’t quite corroborating the story, common symptoms like dizziness arise.
But your symptoms could also stem from how your vestibular system interacts with the rest of your body. Remember, the brain relies on data from your vestibular system, your vision, and your proprioceptive system to determine where you are and how fast you’re moving relative to the objects around you. When any one of those systems is injured, it will affect the others.
Often, patients with vestibular disorders have functional vision issues or dysfunction in the brain regions that interpret signals from the eyes and ears. Even if only the vestibular system is affected, the mixed signals (your eyes seeing one thing, but your vestibular system sensing another) is enough to cause some post-concussion symptoms as well.
Most concussion patients never have to worry about their inner ear crystals (canaliths). But a small percentage may have symptoms from ear crystals that move into the wrong location.
Inner ear crystals help us with linear movement. If we’re in a car or riding the elevator, they help our brain understand acceleration and deceleration. Normally, they rest in a large chamber called the utricle. It’s like a bowl of gelatin with rocks (the crystals) on top. When you start to move forward, the crystals stay behind for a moment and then catch up, giving you the sensation of movement.
During a concussion, some of those calcium crystals may be jostled loose and travel to the semicircular canals. Here, they interfere and cause your brain to receive incorrect positional information. The result is near-constant vertigo.
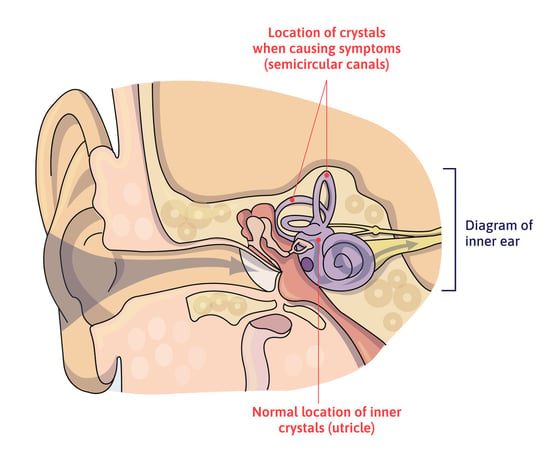
Fortunately, there’s a simple fix for this problem: the Epley maneuver. The Epley maneuver is a series of movements designed to get the crystals out of your canals and back into the utricle where they belong. It’s best to have a health care professional perform this maneuver on you for the first time, but you may be given instructions on how to do it at home as well.
Physical therapists Bob Schrupp and Brad Heineck demonstrate the Epley Maneuver in real time with a patient. The epley maneuver is a go-to method to help patients with benign paroxysmal positional vertigo (bppv).
After a concussion, you might experience any number of these symptoms related to the vestibular system:
Many people have a slight imbalance in their vestibular system (signals favoring either the right or left ear) before sustaining a head injury. It’s something our brain gets used to compensating for. But a brain injury makes it a lot harder for the brain to compensate because it has so many more problems to handle. It gets overwhelmed! So an issue that wasn’t a big deal before a TBI could become noticeable afterward.
If you have a preexisting vestibular imbalance, it might take you longer to recover from your injury. All patients can benefit from vestibular rehabilitation, but your specific situation will determine how long it takes for you to see improvement.
Many people have symptoms unrelated to the vestibular system after a concussion, too. Read our post on the symptoms of a concussion to learn more about what they are and how they’re treated.

Vestibular therapy has two parts: diagnosis and treatment. Many people slip under the radar in doctors’ offices because their deficits aren’t bad enough for a neurologist or other medical doctor to notice, so they don’t get diagnosed. But just because you don’t have a clinical deficit doesn’t mean you don’t have real, functional deficits that can be identified and treated.
At the most basic level, vestibular therapy retrains your brain to orient itself properly to your actual position in space, which requires more than just standing on a balance board. You need to do balance exercises, but you also have to engage your visual system and move your head around for therapy to be effective.
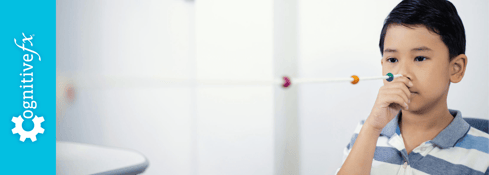
Every evaluation for vestibular dysfunction at Cognitive FX starts the same way. We’ll ask you to focus your vision on a single point while moving your head side to side, then up and down. We also ask you to move your head diagonally while we observe you for tell-tale eye movements and symptom triggers. This process allows us to diagnose each inner ear individually and tailor therapy accordingly. Many patients have one ear with a stronger signal going to the brain than the other, which will keep causing symptoms if it’s not corrected.
Testing for blurry vision and other functional vision changes is also important because vestibular dysfunction and ocular problems often go hand in hand. You might find that your vision is clear when you’re still, but blurs during movement, for example.
Many patients have no idea that their vision is affected after a concussion. Vision is more than checking to see if your eyesight is 20/20. Eye tracking, peripheral vision, ease of focusing, and how you respond to screens are a few examples of functional vision that could change after a concussion. Even if you don’t notice these vision changes, they could be behind symptoms such as headaches, eye strain, fatigue, and more.
The first goal of vestibular rehabilitation is simple: to get you to have vision that is clear and stable during head movement! To accomplish that, we use a process called gaze stabilization. Many patients experience a near-instant improvement in their balance once they’ve gone through gaze stabilization exercises. After that, we’ll move on to exercises that involve more movement and balance.
For example, after activating the individual sides or canals that need work with gaze stabilization exercises, patients then perform full body exercises like catching a ball while standing on a wobbly surface or walking in a Figure 8 pattern around obstacles all while keeping your eyes focused on a point (called the Infinity Walk). We also teach patients good breathing techniques. Proper breathing keeps your body well oxygenated and facilitates recovery.
Some people have vision problems but no vestibular issues; others have vestibular issues without vision problems. Many have both. The exact struggles you have determine what kind of therapy you get and how many sessions you’ll need. For stubborn vision problems, you may need to see a vision therapist separately.
After working with a therapist, you’ll be given exercises to do at home as well. These will continue to reinforce the improvements you make at each appointment.

