Balance is a complex physiological process involving multiple systems in the body, which can be easily disrupted following a concussion. Between 40 and 60% of patients experience balance and dizziness issues after a mild traumatic brain injury (mTBI). While most recover within days, some endure symptoms for months or even years, often alongside other symptoms such as headaches, brain fog, and low mood.
Vestibular rehabilitation therapy, commonly recommended to patients with balance problems and post-concussion dizziness, helps retrain the brain to manage balance and reduce dizziness. While this approach is highly effective for treating balance issues, it addresses only a part of the broader challenges faced by post-concussion patients.
In this article, we cover the symptoms, causes, and diagnosis of balance issues in post-concussion patients, along with an overview of what to expect from vestibular therapy. We also explain why a comprehensive treatment plan that addresses balance, physical, cognitive, and emotional symptoms can be more effective for patients with lingering concussion symptoms.
Below, we cover:
If you've experienced one or more head injuries and have symptoms such as balance problems, headaches, brain fog, and more, you're not alone and you're not imagining it. Help is available. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-head injury symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. Schedule a consultation to see if you’re eligible for treatment.
Balance Problems Are Common After a Concussion
Balance problems are common after a concussion, with around half of patients reporting unsteadiness and loss of balance at some point. Describing these symptoms can be difficult, with some patients feeling like their surroundings are spinning, while others describe the sensation as walking on a mattress or stepping off a merry-go-round.
Patients may experience:
- A feeling that their surroundings are moving (vertigo)
- Lightheadedness
- Feeling faint
- A sensation of floating or swimming
- Disorientation
- A sense that the room is moving or spinning
- Unsteadiness
- Staggering when walking
- A feeling of floating, wooziness, or heaviness
- A feeling of floating in the air
- Difficulty walking in a straight line
- A sense of being disconnected from their body
- A feeling of being on a boat
- A sensation of swaying
- A feeling that they’re going to fall
Some patients experience these symptoms immediately after a concussion, while others notice them a few days later. When a head injury affects multiple areas of the brain, the most severe symptoms often appear first. Vestibular or visual system issues may be present from the start but remain unnoticed initially as the brain prioritizes more serious symptoms first.
This explains why some patients notice balance problems only after other severe symptoms, like headaches, improve. For instance, a patient might make significant progress in therapy, only to start noticing dizziness as their intense headaches subside.
For some, dizziness is constant, occurring when moving, standing still, or lying down. For others, it’s triggered by specific activities, such as exercising or riding in a car.
Understanding these patterns can help patients and providers navigate the recovery process and tailor treatment to individual needs.
What Causes Balance Issues After a Concussion?
For most patients, it’s difficult to determine exactly what causes symptoms of dizziness and imbalance. Often. It’s a combination of several factors, including:
Direct Damage to the Vestibular System
