Vertigo is a common symptom after a mild traumatic brain injury (mTBI). Most patients describe it as feeling like either the room is spinning or they are. Almost half of those who sustain a concussion report vertigo in the first few days after their injury. For most patients, this feeling dissipates within a few days or weeks at most, but for some, post-concussion vertigo persists for years after the trauma.
For some patients, vertigo starts immediately after the head injury and persists throughout the years. However, this may not have been the case for you. It could be, for example:
- You experienced vertigo on and off over the years, sometimes accompanied by other symptoms, such as lightheadedness, dizziness, balance dysfunction, feeling faint, double vision, nausea, and vomiting.
- You didn’t develop vertigo immediately after the injury, but instead, it developed months or even years later.
- You experienced vertigo after the head injury, it was treated and resolved, and it’s now coming back a few years later.
- You’re currently experiencing medical issues (unrelated to the head injury) that are bringing back some of your concussion symptoms, including vertigo.
- You hardly noticed the dizziness at first and so learned to cope with it, but it’s gradually getting worse.
- You experienced visual problems after your head injury which were never properly resolved. These symptoms are getting worse, causing a mismatch between vision and vestibular systems and creating a vestibular problem that wasn’t there before.
As you can see, there are many different ways that your current vertigo could be a symptom of an old head injury, even after all these years! There are many possible causes of vertigo related to a head injury, and successful treatment depends on making an accurate assessment of the issue.
At Cognitive FX, we have a team of specialists who can investigate what’s causing your symptoms and treat you with a combination of exercise and multidisciplinary therapies. In this article, we’ll cover how head injuries cause vertigo years after the original incident and how we approach vertigo treatment at our clinic.
Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, schedule a consultation.
How Head Injuries Cause Vertigo Years Later
To maintain balance and help our body navigate around obstacles, our brain needs to process information coming from the eyes (visual system), ears (vestibular system), and body (proprioceptive system). We’ve explained this process in more detail in our article about post-concussion dizziness.
In very simple terms, anything that disrupts one or more of these systems or the way they communicate with each other can result in vertigo. This happens because the brain receives conflicting visual, proprioceptive, or vestibular information about your position in space.
Some of these causes include:
In this section, we’ll explain how a head injury can result in each condition. Oftentimes, a patient’s post-concussion symptoms stem from more than one, making an accurate diagnosis key to a good recovery plan.
Neurovascular Coupling (NVC) Disruption
In a healthy brain, nerve cells get the resources they need — nutrients and oxygen — from a network of surrounding blood vessels. This dynamic relationship is called neurovascular coupling (NVC).
However, concussions can disrupt this mechanism, resulting in areas of the brain that no longer receive what they need and, as a consequence, stop functioning normally. If this disruption affects areas of the brain involved in controlling coordination, balance, and equilibrium — especially the cerebellum — it can lead to vertigo, lightheadedness, and balance problems.
.png?width=1600&height=985&name=can%20a%20head%20injury%20cause%20vertigo%20years%20later%20(6).png)
Autonomic Nervous System (ANS) Dysfunction
The autonomic nervous system (ANS) is responsible for many different functions in the body, including blood pressure, heart rate, breathing rate, sweating, and others. Two subsections of the ANS are the sympathetic nervous system (SNS), which regulates the “fight-or-flight” response, and the parasympathetic nervous system (PNS), which regulates the “rest-and-digest” response.
If you feel vertigo when you stand up, it may be because your blood pressure drops too quickly. This could be due to a faulty regulation of the ANS caused by traumatic brain injury (TBI) — a condition called dysautonomia — which leads to autonomic symptoms such as dizziness, vertigo, and unsteadiness.
If your symptoms were originally mild and gradually got worse over time, they might stem from NVC disruption (see above) and/or ANS dysfunction. For some patients, vertigo only develops months or years after the head injury, when ANS dysfunction reaches a certain point and the brain is no longer able to compensate. The good news is that we treat this type of vertigo at Cognitive FX. (See more about treatment later in the article.)
Further reading: The Patient’s Guide to Post-Concussion Autonomic Dysfunction (Dysautonomia)
Whiplash
Another cause of prolonged symptoms after a head injury, including vertigo, is a neck injury due to whiplash. The first two vertebrae are particularly vulnerable to neck trauma. This neck region contains multiple nerves that are part of a complex proprioceptive system that relays information to the brain about the position of the head and body.
If whiplash damages these nerves, the brain receives inaccurate information, which in turn affects the vision and vestibular system. As a result, patients experience a variety of symptoms, such as dizziness, vertigo, lightheadedness, and spatial disorientation.
