“I feel like there’s a tight band around my head.” “My head feels like it’s blowing up like a balloon.” “I have a constant pressure headache.” “I feel like my head is being pulled apart between the eyes.”
These are comments we hear daily from patients with post-traumatic headaches (headaches resulting from concussion or another brain injury). Many patients report that their post-traumatic headaches “just feel different” from a normal headache. This is because the cause and presentation of post-concussion headaches are noticeably different from other headaches.
At CognitiveFX, we treat post-traumatic headaches as well as many of the other common symptoms of concussion in patients whose symptoms persist for three months or more (a condition commonly known as post-concussion syndrome). Many of our patients ask the same questions about their headaches, so we’ve put together this guide to help you understand:
Post-concussion headaches are complicated, and there’s still much work to be done in understanding why and how they happen. They don’t always respond to medication; sometimes it takes other therapeutic interventions to bring them under control. But treating them is key — the prevalence of headache in mild TBI patients is 47–95% (comparatively, a smaller but not negligible 20–38% of moderate to severe TBI have them).
At Cognitive FX, we focus on treating the underlying cause of the headaches instead of just masking them with medications. If you’re experiencing symptoms (such as headaches) that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function. To see if you are eligible for treatment, sign up for a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
Post-Concussion Headache Locations and Causes
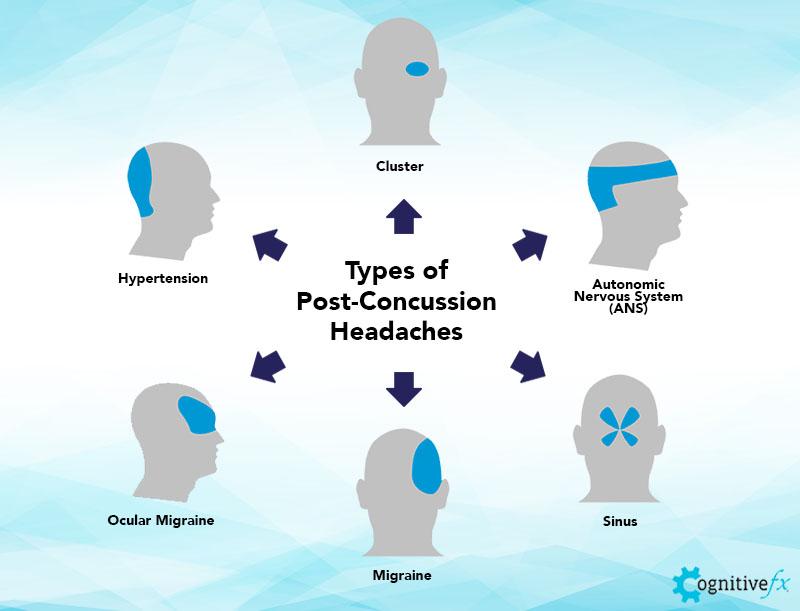
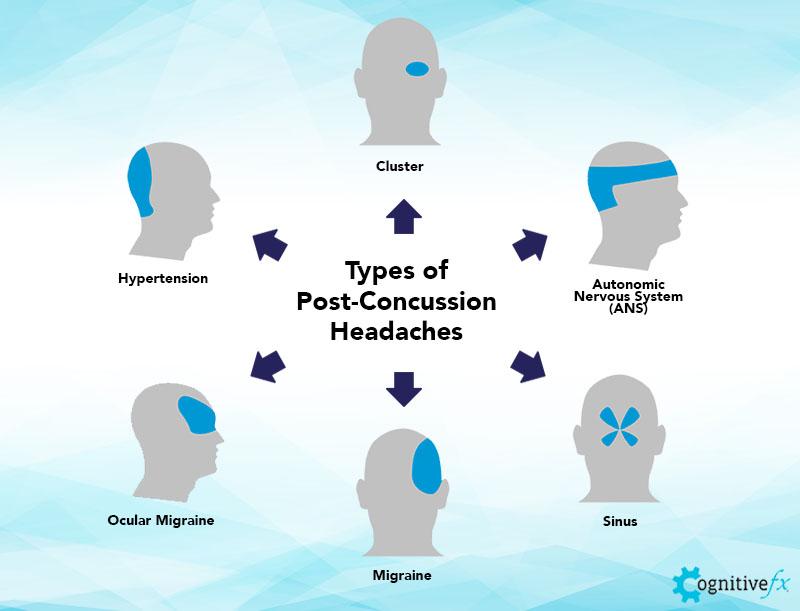
Headaches can come in many forms. Above are some examples of the way patients experience a headache and their potential ‘type’ or location. Patients may experience one, several, or all of these types depending on their situation.
