Depression After a Concussion or Brain Injury
Depression, one of the five stages of grief, may be the most familiar, and frustrating, feeling experienced after a traumatic brain injury (TBI) or concussion. And it’s not a fun one. Depression is a...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
People who have suffered a mild traumatic brain injury (mTBI) often experience difficulties with their psychological and emotional health. For example, among the patients we treat at our clinic, it’s common for them to deal with feelings of grief, depression, and various forms of anxiety including increased worry, overwhelm, and even panic or PTSD. This is especially true for patients who develop persistent physical and cognitive symptoms lasting months or years after their injury.
If you or a loved one has experienced this, the most important thing to understand is that treating these conditions in the context of a head injury is distinctly different from treating these conditions in patients who haven't had a head injury. Namely, treating anxiety and depression when you have a mild TBI needs to include treating the physical and cognitive symptoms of the TBI alongside the psychological symptoms.
In this article, we share examples to demonstrate why this is true, discuss the most common forms and causes of depression and anxiety that our patients experience, and share how we treat their mTBIs alongside their emotional symptoms for significantly better results.
Below, we cover:
Over 80% of our patients have experienced emotional symptoms after a concussion. Many of those symptoms resolve shortly after treatment at our clinic (although serious mental health issues like depression and anxiety can take additional therapy to resolve). If you’d like to learn more about how we can help you, book a consultation.

To understand why treating depression and anxiety in the context of brain injury is different from treating these conditions in patients who haven’t had a TBI, it’s helpful to look at some examples that we commonly see among our patients. Let’s begin with how people with mild TBIs typically come to feel depressed.
If you get a concussion that leads to persistent symptoms that fail to resolve within the weeks after your injury (what’s known as post-concussion syndrome), your life can change pretty drastically. Physical symptoms such as headaches, noise and light sensitivity, fatigue, and cognitive symptoms such as brain fog, memory problems, and poor concentration, make it difficult to work or attend school, engage in social outings, or even get some exercise.
To make matters worse, finding support through your local healthcare system can be extremely difficult. It’s not uncommon for people to visit numerous types of doctors (including neurologists) and therapy offices over many months, and still fail to receive any treatment that helps them feel better. So recovery really can feel impossible.
Is it any wonder, with all of these symptoms, difficulty getting help, and inability to live their lives normally, that PCS patients begin to feel sad and grieve the loss of life before their injury?
We think depression and grief are very understandable emotional responses in the context of these life changes. However, if you try to treat these emotional symptoms with standard psychological treatments such as medication or psychotherapy, you fail to treat the root causes (i.e., their physical and cognitive impairments) that led to their emotional symptoms in the first place. While medication and therapy might dampen some of their depressive feelings, they won’t solve the underlying problems.
Similarly, as we’ll explain below, feelings of anxiety in mild TBI patients are often directly or indirectly linked to the functional changes in their brain that happened because of their injury.
For example, affected areas of their brain can lead them to experience overstimulation which can increase anxiety. Worry and associated anxiety can also result from life changes accompanying mTBI such as worry about being able to work, meet financial obligations, pursue goals, etc. Anxiety stemming from overstimulation and worry about the effects of limited functioning due to PCS both need to be addressed.
For these reasons, patients see much better results in resolving their symptoms when they treat their physical and cognitive issues alongside their psychological symptoms. For some patients reducing their PCS symptoms and getting back to their normal lives, reduces their depression and anxiety. For others, additional psychological treatments are necessary, but these patients are much better positioned to get better both psychologically and emotionally if they are also treating their PCS symptoms.
In the rest of this post, we’ll take a closer look at the specific forms that depression and anxiety can take in the mild TBI patients we treat, what causes these issues, and how we approach treating their TBIs alongside their emotional symptoms at Cognitive FX.

As we’ve discussed, feelings of sadness and depression are often accompanied by grief after a brain injury. When patients cannot engage in normal activities, such as work, sports, recreation, or hobbies that previously brought joy and meaning to their lives, they naturally begin to feel sad and grieve the loss of these activities and the person they were before the injury.
During the initial rehabilitation process, patients often receive plenty of medical assistance as well as support from friends and family members, but as time goes by and symptoms persist, the reality of living with a brain injury sets in and patients may struggle to adapt to their disability. This is especially true for patients who are not receiving any treatment for their symptoms or if treatments are not working.
Symptoms of depression and grief after a TBI may include:
It’s worth noting as well that changes in the brain as a result of a head injury can lead mild TBI patients to experience energy depletion, which can cause low motivation, fatigue, flat mood, and apathy. These symptoms can at times be misdiagnosed as depression, particularly by doctors who are not aware of the patient’s head injury. This is another scenario where treating the physical and cognitive TBI symptoms can help resolve the depressive feelings.