Further reading: The long-term effects of whiplash
Direct Damage to the Inner Ear (Vestibular System)
If the head injury damages the vestibular system (located in the inner ear), patients will experience balance problems, dizziness, and vertigo. This is sometimes called a labyrinthine concussion. It typically happens after a direct hit to the sides of the head, which in extreme cases can cause fracture of the temporal bone, the skull bone that protects the inner ear. In addition, vibration forces transmitted through the skull to the inner ear can produce a shock pulse that damages the inner ear.
Direct Damage to the Cerebellum in the Brain
Head injuries can also cause vertigo if two important areas in the brain called the brainstem and the cerebellum are directly damaged during the incident. If these areas are not functioning properly, they are easily overwhelmed by the information coming from the eyes and vestibular system, giving you symptoms of nausea and vertigo.
If your vertigo is caused by damage to the brainstem or the cerebellum, you may also experience:
- Poor balance
- Uncoordinated movements
- Episodes of dizziness
- Abnormal eye movements
- Nausea from busy visual environments
- Anxiety
- Digestive symptoms
- Tremors with movement
Damage to the 8th Cranial Nerve
We have a total of 12 cranial nerves in the head responsible for specific functions, such as helping you taste, smell, hear, and feel. Because they run through different parts of the face and head, they’re extremely vulnerable to damage during head trauma. Symptoms may appear immediately or can take days to develop.
The 8th cranial nerve — also called the vestibulocochlear nerve — connects the inner ear and the brain and is responsible for maintaining balance. Any injuries to this nerve can cause vertigo, nystagmus (involuntary movement of the eyes), tinnitus, and hearing loss.
Mismatch Between the Visual and Vestibular System
A mismatch between the visual and vestibular systems may also cause vertigo. This happens when your brain receives conflicting information coming from your eyes and your ears. As a consequence, the brain has a hard time figuring out which is moving: you or the things around you.
Anything that overwhelms your vision can trigger this mismatch, including:
- Noise and movement at busy shopping areas
- Quick movement of kids and pets
- Busy or large patterns on the floors and walls
- The motion of ceiling fans
- The back-and-forth movement of windshield wipers
- Flickering sunlight
- Car rides (whether passenger or driver)