Post-post-traumatic headaches can be pretty distinct from “normal” headaches (think dehydration-type headaches, sinus pressure headaches, etc.) and can present in various forms. In some instances, patients will report experiencing more than one type of post-traumatic headache, but they are complex in their presentation, their cause, and their treatment. We’ll explore more about their causes and presentation in the sections below. In this section of the guide, we’ve outlined some of the more common post-concussion headache types:
Additionally, you can check out our online course that covers which types of headaches you can get after a concussion, as well as specific techniques for coping with those types of headaches. If you want to learn how to manage your headaches at home, visit our course.
Cervicogenic and Autonomic Nervous System (ANS) Headaches
Cervicogenic and Autonomic Nervous System (ANS) headaches are some of the most distinct headaches after a head injury. They can cause similar headache “types” after concussion or brain injury. Many of the patients we see in our clinic experience both.
Cervicogenic headaches are often associated with neck tension, neck pain, and a pulling feeling along the neck. They are related to issues with the cervical spine (the neck bones and disks) and the musculature in the neck and shoulders. These often follow whiplash-associated injuries, but may also be subsequent to ANS dysfunction.
Further reading: Treatment for post-concussion neck pain
How are the cervical spine and ANS related with regard to headaches? Both of them involve problems with vascular (i.e., blood vessel) or cerebral blood flow (i.e., occurring in your head) and can often be associated with feelings of pressure. Cervicogenic and ANS headaches are closely connected, and many patients have both, so we assess and treat each patient’s headaches on a case-by-case basis.
In the following sections, we’ll explain more about what causes ANS headaches, what they feel like, and what makes them worse.
How Autonomic Nervous System Dysfunction Leads to Post-Concussion Headaches
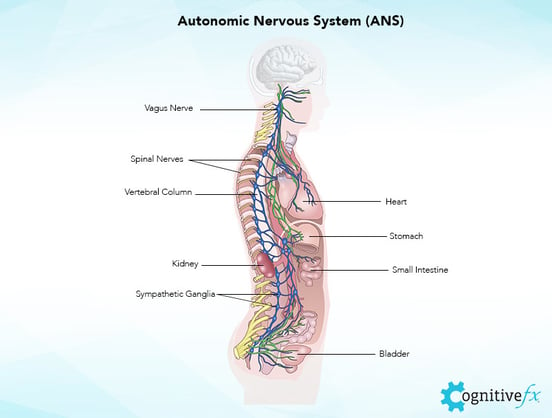
The autonomic nervous system controls heart rate, respiration rate, vascular constriction and dilation, and many of the other bodily functions we don’t think about that keep us alive. It has two parts: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS and PNS regulate your “fight or flight” and “rest and digest” processes, respectively.
Normally, these two are balanced like a set of scales so that we can respond to our environment appropriately. After a head injury, however, the fight or flight system (SNS) may tend to dominate, leading to a variety of common symptoms, such as exercise intolerance, headaches, fatigue, memory problems, sleep disturbance, and more.
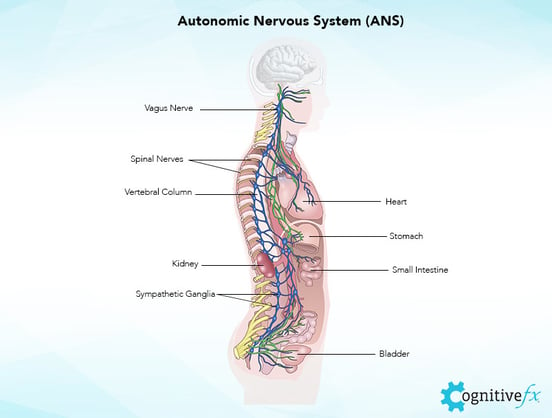
For example, you may initially be startled when you hear a loud sound, but you recover and rebalance when you realize it was a dish dropped on the floor. When the autonomous nervous system is dysregulated due to a mild head injury, the SNS can more easily dominate the PNS and prevent your body from returning to a ‘normal’ resting state as quickly as it should. In other words, the sound of a dish falling may cause your “fight or flight” reaction to linger.
Why does this matter? It has lasting effects on your stress levels, your blood pressure, and other functions regulated by the ANS — including post-traumatic headaches.
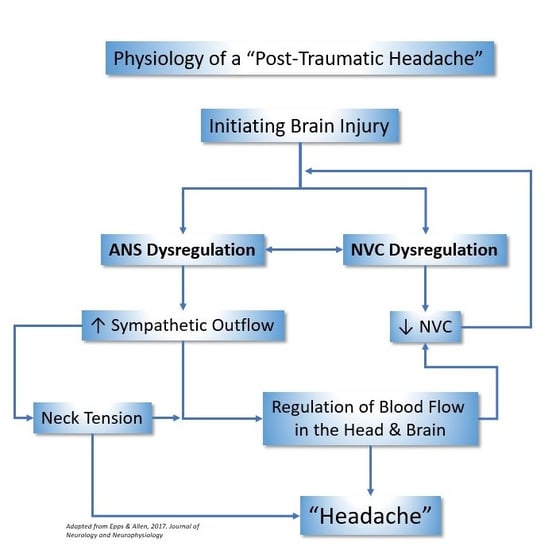
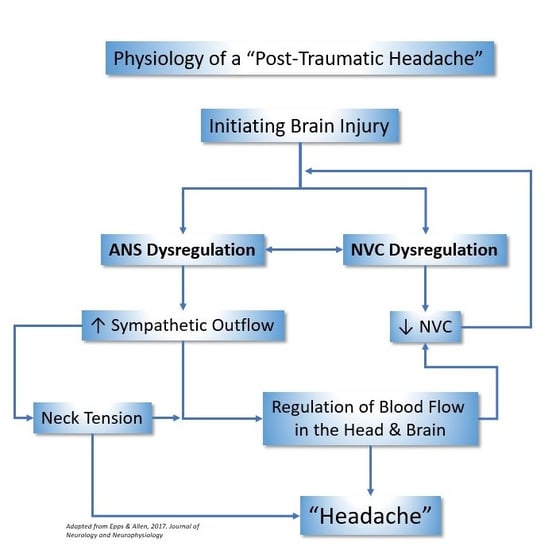
How does this specifically come into play for post-traumatic headaches? There can be many physiological sources. Autonomic nervous system dysregulation leads to increased tension in the neck. In addition, concussions can disrupt the regulation of blood flow to, from, and in the brain. As a result, patients experience tension and pressure in the head.
For example, you may feel like your head is blowing up like a balloon. This tension generally starts in the back of the neck and moves up around the eyes. Because ANS dysfunction impacts cerebral blood flow, it interacts with another cause of post-concussion headaches: neurovascular coupling dysfunction.
How Neurovascular Coupling Dysfunction Contributes to Post-Concussion Headaches
Neurovascular coupling (NVC) is the connection between neurons and the blood vessels that supply them with oxygen. During head trauma, your immune system causes inflammation in the affected parts of your brain. Any part of the brain affected by a concussion can experience a communication breakdown that may or may not be restored after you heal from the initial injury.