Balance problems after a head injury may be caused by damage to the vestibular system. This system helps us maintain balance and understand where we are in space. It includes the inner ear, parts of the brain (like the brainstem and cerebellum) that process signals from the ear, and the vestibular nerve, which connects them.
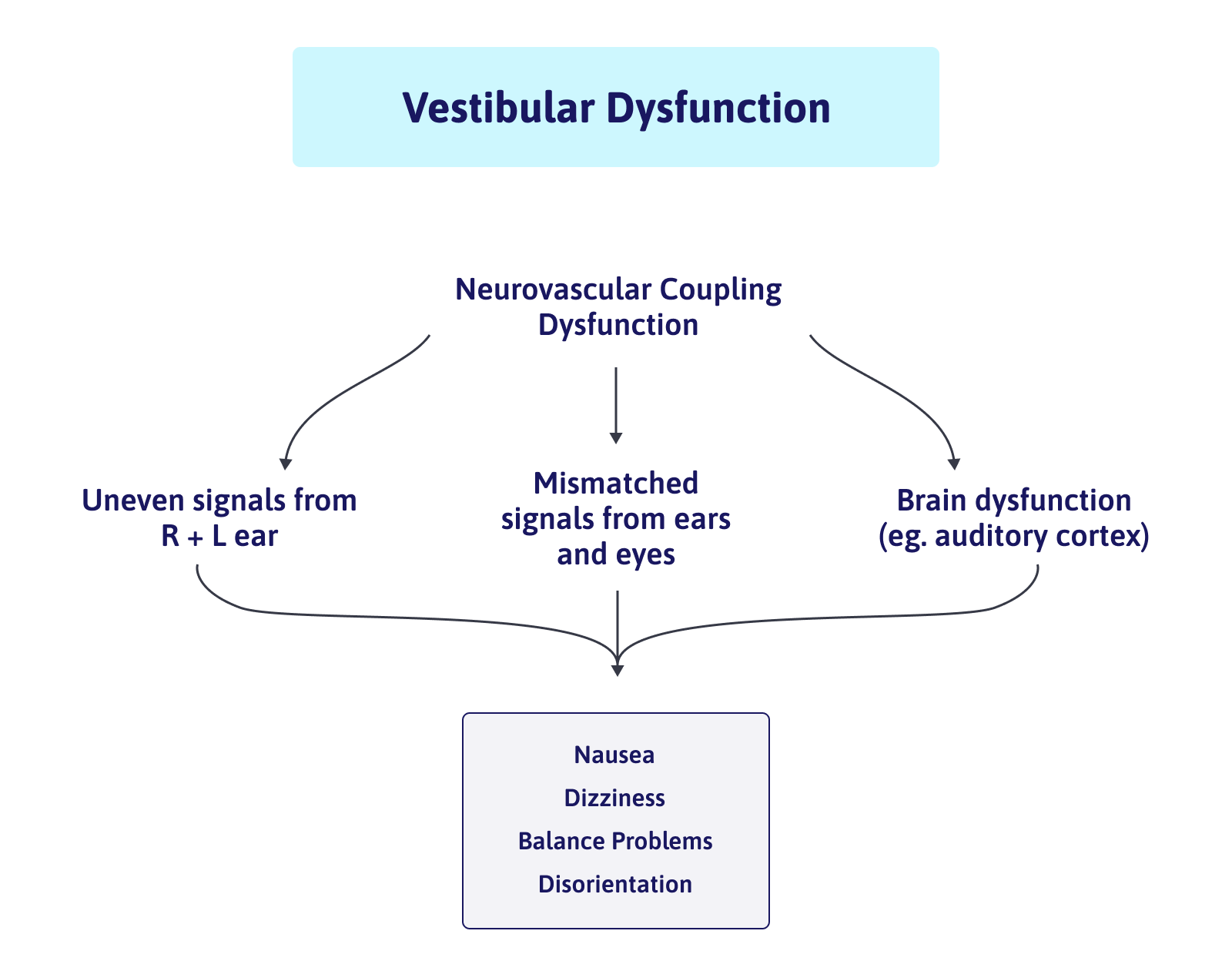
When any part of this system is disrupted by a concussion, it can lead to symptoms such as dizziness, unsteadiness, or a spinning sensation. For example, if the vestibular nerve is damaged, the brain might not receive crucial signals from the inner ear. This mismatch can confuse the brain and result in dizziness or lightheadedness. Similarly, if one ear sends stronger signals to the brain than the other, it can also cause these symptoms.
Interestingly, the areas of the brain involved in balance processing are connected to regions that regulate nausea and heart rate. This explains why balance problems often come with symptoms like nausea or digestive discomfort.
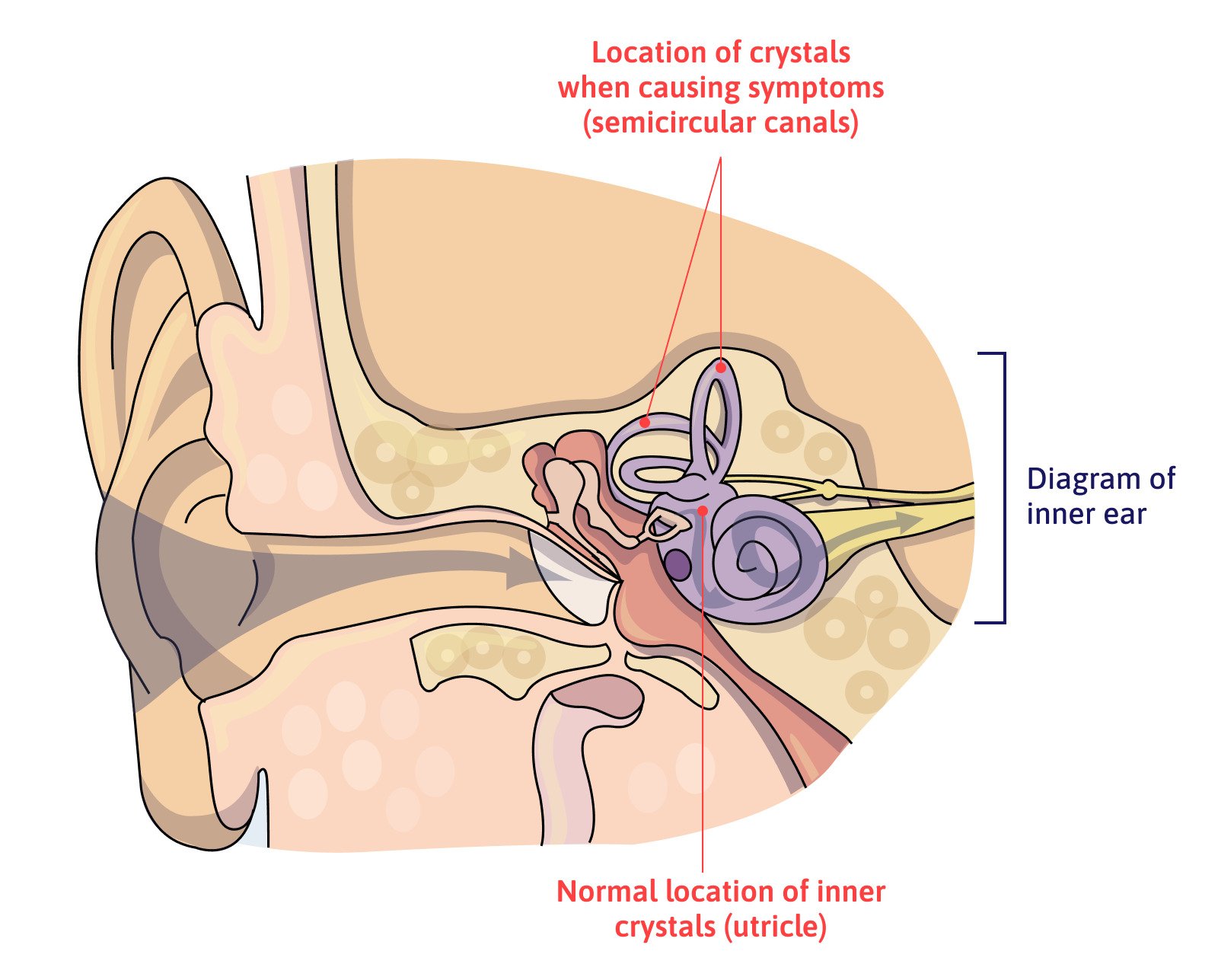
Benign Paroxysmal Positional Vertigo (BPPV)
Affecting more than half of post-concussion patients with dizziness, the most common vestibular disorder after a concussion is called benign paroxysmal positional vertigo (BPPV).
BPPV occurs when tiny calcium crystals called otoconia are dislodged from their normal location on the utricle, a sensory organ located inside the inner ear. When these crystals become free, they can flow inside the inner ear in spaces filled with fluid called semicircular canals. As these areas are important to sense rotation movements of the head, patients can experience vertigo when they change their head position, such as when looking up or down, going from lying to sitting, or rolling over in bed.