Many of these triggers are because fast movement in your peripheral vision can play tricks on your brain.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in the long-term symptoms of head injury. To see if you are eligible for treatment, sign up for a consultation.
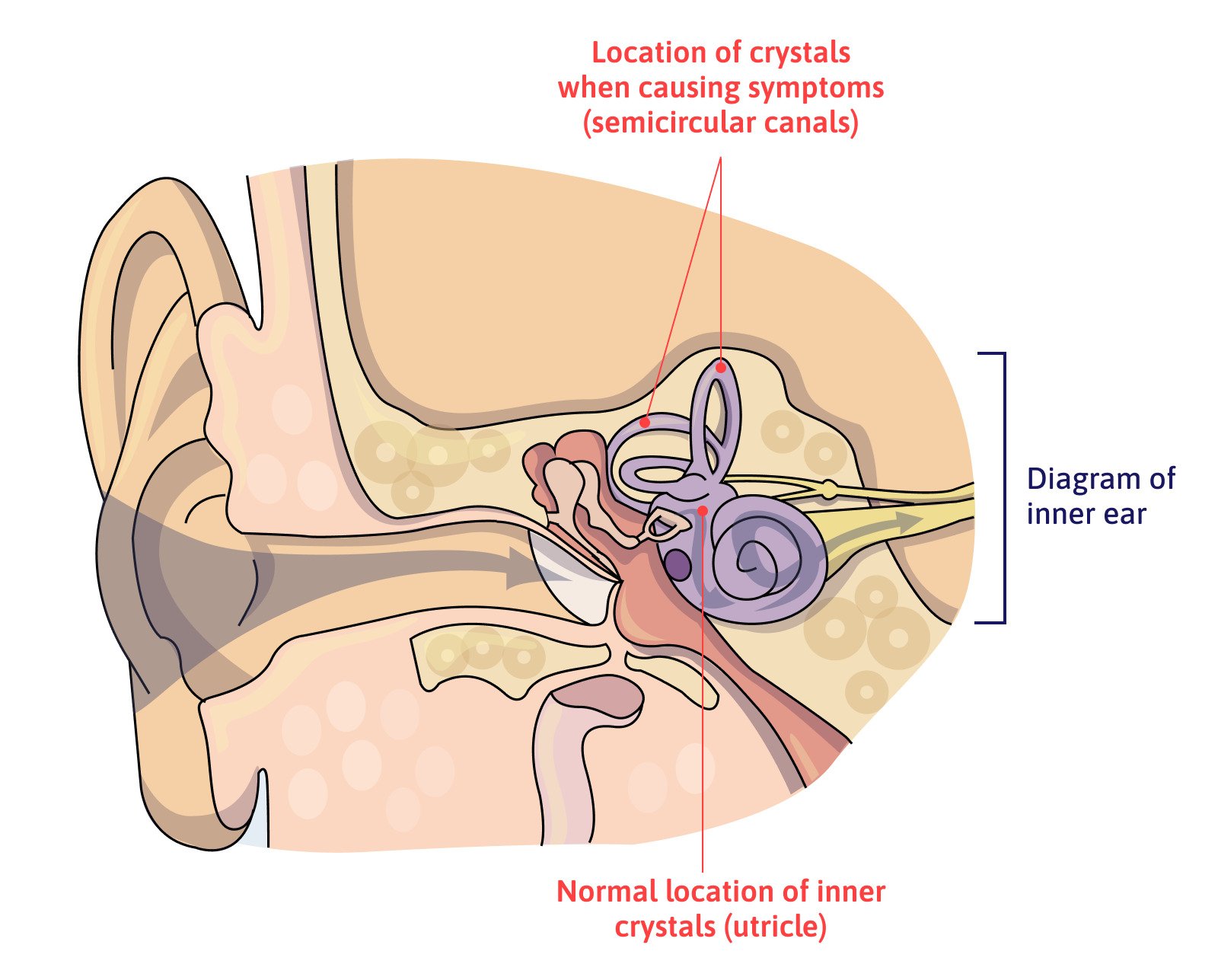
Benign Paroxysmal Positional Vertigo (BPPV)
The most common vestibular disorder after a concussion is called Benign Paroxysmal Positional Vertigo (BPPV). About one-third of patients with post-traumatic vertigo have this condition. It’s more common after a direct hit to the head, but even injuries that do not directly affect the head can cause BPPV.
Patients suffering with BPPV often describe their vertigo as if they’re on a merry-go-round. It typically happens with specific head positions and movements, such as sitting up in bed, bending down to pick something up, or a quick head movement.
BPPV occurs when the tiny crystals (called otoliths) which should be in the vestibule (including two sections called the saccule and utricle) move into one of the inner ear semicircular canals and get trapped inside. As your head moves, the canals send confusing information to the brain, causing vertigo.
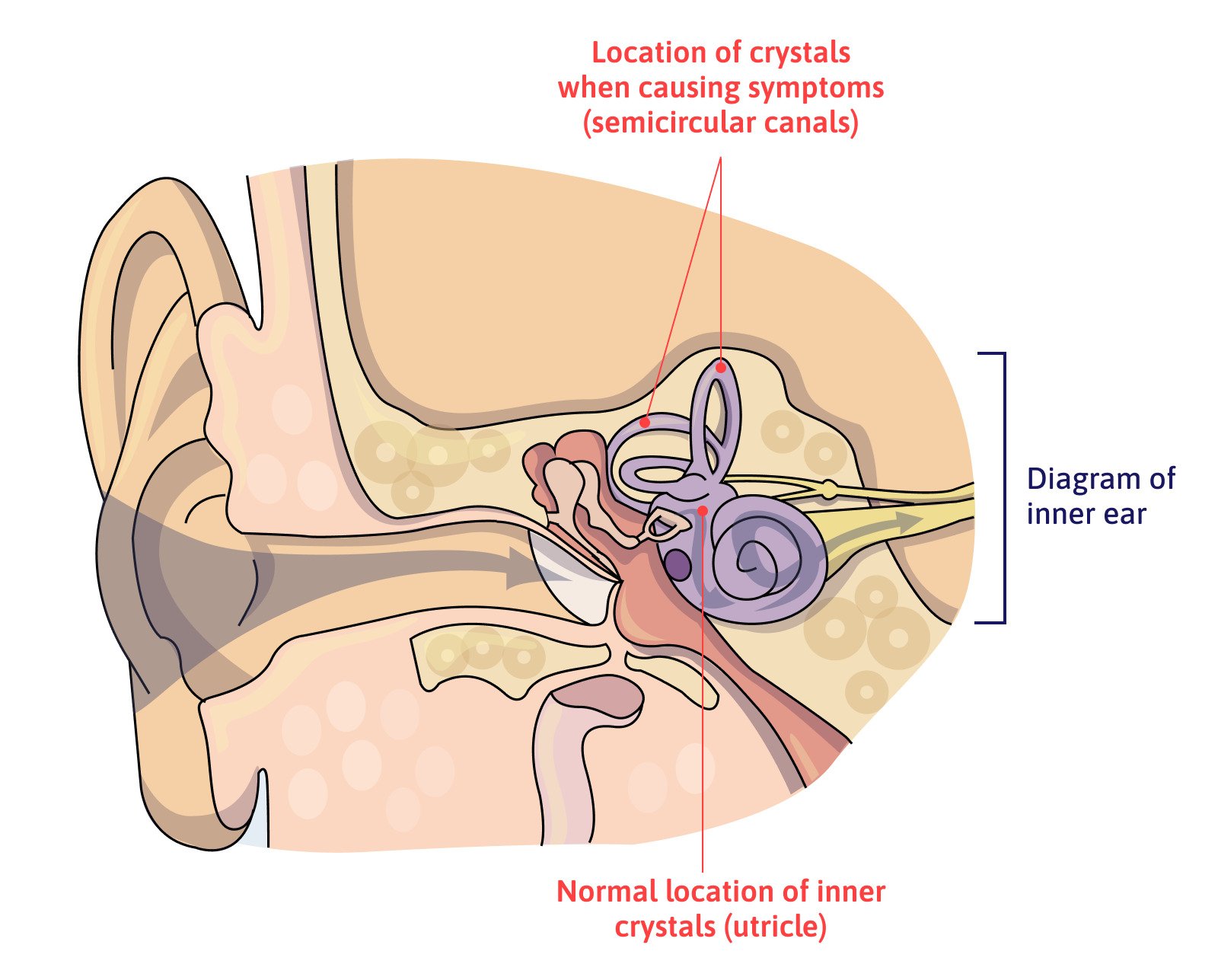
The risk of developing BPPV is highest immediately after the head trauma, even if it’s a mild head injury. For patients who don’t experience this or other vestibular problems, after a few weeks, the chances of developing BPPV eventually decrease to what’s found in the general population. In contrast, patients who experience BPPV after the head injury have a higher rate of recurrence, and about half will experience at least one more episode in the years after the original head injury. Most of the time, it is readily treated with canalith repositioning maneuvers, but some patients may also need vestibular rehabilitation.
For example, one of our patients did not initially experience vertigo after her injury. But years later, she started taking medication that aggravated her dysautonomia. At the same time, she developed and was diagnosed with BPPV. Although it’s impossible to determine whether BPPV was related to her concussions or not, this, combined with ANS dysfunction, disrupted the communication between her vision and vestibular system. She started experiencing severe vertigo and lost her ability to drive.
While her condition improved after treatment of the BPPV, she required additional therapy to help her eyes and ears work together in harmony again. These symptoms wouldn't have been so severe if she hadn't had the old head injuries to make symptoms worse and treatment more complicated.
Post-traumatic Meniere's Disease