Think of the signaling between neurons and blood vessels like road traffic. A healthy brain would distribute “traffic” — i.e., the signaling and blood flow dynamics needed for a task like reading — equally along existing pathways. Neurovascular coupling dysfunction is like getting stuck in a traffic jam or taking a frontage road instead of the highway. It’s inefficient and requires more “gas” to get to the same destination. Even when there’s no physical brain damage, there’s a real change in the brain’s ability to function.
Brain regions impacted by NVC dysfunction either can’t call for enough blood flow to complete their tasks or they call for far too much, making it harder for the brain to do its job well. Other neuron clusters in nearby regions have to step in and do the job for them, but it’s easy for them to become overloaded.
The more your brain is affected by NVC dysfunction, the more likely you are to experience symptoms like headaches. Many patients notice that their headaches get worse when they try to complete cognitive tasks; NVC dysfunction is why. The good news is that we know how to treat NVC dysfunction, which we’ll discuss more in the treatment section of this post.
The effects of NVC dysfunction (which affects blood flow dynamics within the brain) and ANS dysfunction (which affects blood flow into and out of the brain) can combine to make your post-concussion headaches worse.
Headaches from post-concussion syndrome may improve with time, but most do not resolve unless treated. Want our help in understanding your headaches? Sign up for a consultation.
What ANS Headaches Feel Like
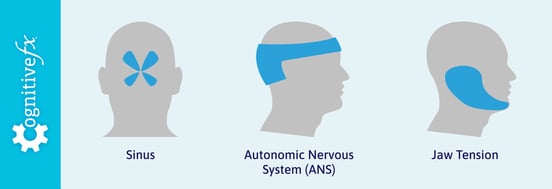
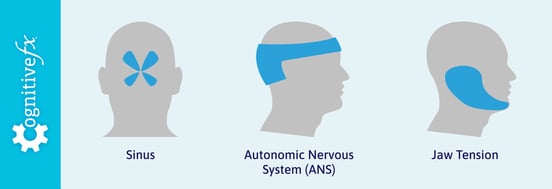
Autonomous nervous system headaches can present in a few different ways. They often are described as starting in the back of the neck and spreading up around the back of the head to the temples like a crown. This sensation is caused by gradual blood flow buildup and muscle tension from neck muscles.
Jaw tension-type headaches can also be related to autonomic nervous system dysregulation. It often begins around the back of the jaw and can move across the face and over the top of the head. You, your family, or even friends may note increased jaw musculature or teeth grinding associated with jaw-related head pain.
ANS headaches can also feel like sinus pressure headaches, with pressure or pain present around the nose and near the bridge of your nose and cheekbones (where the sinuses are located), then spreading through the head. Unlike allergy sinus headaches, the pain is almost constant; it does not change based on the time of day or exposure to allergens. Congestion may or may not be present.
In some less common situations, ANS headaches can also be accompanied by a soft bump or bumps on the head due to excess fluid pooling in a single location (also called “edema”).
Often, patients will describe a “moving headache” which incorporates many of the locations and profiles of headaches described here. This experience doesn’t mean your headache is untreatable! It just means that treatment will need to address each cause of your headaches, not just one or the other.
Finally, post-concussion NVC and ANS dysfunction are usually not the sole cause of your “headache” experience. Vision issues, genetic and environmental risk factors, and a multitude of other variables can make every person’s experience very different. After a concussion, people may have one, several, or all of these factors influencing their headaches.
Factors That Make ANS Headaches Worse
Autonomic nervous system headaches usually get worse with rigorous cognitive or physical activity. Although exercise may make ANS headaches feel worse, it is extremely important to keep exercising regularly. The headaches themselves do not cause injury (that said, pay attention to your body — ANS dysregulation can cause other problems including dizziness, nausea, or vomiting, and you should be aware of your limits). Exercise is important for recovery, even if it causes your headaches to worsen temporarily.