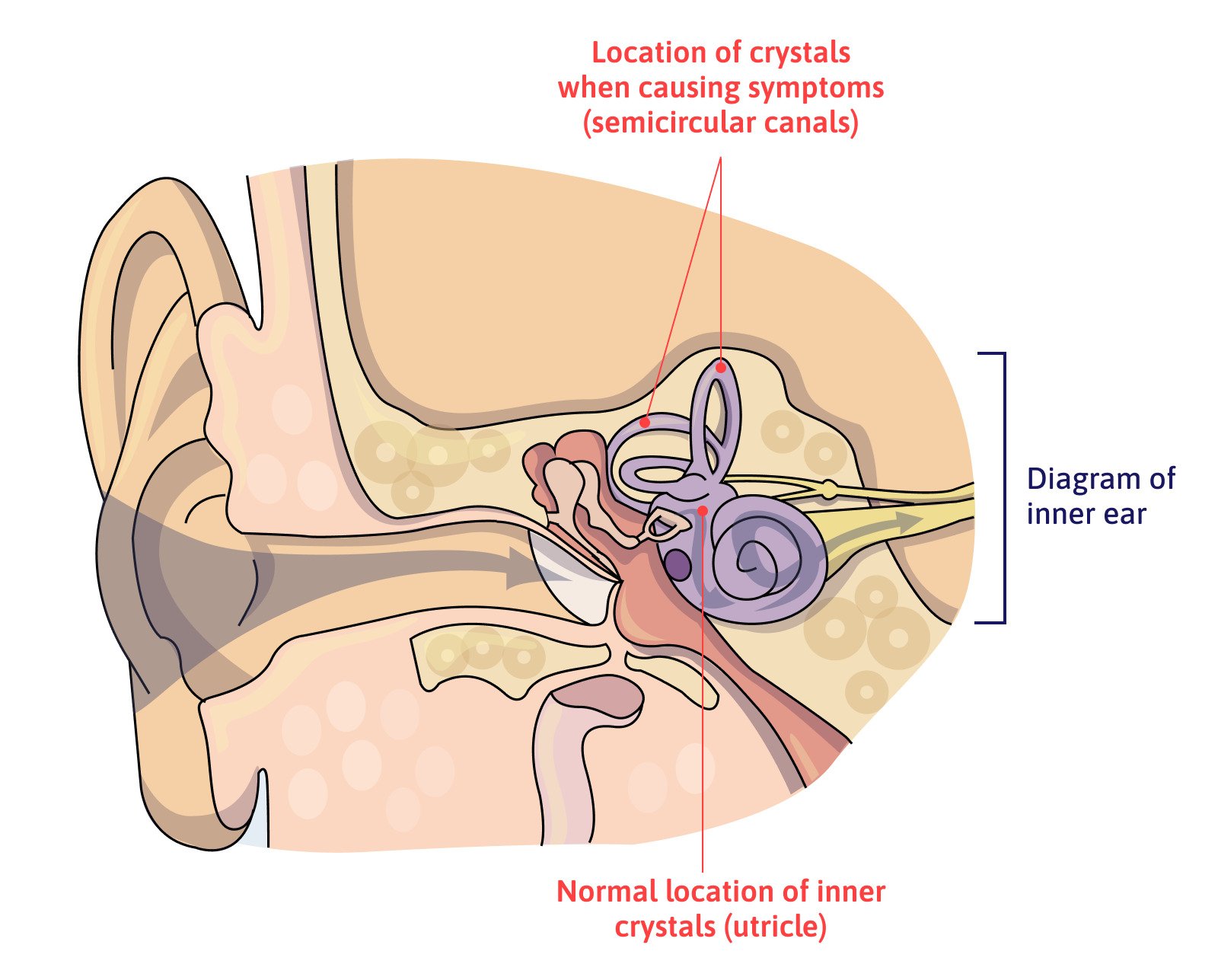
Many cases resolve without treatment, but patients with persistent symptoms may need a technique called the Epley maneuver (or another canalith repositioning maneuver) to dislodge the crystals from the canals and return them to the vestibule.
Neurovascular Coupling (NVC) Disruption
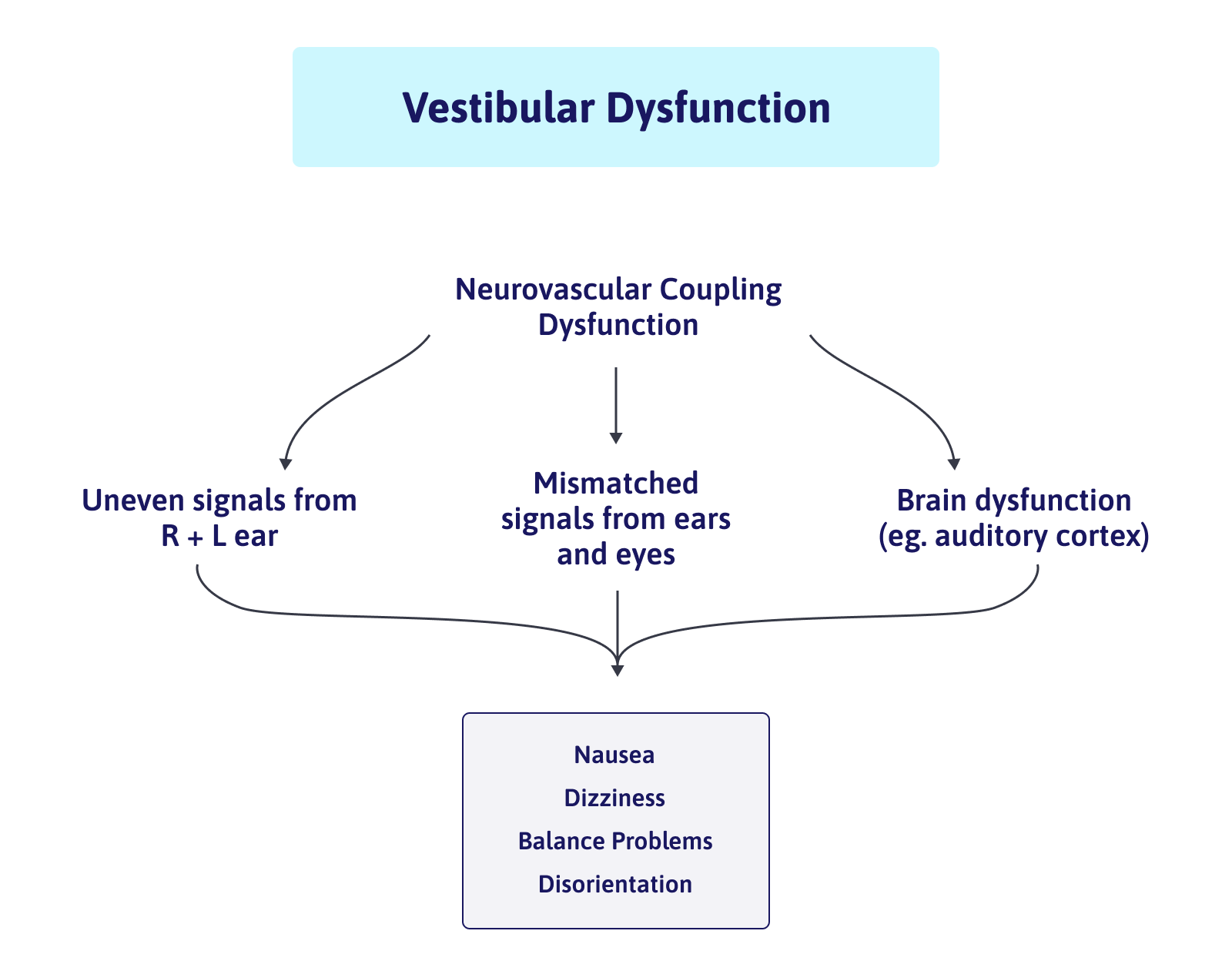
In a healthy brain, brain cells receive the resources they need to perform a particular task from a network of blood vessels. This dynamic relationship is called neurovascular coupling (NVC).
Concussions, however, can disrupt this mechanism. As a result, some areas of the brain can no longer function normally. If this occurs in the areas involved in processing information related to balance, including the brainstem, the cerebellum, and the cranial nerves that connect the vestibular and visual systems to these areas, patients may experience dizziness, vertigo, or lightheadedness.
Neurovascular coupling disruption is one of the root causes of concussion symptoms and is a key area of focus at our clinic.
Further reading: What is neurovascular coupling?
Dysfunction of the Autonomic Nervous System (ANS)
Dizziness and other balance deficits can also be caused by dysfunction of the autonomic nervous system (ANS).
The ANS includes the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which regulate vital body functions such as blood pressure, heart rate, sweating, and breathing rate. Faulty regulation of the ANS, known as dysautonomia, can lead to symptoms like dizziness, vertigo, and imbalance.
For example, ANS dysfunction can disrupt breathing and blood pressure regulation. In practical terms, this means the body cannot make the small adjustments needed to maintain blood pressure (BP) when moving from sitting to standing, causing BP to either rise or fall too much, leading to dizziness and lightheadedness.