Whether you get vestibular therapy at Cognitive FX, or try a different clinic, pay close attention to how your therapist handles intake. The best therapists:
One of the most important practices is to determine if there’s an imbalance between the left and right inner ear. When therapists work both sides indiscriminately, it can sometimes worsen the difference between the two ears. But if they balance the two sides first, then move to full body exercises, patients progress more quickly.
At Cognitive FX, vestibular therapy is just one part of a comprehensive treatment program for people suffering from lingering symptoms after a concussion or other head injury. If you’re only experiencing symptoms related to vestibular function, then finding a vestibular or vision therapist is likely sufficient. But many patients struggle with symptoms such as headaches, sleep problems, difficulty exercising, brain fog, light sensitivity, emotional changes, and more.
Vestibular therapy can’t fix all of those issues, and treating each symptom separately may not help if they all stem from the concussion. And knowing exactly which brain regions are affected in which way determines which therapies will help. The best treatment plan takes into account those differences.
At Cognitive FX, we use a unique imaging protocol (functional neurocognitive imaging, or fNCI) to identify which specific regions of the brain were affected by the concussion and how. We then use a host of therapy techniques — such as physical therapy, cognitive therapy, sensorimotor therapy, occupational therapy, and more — to treat the specific brain injury you’ve sustained. At the end of treatment, patients get another brain scan to see the improvement they’ve made.
You can learn more about our program here.
Vestibular therapy helps with vestibular symptoms. If you find a good therapist who treats each side of your system individually, you should make rapid progress. But vestibular therapy alone — even if it’s alongside vision therapy — isn’t enough to make all post-concussion symptoms go away.
If you’re having persistent symptoms after a concussion or other head trauma, it’s best to get treated for all of those symptoms at once. At Cognitive FX, we can evaluate your brain, vision, and vestibular system to determine what therapy you need. 95% of our patients experience statistically verified restoration of brain function!
Schedule a consultation with our team to learn if you’re eligible for our program.

Andy is a Certified Athletic Trainer (ATC) and Z-Health Performance Master Trainer. He began his career in Orthopedics, then worked as Head Athletic Trainer and Director of Human Performance at a specialty physical therapy clinic. Here, his passion for innovative human body approaches ignited. In 2010, he founded Fitness Evolved in Berkeley, CA, focusing on a neurologically informed health and exercise paradigm. Andy mastered the Z-Health Performance Solutions system, creating brain-centric training and rehab at Fitness Evolved, serving diverse clients, including pro athletes and brain injury survivors. He's an accomplished Z-Health instructor, having trained professionals worldwide. Andy is thrilled to join Cognitive FX, contributing to our revolutionary concussion and TBI recovery techniques.

Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect...

If you’ve had a severe or mild traumatic brain injury (severe TBI or mild TBI) that’s left you with post-concussion syndrome (PCS), just thinking can be taxing. Cognitive health is “the ability to...
As you read this text, your brain is processing the incoming visual information and sending directions to your eyes so they maintain focus on what you want to read. But if you have post-traumatic...

Post-concussion syndrome (PCS) is a complex condition in which concussion symptoms persist for weeks, months, or even years after the initial head injury. While most people recover from a concussion...

Balance is a complex physiological process involving multiple systems in the body, which can be easily disrupted following a concussion. Between 40 and 60% of patients experience balance and...
Living with the lingering symptoms of a concussion for months or even years is life-changing. Patients with post-concussion syndrome (PCS) can feel worthless, misunderstood, lonely, and frustrated....
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY