“No one ever told me my concussion could cause depression.”
Again and again, we hear those same words from patients. Maybe they went to the emergency room (ER), or saw their primary care physician, or brushed it off and thought their head injury wasn’t a huge deal. They expect the headaches and the fatigue to last for a few weeks, but few are prepared for persistent symptoms (even though up to 30% of concussions result in long-lasting symptoms). Even fewer expect the emotional changes and mental battles that concussions can bring.
So if you’re suffering from post-concussion depression, know that you aren’t alone. Over 80% of our patients have reported symptoms related to mood or personality since their head injury (which developed into post-concussion syndrome). It really isn’t unusual for patients to suffer psychologically after a traumatic brain injury (TBI) or mild traumatic brain injury (mTBI).
With this post, we hope to answer some of your questions and help you understand how to move forward on your recovery journey. We’ll cover:
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What Is Depression?
The word depression is really an umbrella term; it can be used to describe various mental health conditions. For the purposes of concussion patients, we take “depression” to mean a disordered mental state, characterized by having some combination of these types of feelings:
- A negative feeling that goes beyond normal sadness (it might feel a bit like grief, but you recognize it as being distinct from grief)
- Low or no motivation, such that your ability to do what you need or want is compromised
- The inability to feel pleasure (anhedonia)
- A persistent disinterest in things (apathy)