Further reading: The patient’s guide to post-concussion autonomic dysfunction (dysautonomia)
Mismatch Between Vision and Vestibular Systems
Your dizziness may also be caused by a mismatch of information coming from the visual and vestibular systems, which is not interpreted correctly by the brain. This is called a visual-vestibular mismatch.
In simple terms, it means the information your brain receives from your eyes does not match that from your vestibular system. Without reliable information, the brain cannot correctly interpret what’s moving: you, or the things around you.
This mismatch can be triggered by anything that overwhelms your vision. Common situations may include:
-
Large shopping areas, which are often busy and noisy
-
Places with kids and pets (Fast movement in your peripheral vision can play tricks on your brain.)
-
Busy or large patterns on the floors and walls
-
Ceiling fans
-
Windshield wipers
-
Sunlight flickering
-
Driving or being a passenger in a car
Problems with Proprioception
Proprioception refers to the body’s ability to sense its position and head movements. It’s an automatic or subconscious process. Proprioception allows the brain to know the body’s position without relying on visual input alone.
This system is formed by sensors located in the skin, bones, and muscles, especially the joints, where most of the receptors — called mechanoreceptors — are found. These receptors send information to the brain about movement and positioning, helping the body understand which parts are in contact with the ground and which are in motion. This allows for a stable, upright position and balanced movement.