Stress also has a significant impact on headaches. The sympathetic nervous system becomes even more over-activated during periods of stress, further exacerbating autonomic nervous system dysregulation.
Finally, although stimulants and depressants (like coffee and alcohol) may provide temporary relief from a headache, they can actually make your headaches worse over time. Use discretion when consuming them.
Migrainous Headaches or “Migraines”
Another commonly reported type of post-traumatic headache is a “migrainous” headache. These typically present as an extreme, stabbing pain on one side of the head (or the other), generally near the top of the head.
Sometimes doctors and patients use the term “migraine” to describe any extreme headache. Just know that migrainous, severe, unilateral (i.e., on one side) headaches caused by a concussion often occur in individuals who have a predisposition to or family history of migraines. That said, they can also occur in individuals who do not have any history of migraines.
If you’ve ever experienced an “aura” before your headache, it’s probably migrainous. For example, an aura could show up as black or white spots in your vision, a strange smell, or tingling hands. An aura can be a good warning for some people to take their migraine pills or move to a safe area. These sensory disturbances may make a person extremely sensitive to light, touch, or smell. Up to 33% of people who suffer from migraine experience an aura (a sensory change or disturbance) right before the migraine manifests.
Although the exact cause of migraines is unknown, the neurovascular components of a migraine and a concussion are quite similar. For this reason, it is understandable that the physiological effects of a concussion can increase the frequency or intensity of migraines, especially for someone who is already predisposed to them.
It’s worth working with your doctor to determine if your headaches are migrainous or not. Understanding your family medical history, the effectiveness of migraine medication on your severe headaches, what triggers the headaches, and whether you experience an aura will help clinicians give you a diagnosis and treatment plan.
Other Concussion Symptoms Can Lead to Post-Traumatic Headaches
In addition to ANS headaches and migraine headaches, patients can experience a few other types of post-traumatic headaches.
Vision problems are common culprits. These headaches are more likely if you experience vision problems such as light sensitivity, difficulty focusing, symptom increases in visually busy environments, and so forth. The strain created by trying to overcompensate for any new vision issues leads to tough, pulsing headaches. These headaches generally involve the area around the eyes; your eyes may feel like they are inflamed or pained.
Further reading: Vision problems after a concussion
Vestibular issues can also lead to headaches. Your vestibular system, located in your inner ears, helps your brain to understand your position in space. Your body, vision, vestibular system, and brain all work together to help you move without symptoms. If a concussion affects your vestibular system, you might experience headaches, nausea, dizziness, balance issues, spatial disorientation, and more.
Further reading: Vestibular therapy after a concussion
Sleep problems after a concussion are another common culprit. If you aren’t sleeping well, your brain isn’t getting the rest it needs to function properly. One of the goals of our treatment program is to rehabilitate the regions of the brain involved in sleep (such as the thalamus). If your headaches are related to poor sleep quality, then you should notice them decrease in severity (or disappear completely) after treatment.
Further reading: Post-concussion sleep problems
What Post-Concussion Headaches Feel Like

Many concussion patients will say that post-concussion headaches ‘just feel different,’ or they ‘just know when they have one.’ The exact feeling can vary from person to person and from headache to headache. Often, patients can experience more than one of the post-traumatic headaches outlined above. Let’s just summarize here:
Concussion headaches can have a feeling of tension, tightness, and/or pressure. The feeling of increased pressure in your head is often indicative of an autonomic nervous system headache. Patients will describe these headaches as though there is a clamp tightening around their head or as though their head is a balloon that is being blown up. If a patient is suffering from an ANS headache, the tension might start in the neck and spread up to the top of the head.
With headaches caused by eye strain, the pressure might start behind the eyes and spread to the back of the head.
A sharp, stabbing pain might be indicative of a migrainous headache. These often feel similar to a normal migraine, but increase in frequency and intensity after a concussion.