If you’re experiencing episodes of vertigo and dizziness accompanied by tinnitus, pressure in the ear, and hearing loss, your neurologist might diagnose you with post-traumatic Meniere’s syndrome (also known as post-traumatic hydrops).
These symptoms are caused by abnormal fluctuations in the fluid that fills the hearing and balance structures of the inner ear and may start immediately after the injury or years later.
Hormonal Disorders
Brain injuries can also damage the hypothalamus and/or pituitary gland, which are small structures responsible for regulating many of the body's hormones. This damage can lead to hormonal problems, which, in turn, increases the susceptibility of patients to developing vertigo and dizziness.
For example, there is some evidence to support that patients with deficits in thyroid hormone levels (which can be a consequence of brain injury) can experience vertigo and dizziness.
It’s a good idea to have hormone testing done by an endocrinologist familiar with post-traumatic hormone changes if you’re experiencing persistent symptoms.
Further reading: Post-concussion hormone dysfunction
Migraines
One of the most common symptoms after a head injury are post-traumatic headaches and migraines. In about 40% of patients, these migraines trigger vertigo episodes. These are known as vestibular migraines.
In addition to vertigo, patients may also experience:
- Imbalance
- Nausea and vomiting
- Dizziness
- Sweating
- Sensitivity to light, noise, and motion
- Tinnitus
- Hearing loss
- Feeling of pressure in the head
- Visual changes
- Numbness in the face
The symptoms build over the course of a few hours and leave the patient tired and drained. For many patients, migraine-associated vertigo manifests regularly and persists for several years.
Further reading: Post-concussion headaches
Side-Effects of Medication
Many patients experience vertigo as a side effect of prescription drugs. Examples of medications that may cause vertigo include anti-inflammatories, antibiotics, analgesics, and tranquilizers, as well as those used to treat blood pressure, heart conditions, and seizures.
Ask your health care provider if any of the medicines you take may be causing vertigo or balance problems. A change in medicine or dosage may fix the problem.
Further reading: Medication for post-concussion syndrome
Depression, Anxiety, and Other Psychological Disorders
Although most cases of vertigo directly or indirectly affect the vestibular system, it’s important to recognize that psychological disorders can also cause this symptom. This is called psychogenic vertigo.