If head trauma disrupts the communication between these sensors and the brain, the brain doesn’t get the messages it needs leading to balance problems. If patients experience dizziness when their eyes are closed, it’s a good indication that the problem lies with the proprioception or the vestibular system. Without visual input, the brain has to rely solely on these systems to maintain posture.
Medication
Some medications can make you feel dizzy, lightheaded, and off-balance. Examples include antibiotics, tranquilizers, blood pressure, heart, and seizure medication. Not surprisingly, the more medication you take, the higher the chances of triggering dizziness.
If you’re worried, ask your doctor if any medicines you take may be causing dizziness or balance problems. A change in medication or dosage may fix the problem.
Further reading: Medication for post-concussion syndrome
Hormonal Disorders
Some cases of imbalance and lightheadedness can be triggered by hormonal disorders. For example, about 10% of patients experience post-concussion pituitary dysfunction, which can cause dizziness. If your symptoms persist for a long time despite treatment, our advice is to seek medical help from an endocrinologist for a full hormone analysis.
Further reading: Post-concussion hormone dysfunction
Psychological Problems
Some people with head injuries develop fear and anxiety if they’re constantly worried that they’re going to trip and fall. In turn, these emotional symptoms can cause or aggravate dizziness and vertigo episodes and are often accompanied by headaches, breathlessness, nausea, panic, and heart palpitations.
Practitioners call this psychogenic dizziness. These psychological problems can reduce the normal amount of carbon dioxide in the body, causing dizziness and lightheadedness and potentially aggravating other mental health issues.
How Post-Concussion Balance Problems are Diagnosed

Vestibular impairments caused by a concussion can be diagnosed by a primary care doctor, but more often are diagnosed by a specialist such as an otolaryngologist, otologist, neurologist, or neuro-otologist. Depending on the severity of the injury, evaluation by an audiologist or other healthcare professional may be helpful to assess any damage to the inner ear.
Typically, your healthcare provider will ask about your symptoms, your medical history, and any medications you are currently taking. Depending on your symptoms, you may have some of the following tests:
-
Hearing and vestibular function tests
-
Eye movement tests
-
Balance tests that measure to assess what happens when you remove input from the visual or proprioceptive systems by standing on a soft surface with your eyes closed
-
Blood tests
-
Imaging (CT or MRI scans) can be used to rule out serious injuries
The aim is to determine which aspect of the balance system is affected, which in turn will decide what kind of treatment options are available for the patient. Assessment tests the vestibular and visual system, proprioceptive receptors, and the integration between all three systems.
Vestibular Rehabilitation Therapy Is the Most Effective Way to Treat Balance Problems
The most common way to treat symptoms of dizziness and imbalance after a concussion is with vestibular rehabilitation therapy (sometimes referred to as VRT).
This therapy helps strengthen the communication between the body (proprioception), eyes (visual system), inner ear (vestibular system), and brain. During therapy sessions, symptoms are intentionally triggered in a safe and controlled environment to work towards getting the brain used to situations that cause dizziness. The overall goal is to increase the patient’s quality of life, decrease symptoms, and improve overall function.
Studies show that rehabilitation programs are more effective when they’re customized to each patient. The type, frequency, and intensity of effective exercises vary from person to person.
As such, a rehabilitation program may include:
-
Adaptation exercises: These exercises are useful if patients struggle to maintain focus. The aim is to keep visual targets in focus even when the head is moving.
-
Gaze stabilization exercises: During these exercises, patients move their heads while keeping their eyes focused on a target. Patients start slowly and gradually increase speed and move their heads as quickly as they can while keeping the target in focus (not blurry). Often patients get a little dizzy or miss the target every now and then.
-
Habituation exercises: These exercises are designed to reset nervous system sensitivity. They help the brain get used to movements or situations that make the patient feel dizzy. Patients repeat exercises with controlled exposure to signals such as certain body movements, visually complex patterns, and busy environments.
-
Balance retraining exercises: These exercises involve standing on different surfaces with increasingly narrow bases of support. They are used to improve steadiness to carry out daily activities and lower the risk of falling.
-
Balance exercises with eyes closed: These exercises help reduce the reliance on the visual system and encourage the use of the vestibular system.
-
Gait training: These exercises involve relearning how to walk over unstable surfaces.
-
Breathing and relaxation exercises: These exercises help regulate the autonomic nervous system, whose malfunction can trigger dizziness (see above).
Other Treatments for Vestibular Problems
Some patients may need specific treatment for their conditions, such as the Epley maneuver to address BBPV or medications to help patients cope with their symptoms.
Treatment for BBPV
In most cases, BPPV can be treated successfully without any surgery or medication by using the Epley maneuver.