- Feeling of emotional heaviness or like you’re moving through mud
- Feeling empty or robotic
- A negative outlook about yourself, the world, and/or the future
- A sense of worthlessness
- Indecisiveness
- Suicidal ideation.
Note: If you are experiencing suicidal thoughts, please seek help from a qualified medical professional. You matter, and you can get better. In emergencies, call the National Suicide Prevention Hotline at 1-800-273-8255.
Again, depression can have different causes, risk factors (like family history), and expressions. In this post, we’re focused only on the most common types of depression for post-concussion patients. If you experienced signs of depression prior to your head injury, whatever caused your depression previously may also be at work now.
How Can Concussions Cause Depression?
There’s more than one way for concussions to result in depression. The most common way, especially for people who haven’t previously experienced depression, is overactivation of the behavioral inhibition system (we’ll explain what that is in a moment). That said, it can sometimes stem from other issues such as hormone dysregulation and sleep disturbances.
Let’s explore each.
The Behavioral Inhibition System: A Common Cause of Post-Concussion Syndrome Depression
Before we discuss what goes wrong because of concussions, we need to explore how your brain is supposed to work.
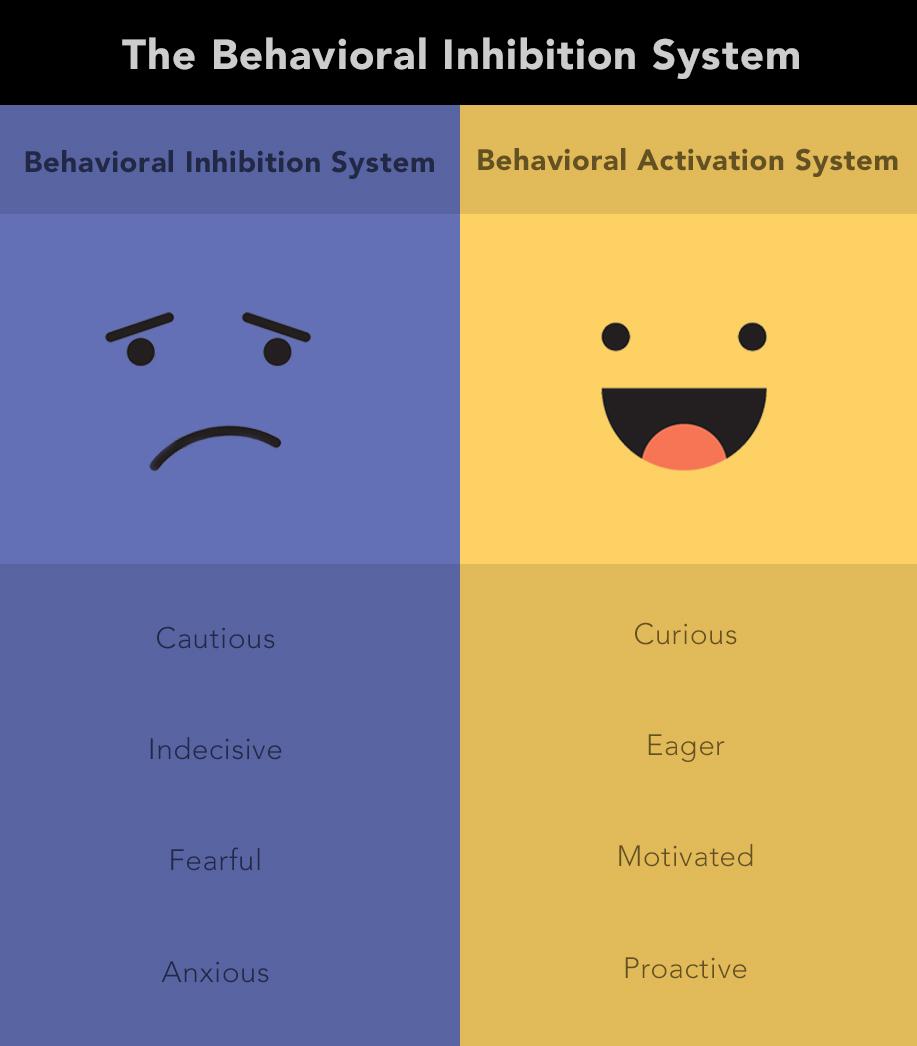
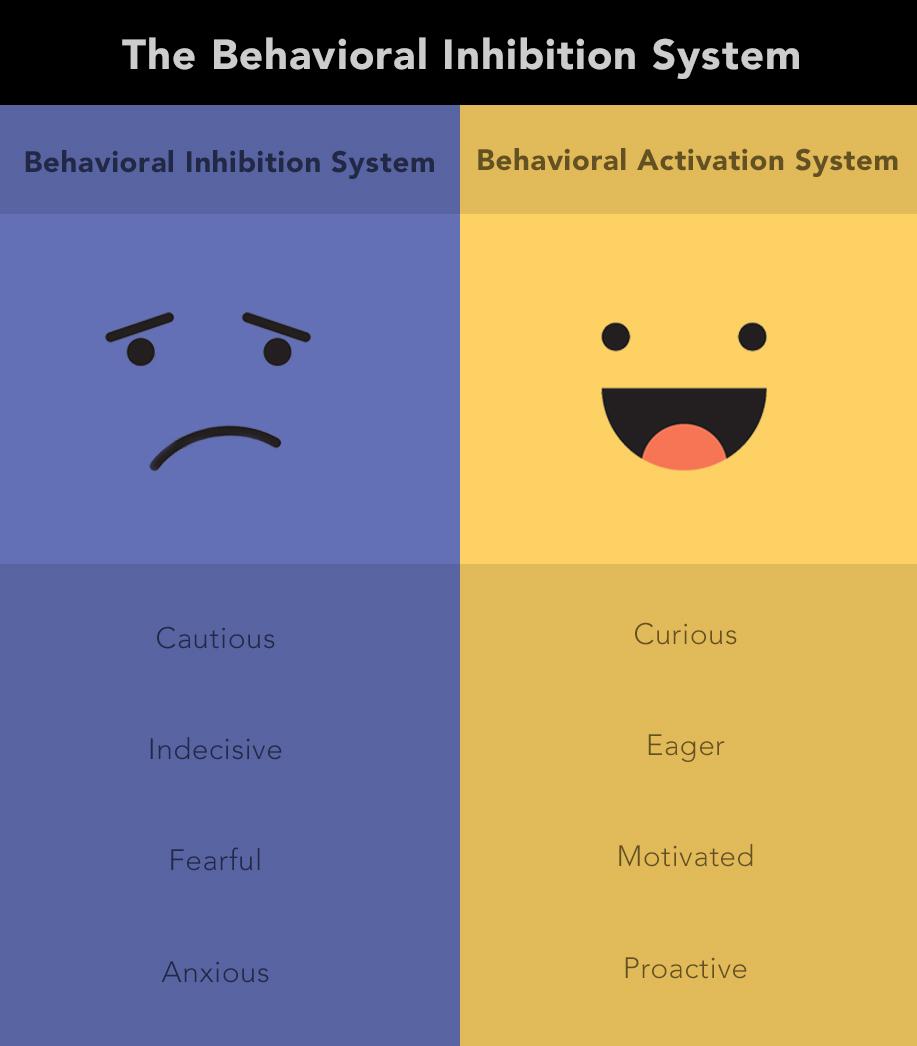
Each of us has a behavioral activation system and a behavioral inhibition system. They monitor and reward (or suppress rewards for) our behavior. When the behavioral inhibition system gets triggered too often, depression can result.
How Behavioral Activation and Inhibition Work
You can think of the behavioral activation system as our brain’s default setting. It makes us curious and eager to learn. It helps us feel rewarded for mastering a topic or experiencing something pleasurable. It’s an important part of why we engage with the world and the people around us.
But in the background, the behavioral inhibition system is monitoring everything we do. It’s watching out for loss, and it tells us whenever we’ve experienced a loss. And if we experience what it believes are too many losses, it pulls back on the reigns, dampening (or completely disrupting) the behavioral activation system.
For example, think of your activities like investments in the stock market. If you invest in stocks and win, you feel great! When you lose, you feel disappointed or maybe even regretful. But when you lose money repeatedly, you might start to reconsider your investments; you might even pull out of the stock market altogether because the cost to you is just too high, and there is little or no return on your investments.
Similarly, every time you experience a loss, your behavioral inhibition system takes note. It’s effectively saying, “Hey! You! You lost something. That mattered to you.” It’s an important system — if we didn’t notice when we lost the things that matter to us, we’d lose a whole lot more than we do.
But when we lose something really big — or lose a lot of smaller things all in a short span of time — the inhibition system wants to clamp down on what we’re doing and have us withdraw (to protect us). Loss of loved ones, health problems, job loss ... There are plenty of ways for that inhibition system to decide we need protection.
How Behavioral Inhibition Leads to Depression After a Concussion

That leads us to concussions. If you get a concussion and recover within a couple of weeks, your chances of staying emotionally stable are pretty good. But if your symptoms linger, it’s another story entirely.
You might lose socialization, work, autonomy, or even the ability to communicate the way you used to because of concussion symptoms. Disengagement from anything you used to do (whether it’s because of postconcussion symptoms or COVID-19) is really hard on your mental state and quality of life.
Because of that, lingering post-concussion symptoms are strong activators of the behavioral inhibition system. And once that system is in control, it can prevent you from feeling pleasure or from feeling rewarded when you do something that used to make you feel satisfied in an effort to protect you from further loss. And when that inhibition system looks toward the future, all it sees is more loss, resulting in feelings of hopelessness.
As if that weren’t frustrating enough, concussion patients face a double-whammy: Not only is that inhibition system overactivated, but they’ve lost many of the activities that could jumpstart their behavioral activation system (which would help calm down the inhibition system and allow feelings of reward and pleasure again).
Think about it: Physical symptoms such as headaches, noise and light sensitivity, and fatigue, along with cognitive symptoms such as brain fog, memory problems, and poor concentration, make it difficult to work or attend school, engage in social outings, or even get some exercise. So recovery really can feel impossible.
The result? People who feel really crummy, experience multiple losses, and don’t know how to get better. Often, our patients are surprised by how they feel. For example, sometimes parents will talk about how they think they must be monsters because they can’t feel anything, even toward their kids. They struggle to care about anything and reveal how they never knew how terrible it could be to feel nothing or be so robotic.
It’s so important to understand: There isn’t something wrong with you for feeling this way. Your brain — specifically, your behavioral inhibition system — is just trying to protect you from further loss, and it’s messing with your feelings in the process.
Note: We still have some possible causes to explain, but if you want to skip to the part of the article where we talk about treatment options, click here.
What If You’ve Had Depression Before?
The explanation above is mainly intended for concussion patients who had never experienced depression before their head trauma. But a decline in brain health could trigger another depressive episode in patients with pre-existing depression.