Without treatment, vertigo can persist for months or years after the head injury, and each episode can last for hours, often accompanied by hyperventilation and feelings of fainting. For these patients, overwhelming situations, including crowded, noisy, or confined spaces, can trigger vertigo.
Some patients with psychophysiological vertigo find a combination of medication (antidepressants or anti-anxiety meds) and cognitive behavioral therapy helpful. Talk to your neurology or psychiatry specialist if you think this approach could help you.
Multidisciplinary Approach to Treat Vertigo Years After Head Injury

Treatment for post-traumatic vertigo and other balance impairments depends greatly on what’s causing the symptom. For some patients, medication or surgery (in rare situations) may be the best option, but most common treatments include canalith repositioning maneuvers (especially for BPPV) and vestibular therapy to restore healthier balance, posture, and vestibular and visual functioning.
Patients who have had to deal with vertigo and other persistent symptoms often need a more in-depth approach. Vertigo is usually just one of many head injury symptoms that persist. Instead of offering only one type of treatment or therapy, at Cognitive FX, we use a multidisciplinary approach that allows us to tackle the root issues underlying vertigo, fatigue, sleep disruptions, difficulty concentrating, memory issues, and so many more symptoms stemming from an old head injury.
After treatment, 90% of our patients report reduced symptoms. And many experience remarkable recoveries.
For example, Lori Montague shared in a Google review the transformation her daughter experienced:
"When she was 12 years old, she was a state champion competitive gymnast, a straight A honors student, and a pianist. Then she over-rotated in a tumbling pass at a gymnastics meet and landed on the back of her head. The concussion resulted in a traumatic brain injury that left her functioning at less than 20% in both the vestibular and the visual-scanning-memory brain centers.
She could no longer balance on one foot, or bend forward without feeling dizzy. Riding on an elevator would make her sick for at least an hour afterward. She could not read. She could no longer scan the music to play the piano. Her headaches were chronic and intense, limiting her daily activity to a fraction of what it had been previously. We spent many months in therapy with very competent therapists. They helped her regain the capacity for basic daily function. We are so grateful for them, and the part that they played in her recovery. But after all they could do, there were still many restrictions. She learned to read again, but she could only focus if the print was large. It was over a year before she could make it through a full day of school, and then she never made it through more than 2 or 3 days without having to take a rest day.
She could not test at school for more than a half an hour at a time. When she tried to do core testing on a computer, she made it 45 minutes, and then came home with a migraine that shut her down for 3 days. She could only play the piano very slowly. There was always pain behind her eyes. She told me that she didn't remember what it was like to not have a headache. She had not been pain free since the accident. She had almost no social outlets. Places with bright lights or lots of loud noise completely shut her down. I spent 2 and a half years protecting her and helping her learn how to balance her life to limit the pain as much as possible.
Then we found Cognitive FX. The doctors and therapists there were caring and competent. Every person we worked with was the best at what they do. They made the week positive, and kept my daughter motivated and hopeful throughout the treatment. In one week, they fixed her. I know that is hard to believe. I would not have believed it if I had not experienced it myself. But it has been 1 year, and my daughter has NO RESTRICTIONS.
The pain behind her eyes is gone. It was like there was a part of her that had been missing for 2 and a half years, and they gave her back to me. She is animated, happy, and excited about life. She never had to miss a day of school in the last year because of headaches or fatigue. She took the ACT test (4 hours of testing), scored well, and had no symptoms afterward. She can read any size print in any book. She can play the piano again. She can do flips off the diving board at the swimming pool. She can jump on the trampoline. She can ride on roller-coasters. She is once again a straight A honors student. She is one of the most advanced students at her ballet company, and she is on the high school ballroom dance team. She flips, and turns, and jumps, dancing 3 to 4 hours a day. She goes to football games, and watches fireworks. She has NO RESTRICTIONS. They fixed her."
Our team of specialists includes neuroscientists, radiologists, psychologists, a clinical neuropsychologist, and a host of therapists from different disciplines (physical therapy, occupational therapy, neurointegration, and more). They work together to evaluate and treat each patient.