This is a simple and effective method to treat BPPV and involves sequentially turning the patient’s head in a way that helps move the crystals and help them float back to their correct position. Patients often need several repositioning maneuvers to get the best results.
After this treatment, patients should be more careful and avoid putting their head back or bending far forward for the remainder of the day. Sleeping on the side of the affected ear should be avoided for several days.
For patients with extreme nausea, the doctor may prescribe anti-nausea medications, especially if it helps the patient tolerate the repositioning maneuvers.
Medication
Patients with severe balance issues that last hours or days can be prescribed medications for motion sickness to control dizziness and vomiting.
Some doctors may prefer to use sedatives to address dizziness. These prescription drugs don’t stop the symptoms but help patients cope with the sensation. In extreme cases, antidepressants may be useful in some patients.
Concussions Cause More Than Just Balance Problems
Balance problems are rarely the only symptom a patient experiences after a concussion. It’s not uncommon for patients to experience a variety of physical, cognitive, and psychological symptoms, including headaches, brain fog, anxiety, low mood, nausea, difficulty concentrating, and sleep disturbances.
Patients may try to address their issues by going to different specialists — which may include a physical therapist for vestibular therapy — but this approach only addresses symptoms in isolation and often without knowing the root problem behind these symptoms.
At Cognitive FX, we believe these symptoms are best treated in combination instead of one by one. Our multidisciplinary team uses different therapies tailored to each patient’s unique injury and needs to maximize our patients’ chances of recovery.
Treating Post-Concussion Symptoms (Including Balance Problems) at Cognitive FX

Since every patient is different, our treatment process starts with a detailed and in-depth evaluation with our team. This includes a review of your medical history, an assessment of your symptoms, and a series of physical exams, including a close examination of your balance and posture.
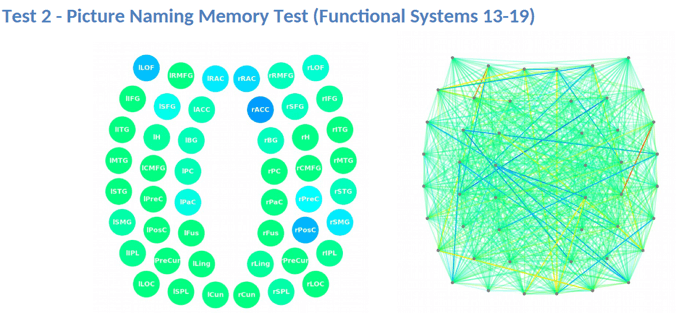
Patients undergo a state-of-the-art brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine exactly how the concussion affected their brain.
The fNCI scan measures blood flow in 100 different regions of the brain while patients carry out a set of standardized cognitive tasks. It produces a series of real-time images that are combined and compared with scans from healthy people to identify the areas where NVC dysfunction is affecting normal brain function.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with neurovascular coupling dysfunction.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
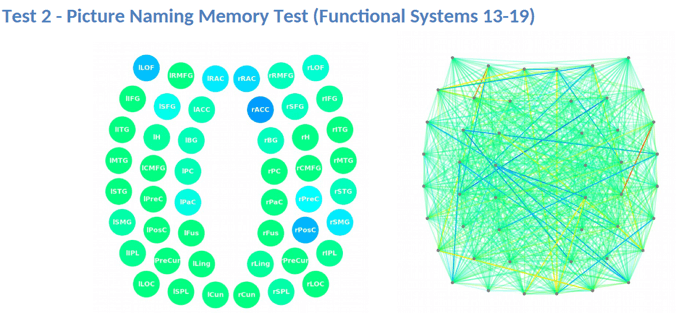
This information provides our staff with huge advantages when it comes to treating patients. For example, if we see visual systems such as target search, visual feature detection, or visual-spatial mapping aren’t working as they should, we can tailor exercises to work on those specific areas of the brain during therapy.
We also carry out structural MRI to check for brain and neck injuries that may explain dizziness and other balance problems.
After this initial evaluation, our therapists combine all the results to design a custom-made treatment plan for each patient. We call our individualized treatment program Enhanced Performance in Cognition, or EPIC for short.
What EPIC Treatment Is Like
Each day of therapy during EPIC treatment, you’ll cycle through a three-step process:
Prepare

Therapy starts with short bursts of aerobic exercise on the treadmill or stationary bike. Exercise triggers the release of important chemicals in the brain, including a compound called brain-derived neurotrophic factor (BDNF). BDNF promotes the growth of brain cells and improves communication between different areas of the brain. In turn, this helps the patient's brain become more flexible and boosts the effect of subsequent therapy.