If you’ve experienced depression before, you may have experienced recurrent episodes (this is most common). The onset of each depressive episode can often (but not always) be tied to a life event. A concussion is definitely a big enough deal to trigger another episode of depression, primarily through the loss system as described above.
Hormone Dysfunction: A Less Common (But Very Real) Culprit
Many people don’t realize that hormone dysfunction can follow a concussion or TBI. The hypothalamus and pituitary gland (both located in the brain) are the main directors of our hormone production. Like any other region in your brain, if they’re injured by a concussion, they may not function properly.
You might experience changes in thyroid hormone, growth hormone, cortisol, estrogen, testosterone, and potentially other hormone levels due to the injury.
Hormones have a powerful effect on our moods. If your thyroid hormone is low, for example, you might feel sluggish, tired, less interested in activities, and irritable. Hormone imbalance can easily decrease your sleep quality and can affect your immune system. While we don’t know if hormone dysregulation can directly cause depression, it can be a contributing factor for some patients.
In addition, concussions can disrupt your brain’s production of brain-derived neurotrophic factor (BDNF). While the research is not settled, dysregulated BDNF levels could also contribute to the depressed state.
If we suspect that hormone dysfunction is contributing to your condition, we’ll recommend tests to confirm or reject that suspicion. If the tests show any problems, we’ll refer you to an endocrinologist for treatment.
Disrupted Sleep and Other Symptoms: Reinforcing Depressive Feelings

While they’re not often a direct cause, other symptoms of concussion can work in concert with your loss system (and/or hormones) to worsen or reinforce depressive symptoms. Many post-concussion syndrome patients experience disruption to their sleep, and sleep deprivation itself can result in depressive symptoms. Additionally, the symptoms of depression can make it harder to sleep, so they work together to make everything feel worse.
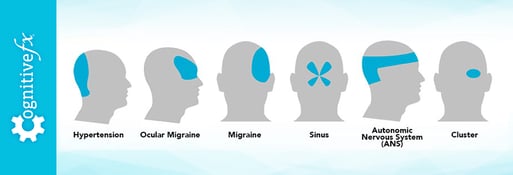
Being in pain all the time is another factor. It’s harder for your brain to believe it’s safe to go back to normal if it’s busy reacting to headaches, feelings of overwhelm, brain fog, and so forth.
Finally, all this can lead to altered habits (not exercising, not eating right) that further contribute to the depressed state. Even though it may be difficult, try to eat well, rest as best you can, and exercise regularly (for more, see how to exercise safely after a concussion).
When Something’s Wrong, but It’s Not Depression
Sometimes, patients feel “down” but aren’t experiencing depression. In these cases, they’re often aware that they’re not exactly depressed, but that there’s still something wrong. Often, what they’re really experiencing is grief.
You may be familiar with the five facets of grief: denial, bargaining, anger, sadness, and acceptance. Not everyone experiences all five, and they might not experience them in that order; they might bounce back and forth between the five facets.
The “sadness” stage of grief has some similarities to clinical depression: You may experience feelings of loss, emptiness, and sadness. You might even experience some disinterest. But key differences between grief and depression are feelings of worthlessness, low motivation, apathy, meaninglessness, hopelessness, and suicidal thoughts. Depression sufferers often have these features whereas those suffering from grief generally don’t.
When grief is at the heart of your mood, your depression-like symptoms often will resolve more quickly than depression once you’ve been through treatment for post-concussion syndrome. Because grief doesn’t activate the behavioral inhibition system as strongly as depression does, these patients often have an easier time experiencing reward and joy from returning to normal activities.
Seeking Treatment for Post-Concussion Depression

When is it time to seek treatment for post-concussion depression? That depends on a few factors. Always seek treatment if you’re experiencing suicidal ideation.
If you can tell that how you’re feeling is interfering with your day-to-day life, that’s a good sign to seek treatment.
And honestly, if you’re asking the question, “Should I get treatment?” the answer is probably yes.
That said, there are two types of treatment to pursue: treatment for post-concussion brain dysfunction and treatment for depression. If you’re still experiencing symptoms in addition to depression months or years after your concussion (or concussions — many of our patients have a history of concussions), then we strongly recommend getting treatment; those symptoms are unlikely to resolve without professional intervention.