Since there isn’t just one type of post-traumatic headache and the headaches vary from person to person, it is difficult to fully describe what a post-traumatic headache feels like. If you’re wondering if your headaches are post-traumatic headaches, start tracking them. Keep a journal of the location, cause, sensation, remedies, pain rating, and length of your headaches. The visual illustration we introduced earlier will be helpful here:
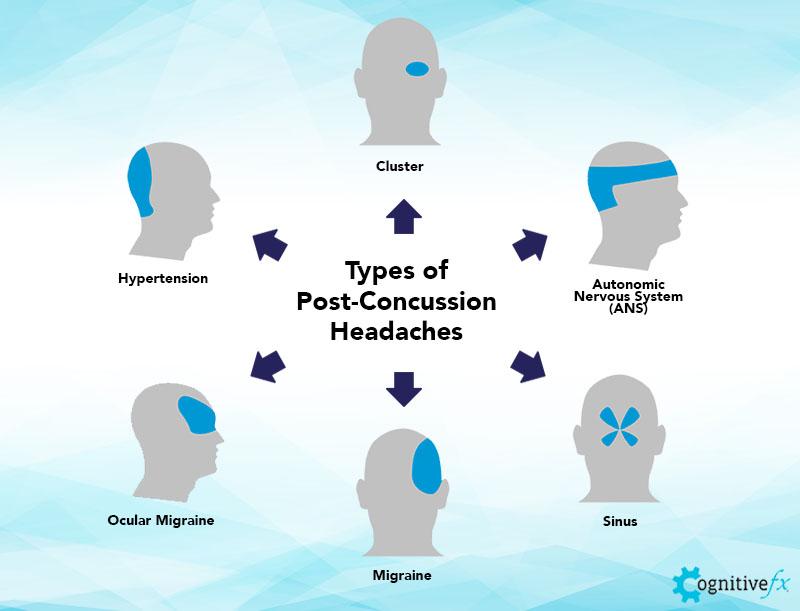
These are the most common headaches our concussion patients experience.
In identifying the type of headache you’re experiencing, remember to note the causes and any remedies. For example, a “normal” headache could be caused by not drinking enough water (and thus be remedied by drinking more water). But an autonomic nervous system headache may not respond to normal remedies, including medication; may persist longer than a normal headache (sometimes lasting weeks); and may worsen with exercise or cognitive activity. Writing down differences in what helps to alleviate headaches can help you understand the cause of the headache.
How Long a Headache from a Concussion Lasts

You can experience a post-concussion headache years after the original injury. It might be constant the whole time, or it might come back months or years later. The length of a post-concussion headache is highly dependent upon risk factors such as genetic predisposition, what type of brain dysfunction you’re experiencing, and what types of post-concussion headaches you’re getting. Contrary to popular belief, loss of consciousness or memory loss at the time of head trauma does not indicate the severity or longevity of postconcussive symptoms.
Most concussion symptoms, including headaches, resolve within 3-6 weeks. If you are still experiencing what you think are post-concussion headaches beyond that period of time, then it is unlikely your headaches will resolve on their own. Some patients go through “good” periods when their chronic headaches aren’t as bad, but any event that taxes the brain and autonomic nervous system can almost immediately bring back the headaches.
The length of a post-concussion headache can vary greatly from patient to patient. Regardless, persistent post-concussion headaches (and any other long-term effects) need the right treatment so that the source of the headache is being treated, not just the pain. Concussion headaches are unlikely to fully resolve without concussion treatment.
If you’re suffering from post-traumatic headaches, we can help. Sign up for a consultation with our team.
Treatment for Post-Concussion Headaches
The best treatment for post-traumatic headaches is to treat the concussion itself rather than medicate the pain. For example, ANS headaches won’t completely resolve until the autonomic nervous system is re-regulated, but this doesn’t just happen with time. Many people will speak with their healthcare professionals about medication options, and these may help with symptoms (potentially effective in the case of migraine medication) but may also not effectively reduce all headache pain. Or, the medications used may come with concerning side effects.