Even patients who struggle with physical activity due to their balance problems can make remarkable progress in these sessions. Our therapists are trained to help patients exercise according to their needs and without triggering severe symptoms.
Activate

After exercise, patients attend a variety of therapies, including cognitive therapy, sensorimotor therapy, neuromuscular therapy, Dynavision therapy, occupational therapy, neurointegration therapy, vision and vestibular therapy, and psychotherapy, to name just a few. Patients receive all or most of these therapies during their visit, but the exact regimen for each one is unique to them.
For patients with balance problems, neurointegration therapy is one of the most important. During these sessions, therapists will guide patients through a series of exercises to help vision, vestibular, and proprioceptive systems. The aim is to recover individual functions for each system and then bring them together. This neurological integration is key to fully rehabilitating balance issues. This type of therapy we offer is unique and comes from years of experience from our team.
To improve vision, patients might do eye tracking, gaze fixation, eye saccades, eye movement exercises, and the Brock string (which helps your eyes to work together and focus on objects at different distances).
To improve vestibular function, patients may engage in different types of exercises to help with balance. One example is gaze stabilization exercises, which involve nodding “yes” or shaking your head “no” while focusing on a letter on the wall. While many clinics treat the left and right ear equally, we go beyond this simple approach and differentiate between the levels of dysfunction in each ear. Often, patients have one side more affected than the other, and treating both sides equally can allow the imbalance to persist, often leading to an increase in symptoms rather than full resolution.
At Cognitive FX, our therapists assess each part of the vestibular system and each side separately. If they find a specific problem with a particular area on just one side, patients may need to do “half no” or “half yes” exercises: not a full nod or shake with the head (which would affect both sides), but short movements to the left/right, up/down, or diagonal with just one side of the head.
Finally, we integrate the vision, vestibular, and proprioceptive systems. At this stage, patients go inside a device called the Maverick, which is shaped like a giant diamond. In each vertice, there’s a light and a letter or a number. Patients need to follow a particular sequence by touching each light; the aim is to integrate head and body movement to get all the systems “talking” to each other in a healthy way.
We have many patients who have tried both vision therapy and vestibular therapy separately with limited success but make significant improvements during their neurointegration sessions when their vision and vestibular systems start to work together again.
Recover
The third step involves periods of rest, which allows the brain to recover before repeating the process. These may include:
-
Neuromuscular massage for the neck and shoulders
-
Breathing and mindfulness exercises
-
Listening to Brainwaves, which work similarly to meditation.
At the end of treatment, patients undergo a second brain imaging scan to check on their progress. They then meet with one of our therapists to review the results and receive a series of at-home exercises. These typically include physical activities, cognitive tasks, visual and vestibular exercises, and relaxation techniques. We recommend patients perform these exercises for about an hour five times a week initially, with the frequency decreasing as symptoms improve. For patients needing further therapy, we provide referrals to appropriate specialists.
On average, our patients’ symptoms improve by 60% after just one week of treatment. To see if you are eligible for treatment, sign up for a consultation.
Tips to Cope with Balance Problems
Dealing with symptoms of dizziness and imbalance at home or work is not always easy. Some patients feel motion sickness or nausea in busy places with bright lights, noise, or movement like a shopping mall or movie theatre.
Here are some tips to cope with these symptoms:
-
Slow down: Take your time when you have to move, such as getting out of bed or bending down to pick up something from the floor. If you start to feel dizzy, try to sit down and move your legs up and down for a few minutes before getting up.
-
Stay active: You may want to avoid exercise as it may trigger symptoms, but it’s important to keep moving. Avoiding physical activity because you’re afraid you may fall increases your chances of actually falling. Inactivity may also lead to anxiety and social isolation, which can lower your quality of life.
-
Prevent falls: Ideally, patients experiencing balance problems should make some changes at home to avoid falls. Tips include removing all clutter in the house, using non-slip mats in the shower, and using railings to go up or down the stairs, for example.
-
Rest frequently during the day: Feeling tired or lacking sleep can increase your risk of feeling dizzy. Make sure you take frequent breaks during the day. However, don’t take naps longer than 20-30 minutes; longer naps may negatively affect your sleep at night.
Further reading: Rest and concussions: Why taking brain breaks is good for you
-
Manage your medications: As we described earlier, some medications can cause dizziness. If this is happening to you, talk to your doctor; it may be possible to switch to a different medication or change dosing.