Evaluation

Every patient undergoes a detailed medical evaluation with our team. This includes a review of the patient’s medical history, an assessment of symptoms, and a series of physical, cognitive, and psychological exams to assess:
- Balance, equilibrium, hand-eye coordination, and other physical responses
- Memory, problem-solving skills, executive function, and other cognitive skills
- Signs of anxiety, depression, or other mental health conditions
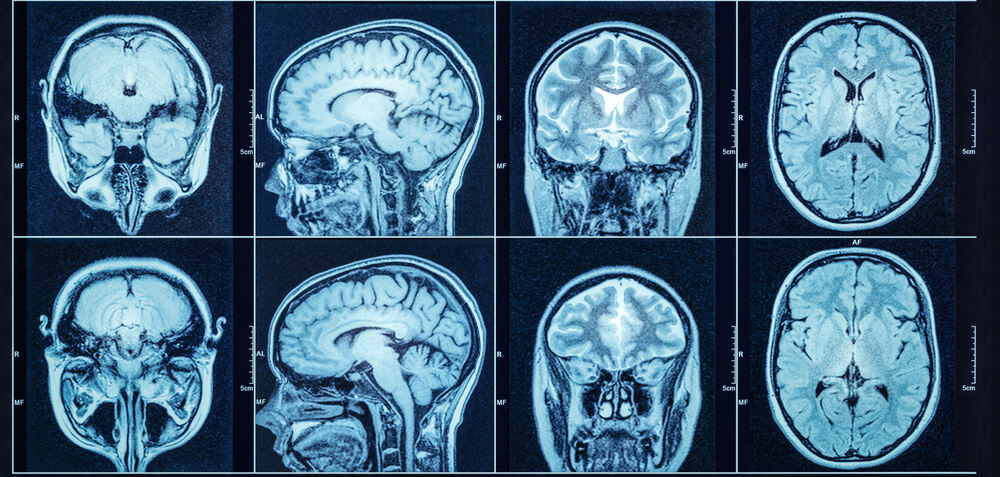
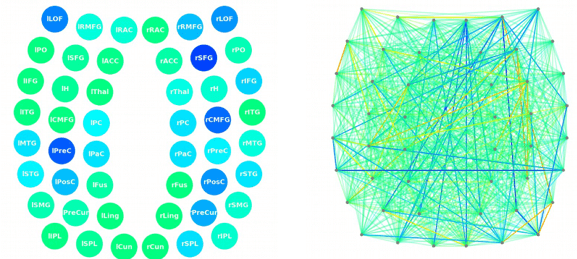
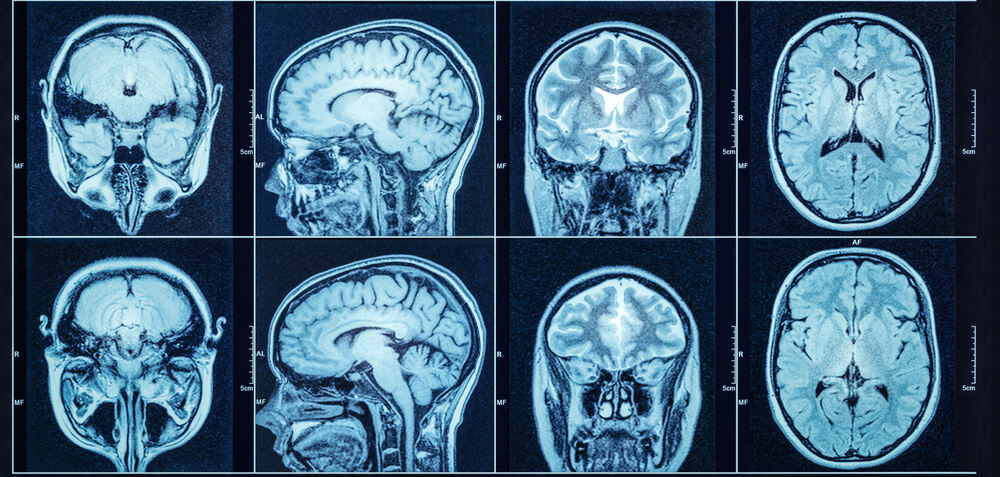
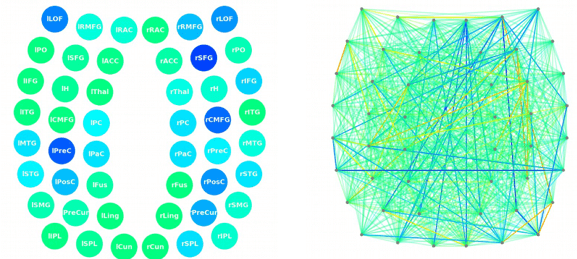
We also use state-of-the-art brain imaging technology to determine exactly how the head injury affected the brain. This scan, called functional Neurocognitive Imaging (fNCI), identifies which regions in the brain are affected by neurovascular coupling dysfunction.
In practical terms, the scan looks at how blood flows in over 100 different areas in the brain, as well as how these areas communicate with each other.
Once this initial evaluation is completed, our team combines all the results to design a custom-made treatment plan for each patient. We call it Enhanced Performance in Cognition, or EPIC for short. While patients complete many of the same types of therapy during their time at our clinic, the specific exercises used by the therapists are chosen based on scan results and evaluation performance.