Below, we’ve provided a brief explanation of potential post-traumatic headache treatment options.
Medications
Depending on the type of headache, medication can bring some relief, but it’s a short-term solution. In the first 48 hours of a concussion, it’s safe to take Tylenol (acetaminophen) if you need pain relief. After that, you can take non-steroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen and Aleve (naproxen sodium). NSAIDs could be dangerous if you have any bleeding in the brain post-concussion, which is why you should not take them until 48 hours have passed since your injury. But they also might help more than Tylenol because they can decrease any remaining swelling and reduce muscle tension.
While over-the-counter pain medication is okay to take for a few days, it’s not a long-term solution. Then again, stronger headache medications are often not helpful; some can even perpetuate the headache (medication-induced headaches are also common in neurotrauma patients).
If you’re experiencing a true migraine, then migraine medications might help. For example, some patients find that migraine medications provide some relief because it helps with migraines, depression, and sleep quality. Unfortunately, many of the patients we’ve spoken to found it to be ineffective.
Beta-blockers can affect blood flow and are sometimes prescribed for post-traumatic headaches. But again, these do not resolve the source of the issues (dysregulated autonomic nervous system and neurovascular coupling), may come with undesirable side effects, and can leave the patient susceptible to medication overuse and dependence.
Many patients are referred to a neurologist for their persistent headaches and other symptoms of PCS. However, these doctors may or may not have training for PCS treatment and are likely to prescribe medication rather than therapy.
Further reading: What a neurology doctor can (and can’t) do for symptoms of post-concussion syndrome
Overall, treating headaches with medication isn’t ideal because it doesn’t solve the root issue, might cause side effects, puts additional strain on your liver (which may already be struggling due to ANS dysfunction), and may result in dependency.
Further reading: What to know about medication and post-concussion syndrome
Post-Concussion Headache Treatment: Addressing the Root Cause with Therapy

At Cognitive FX, we address the source of the headaches rather than just alleviating their severity. We provide our patients with therapy designed to promote neuroplasticity (the brain’s ability to change and to heal itself and the body). Using advanced imaging techniques (the fNCI scan), we can “see” which regions of your brain were negatively affected by your injury. That in turn helps us tailor your treatment plan to what your body needs.
During treatment, our patients go through an intense therapy regimen designed to kick-start neuroplasticity. Therapy begins with cardiovascular exercise to improve blood flow in the brain and to prepare the brain for cognitive exercises. Doing so boosts helpful neurochemicals such as BDNF that make therapy more effective.

Patients then complete therapy to address NVC dysfunction and accompanying cognitive deficits before resting and repeating the cycle. After cognitive exercise, the brain needs some recovery time to perform its best. The continual cycle of exposure to various exercises, tailored for each individual, helps disrupted pathways recover and improve neurovascular coupling.
Some of the therapies patients receive during their time at Cognitive FX include…

While treatment addresses physical and cognitive symptoms, over 70% of our patients report emotional symptoms, too. Many of these symptoms resolve after treatment, but certain mental health conditions — such as depression, anxiety, and post-traumatic stress disorder — need more time and treatment to resolve. All our patients meet with our clinical psychologist for additional evaluation and, if needed, referral for neuropsychological follow-up. For example, say you’re suffering from clinical depression and the antidepressant your psychiatry practitioner is causing unpleasant side effects. In that case, we might refer you to cognitive behavioral therapy.
As we mentioned earlier in the post, neurovascular coupling (NVC) is the connection between neurons and the blood vessels that supply them with oxygen, which is often damaged as a result of mTBI. Improving NVC is important for recovering from a concussion since vascular issues are so connected to ANS dysfunction and post-traumatic headaches.
At our concussion treatment center, we work with patients whose concussion-related physical and cognitive impairments didn’t go away with rest and time. Neuroplasticity is at the center of their concussion recovery journeys. The brain’s ability to heal with physical therapy and cognitive therapy brings hope to our patients and to anyone else who has sustained a brain injury.