The outcome of post-concussion treatment can then determine whether you need follow-up care from a psychologist or other mental health care provider regarding your depression.
Treatment for Post-Concussion Syndrome Depression at Cognitive FX
When you come to Cognitive FX, we use functional neurocognitive imaging (fNCI, which is a special kind of functional MRI) to determine the extent to which parts of your brain were affected by the concussion and in which way. We can see which regions are hyper- and hypo-active, then tailor your treatment plan to help your brain recover.
You can read more about EPIC treatment and how it works; if you’d like a first-hand account of treatment, one of our patients described her experience in detail here.
Resolving your post-concussive symptoms — issues such as headaches, fatigue, difficulty concentrating, and sleep problems that stem directly from your brain injury — can make an enormous impact on how you feel. Depression and other mental health problems like post-traumatic stress disorder and anxiety are often secondary conditions that develop after the injury but which don’t stem directly from the injury.
If your depression was closely connected with your primary symptoms, it may resolve quickly after you complete treatment for post-concussion syndrome. However, for some patients, treatment of post-concussion syndrome is a step in the right direction, but they need additional psychological treatment to overcome the depression.
While you’re at Cognitive FX, you’ll meet with a psychologist multiple times. We’ll do an in-depth psychological evaluation (in light of your complete medical history) to determine what’s causing your depression and any other emotional symptoms. We’ll make sure to explain what’s happening and what your options are for treatment going forward. We’ll also refer you to a psychologist in your area if further treatment is warranted.
In addition, if we suspect any of your symptoms are related to hormonal imbalances, we’ll order blood work. If you do have hormone dysfunction, we’ll refer you to an endocrinologist for further treatment.
Should Post-Concussion Patients Take Anti-Depressants?

Ultimately, the decision to take medication for emotional symptoms is the patient’s choice, but there are a few important things to keep in mind:
The literature on antidepressants is fairly controversial.
For most antidepressants, only about 30% of patients show a significant response to medication, roughly 30% show minimal improvement, and anywhere from 30-50% show no improvement.
So even if you don’t have a brain injury complicating things, taking medication for depression is a trial-and-error process. Typically, a physician will put you on one medication, wait 6-8 weeks to see if it has any effect, tinker with the dosage if needed (and then wait a few more weeks), and continue the process until a suitable medication is found. And that’s not to mention the medications you may have to quit taking throughout the process because the side effects were too unpleasant or dangerous.
Antidepressants can have many side effects.
Speaking of side effects, antidepressants have a lot of them, and those side effects could make your existing symptoms worse. If you’re working with a doctor who doesn’t intimately understand post-concussion syndrome, it can be challenging to differentiate between symptoms and side effects.
Most post-concussion depression can be treated successfully without medication.
If you haven’t experienced depression before your head injury, you likely have what we’d call situational depression, which most of the time can be treated without medication. Medication has a very low chance of being helpful if your main issue is (as discussed above) overactivation of the behavioral inhibition system. It’s not primarily a biochemical or neurochemical problem, so a biochemical solution isn’t going to fix it.
So what should you do?
Each person’s situation calls for careful consideration. If we had to make a general recommendation, it would be to wait on the medication until you’ve at least undergone treatment for your post-concussion syndrome and, if needed, psychotherapy.
What Comes After Treatment?

Even when you’ve gone to treatment for post-concussion symptoms, your recovery doesn’t stop there. It’s good to do “homework” to continue your recovery. Here are two of our recommendations:
- Try to engage with the people you spent time with and the passions you had before your injury. Doing so can help jumpstart your behavioral activation system and convince your behavioral inhibition system that it’s OK to back down.
- Try to look at what’s happened to you not so much as a setback as an opportunity for growth. Reflect on what you’ve learned and how it’s helped you become a better person (more empathetic, for example), spend some time examining your belief systems, and consider whether your priorities have changed post injury.
Finally, remember that having post-concussion syndrome or depression doesn’t make you “wrong.” You’re not crazy. What you’re going through is something many other people have gone through and recovered from. By learning about your condition and seeking treatment for yourself, you’re on the right track to recover, too.
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, schedule a consultation.