Treatment
During treatment, patients cycle through a three-step process:

Prepare
In the prepare phase, patients engage in short bursts of aerobic exercise on the treadmill or stationary bike to promote healthier blood flow in the brain. This step takes advantage of a phenomenon called the post-exercise cognitive boost (PECB). PECB triggers the release of important neurochemicals that improve cognitive abilities and help the brain respond more effectively to therapy.
Patients who struggle with physical activity or experience severe episodes of dizziness and vertigo triggered by exercise can still make progress in these sessions. Our therapists are trained to adapt these exercises and help patients recover without triggering severe symptoms.
Activate
After exercise, patients complete a series of different therapies, including:

For patients with vertigo, two of the most important therapies are vestibular therapy and neurointegration therapy. These therapies are essential to address autonomic dysfunction and vestibular problems, which are the most common causes of post-traumatic vertigo.
Vestibular therapy involves exercises that help patients manage vertigo, dizziness, and other balance issues. Typically, this includes habituation, gaze stabilization, and balance training exercises. We’ve written in more detail about vestibular therapy and what we do at Cognitive FX.

During neurointegration therapy, our therapists guide patients through a series of exercises to help both vision and vestibular systems communicate better with each other and the brain. We may combine therapy for the vision and vestibular systems at the same time.
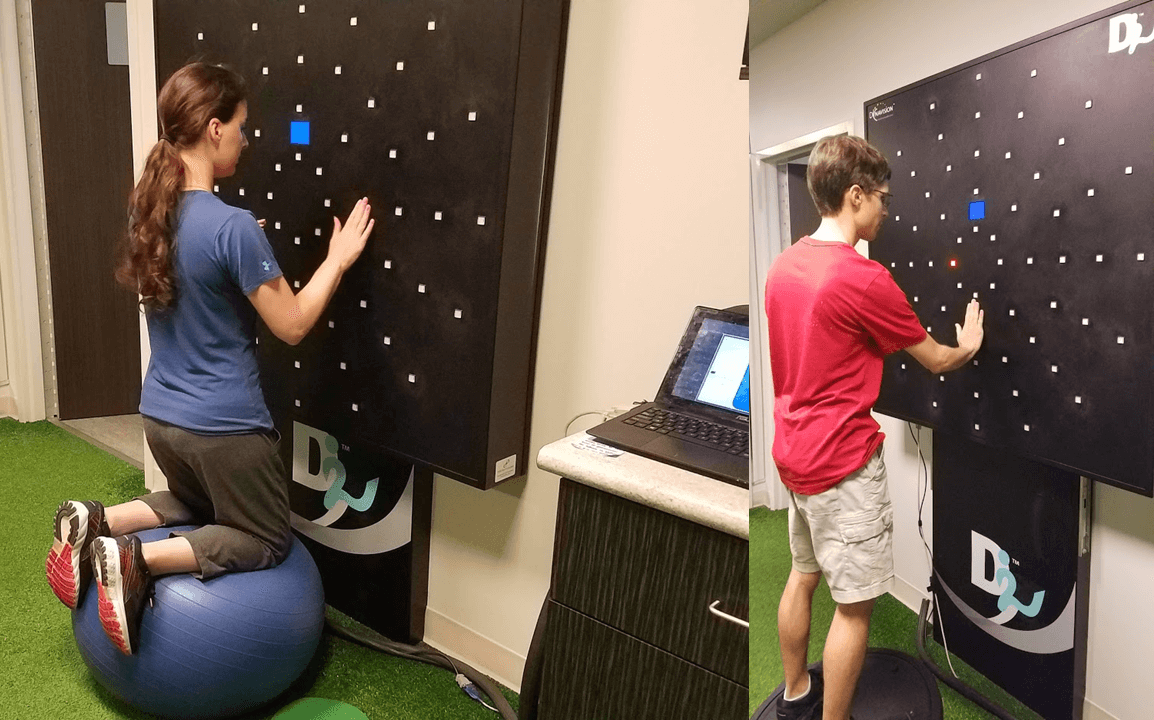
For example, we use a device called the Maverick, which is shaped like a giant diamond. In each vertice, there’s a light and a number or a letter. Patients follow a specific sequence by touching each light to help the body get all the systems “talking” to each other in a healthy way.
Recover
The third step involves periods of rest, which allows the brain to recover before repeating the process. This includes mindfulness exercises, massage of the neck and shoulders, and listening to Brainwaves (which work in a similar way to meditation).
Patients progress through this three-step sequence repeatedly during treatment. At the end of treatment, patients undergo a second brain scan and meet with one of our therapists to go over their results and receive a series of exercises to do at home.