Note: If you’re experiencing post-concussion symptoms six weeks after injury, it is highly unlikely the headaches will resolve without treatment. On average, our patients’ brain scan results improve by 75% after treatment. They report a 60% improvement in symptoms after just one week, on average. To see if you are eligible for treatment, sign up for a consultation.
What Can You Do For Concussion Headaches at Home?

There are some simple steps you can take to help alleviate or reduce the pain of headaches after a mild TBI and improve your quality of life while you wait for treatment of post-concussion syndrome.
Avoid Stimulants and Depressants
One of the first things we recommend is to avoid stimulants or depressants, such as alcohol and caffeine. Although these may provide temporary relief, they can also exacerbate the underlying cause of your headaches. And according to the Centers for Disease Control and Prevention (CDC), drinking alcohol might lengthen your recovery time, especially during acute injury.
Reduce Stress to Ease ANS Headaches
For autonomic nervous system headaches, reducing stress is a very important part of any post-post-traumatic headache treatment plan. For example, you can practice mindfulness and mindful breathing daily, breathing in and out with a focus on your breath. Breathing in this manner helps to decrease the sympathetic nervous system and improve blood flow, along with many other benefits. Other stress reducers, such as using essential oils, can help alleviate headache pain and reduce frequency.
Apply Heat for Sinus Pressure
For persistent sinus pain and pressure, using a hot pad on the sinuses can help to open up the blood vessels and reduce the pressure. Adding in peppermint oil may also help to open up congestion and help with relaxation.
Stretch Your Neck for Cervicogenic Headaches
With spine-related cervicogenic headaches, simply stretching the neck can help to alleviate some of the muscle tension and pain.
Practice Screen Hygiene for Vision Headaches
For vision headaches, completing vision therapy and practicing good screen hygiene (keeping the screen far enough away from your eyes, using a blue light filter, and putting screens away before bedtime) may reduce post-traumatic headaches.
Stay Active and Eat Well
For post-traumatic headache treatment, it is important to stay healthy overall. Eat healthily, take supplements and vitamins as needed, and stay active. Although exercise may immediately make your headache worse, consistent exercise can help to alleviate your headaches over time by improving your cardiovascular health and ANS balance. Try exercising in intervals rather than all at once and taking breaks as needed to keep your symptoms to a manageable level.
Further reading: How to exercise safely after a concussion and another Nutrition for post-concussion syndrome
Consider Supplements and Flavonoids
Finally, flavonoids have been shown to improve cardiovascular health and reduce headaches. Other supplements that boost overall health and decrease stress can help as well. Consult your medical professional before starting and stopping supplements.
What to Do If Your Concussion Headaches Are Getting Worse
Any time your symptoms are consistently worsening, seek medical care from your healthcare provider. Your headaches may oscillate a bit in intensity day to day, but if your symptoms are progressively getting worse, this is a red flag.
If you have any of the symptoms of a severe traumatic brain injury — such as drowsiness, loss of consciousness, confusion, memory loss, extreme personality changes, seizures, slurred speech, and poor coordination — visit the nearest emergency department immediately.
Severe TBI aside, progressively worsening symptoms often mean there are multiple unresolved issues that still need treatment. Sometimes, a head injury is accompanied by a neck injury. Cervical spine abnormalities are one such cause of worsening pain in the head or neck. For example, if your headaches are getting worse, that worsening pain could be from muscle tension and a disk issue, which, if untreated, could cause spine damage.
Contact a healthcare professional soon about your worsening symptoms and seek medical attention. They might order a computerized tomography scan (CT scan) or magnetic resonance imaging (MRI) to further investigate your injury.
If you are experiencing persistent post-concussion symptoms and want to resolve their underlying cause, schedule a consultation to see if our treatment can help you. On average, our patients see a 77% improvement after treatment at our center specializing in neuroplasticity-driven therapy.