Homework typically includes physical exercises, cognitive activities, visual and vestibular exercises, and some relaxation techniques. Ideally, patients should do these exercises for about an hour five times a week after treatment but can reduce gradually as symptoms improve. If patients need further therapy, we can recommend suitable specialists.
Recovery Stories
.png?width=900&height=675&name=can%20a%20head%20injury%20cause%20vertigo%20years%20later%20(1).png)
One of our patients, Myrthe van Boon, was taking three pills per day to control her dizziness. After treatment at Cognitive FX, she no longer needs any medication for vertigo.
“I think the improvement is more than 80%. I could never have dreamed that I could have had this life again. For me, it's worth everything. Every day, I’m so grateful that we did this,” she shared.
Read more about how Myrthe recovered years after a skiing accident.
Another patient, Olivia Seitz, suffered a series of concussions in her childhood. She didn’t connect the head injuries to her symptoms, leaving her puzzled as to why she couldn’t exercise without feeling dizzy, focus on her textbooks, or calm down after a mild scare.
Before treatment, she shared, even small crowds were difficult to handle. But just a few weeks after treatment, she wrote, she “handled Thanksgiving celebrations with over 23 people (13 children under age 10 and over 10 adults) with ease. Instead of finding a quiet corner and staying there all evening, I helped prep food, chatted with multiple people at one time, didn’t get a headache, and had at least as much energy and enthusiasm as the others in attendance!”
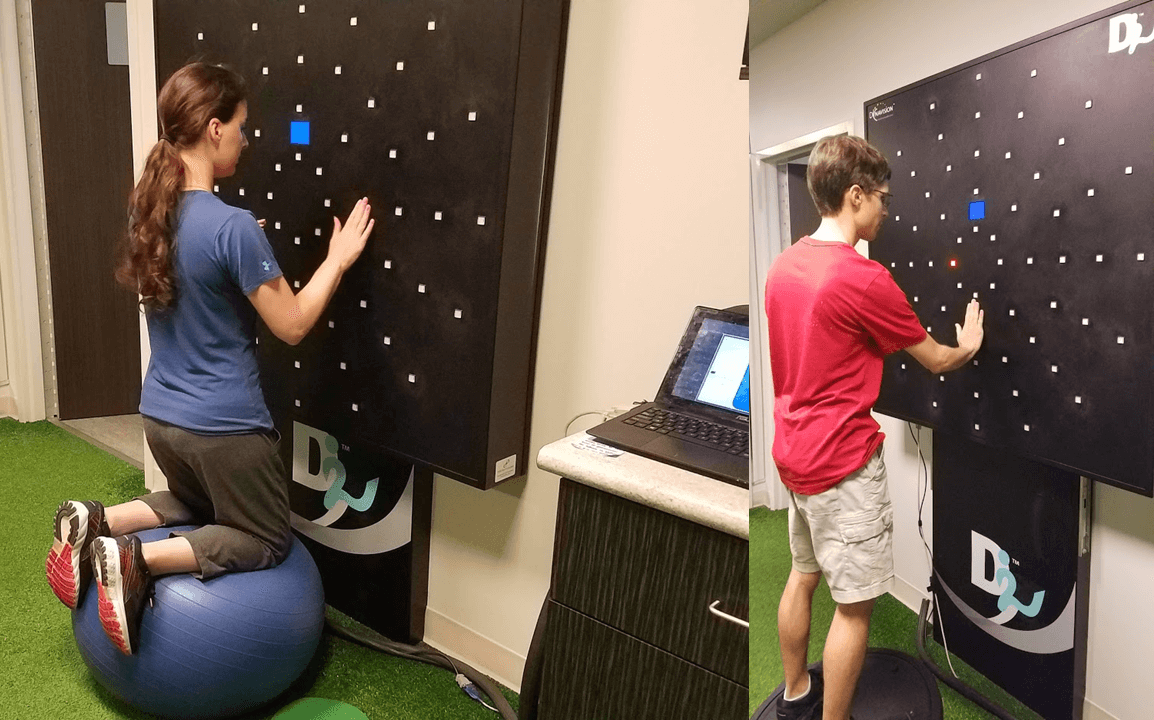 Doing Dynavision with a special twist (don’t worry, most patients don’t do therapy while kneeling on an exercise ball).
Doing Dynavision with a special twist (don’t worry, most patients don’t do therapy while kneeling on an exercise ball).
Read more about how Olivia recovered years after figure skating concussions.
Interested in more recovery stories? You can dive through patient video testimonials here.
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.

.png?width=1600&height=985&name=can%20a%20head%20injury%20cause%20vertigo%20years%20later%20(6).png)





.png?width=900&height=675&name=can%20a%20head%20injury%20cause%20vertigo%20years%20later%20(1).png)