Related reading: Depression after a concussion: Why you feel this way + how to start healing
Anxiety is the other category of psychological disorders that our patients often experience after a brain injury. Most commonly it shows up in one or more of the following forms:
Patients with generalized anxiety feel an internal state of nervousness and restlessness accompanied by chronic worrisome thoughts and rumination.
As we mentioned above, this anxiety can stem from functional changes to the brain that lead to overstimulation. However, patients can also experience anxiety related to their physical and cognitive symptoms or life circumstances. For example, they might feel anxious going to the grocery store because it triggers symptoms such as light sensitivity, overwhelm, and headaches. Or, they might feel anxious about their finances because their TBI has caused them to stop working.
Our patients often describe their anxiety symptoms as:
To learn more about why patients experience anxiety after a brain injury, read our patient’s guide to post-concussion anxiety.
It’s not uncommon for patients with anxiety to also have panic attacks; however, one is not the cause of the other. Panic attacks are a dysfunction of the fear system rather than the anxiety system. They involve a fear reaction when there’s nothing actually present to fear.
Panic attacks can happen due to physiological reasons that stem directly from a brain injury or psychological reasons such as post-traumatic stress disorder. During panic attacks, many patients develop a fear of their physical sensations, which perpetuates and worsens the panic.
Since physiological or psychological factors can cause panic attacks, it’s important to have a psychologist or other medical professional sort out which one is causing your difficulties so you can receive the right kind of treatment.
Alongside their TBI, some patients also develop post-traumatic stress disorder (PTSD). In TBI patients, PTSD usually develops after a serious traumatic event, such as a bad motor vehicle accident, domestic abuse, or dangerous military situations.
Because many symptoms of PTSD overlap with the symptoms of mild TBI, such as headache, fatigue, dizziness, and anxiety, it can be difficult to determine if the patient has symptoms from their TBI, PTSD, or both. In the patients that have both, it’s crucial to understand that physical/cognitive TBI symptoms and PTSD are a consequence of the head injury (patients don’t develop PTSD as a consequence of their brain damage).
Post-brain injury PTSD can involve:
To learn more about why patients experience PTSD after head trauma and how it’s treated, read our patient’s guide to post-concussion PTSD.
Note: These are the most common psychological effects of brain injury that we see in the patients we treat at our clinic. This is not an exhaustive list of all the possible psychological symptoms TBI patients may experience, which can also involve perceived personality changes, impulsivity, emotional lability (teariness), mood swings, disinhibition, challenges with decision-making, and more.
Several times in this article we have mentioned that psychological effects from brain injury can stem directly or indirectly from functional changes that occur in the brain as a result of the injury. This is what we’ll dig into in this section.
Specifically, we’ll look at four common causes that can contribute to emotional changes in mild TBI patients:
Note: None of these causes can be treated with standard psychological treatment options such as medication and psychotherapy. They require specialized treatment like what we offer at Cognitive FX.
Patients can experience psychological effects if areas of the brain involved in controlling emotional and behavioral responses are directly affected by the head injury. Some of these areas include, for example, the amygdala, which is involved in the brain’s response to threats; the hippocampus, which is critical for memory and learning; and the thalamus, which is activated when people feel sad or angry.
If any of these areas are damaged by the injury, patients can experience dysregulation of their emotions. For example, a study showed that post-concussion syndrome patients also suffering from depression and anxiety had lower functionality in areas of the brain associated with the reward circuit and regulation of fear responses.
Another way TBIs can trigger psychological symptoms is due to the disruption of a mechanism in the brain called neurovascular coupling (NVC).
In a healthy brain, nerve cells request the resources they need to complete a particular task from a network of blood vessels. These blood vessels then ensure that the resources are delivered to the right place at the right time.
After a TBI, however, this dynamic connection can be disrupted such that cells don’t receive what they need and struggle to complete their normal functions. If this happens in the parts of the brain controlling behavior and emotion — including the temporal and frontal lobes, for example — it may trigger emotional changes, such as depression and anxiety.
The autonomic nervous system (ANS) controls a variety of bodily functions, including heart rate, blood flow, breathing, and digestion, using two subsections called the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS generates activation in the body to meet daily challenges and also prepares the body to react to threats if needed, while the PNS is the “rest and digest” part and helps the body with restoration. Under normal circumstances, these two sections work in harmony and change dominance as needed.
Even mild traumatic brain injuries, however, can disrupt this balance, causing the SNS to remain activated even when it’s not needed. This causes a series of physical symptoms, including increased heart rate and blood pressure, disrupted breathing, and digestive issues. Under normal circumstances, the PNS helps the brain engage and adapt to different situations in a calm manner. This means that TBI patients, who have limited PNS activity, cannot regulate their emotions as easily. As a consequence, they struggle to maintain focus when facing a challenging or frustrating situation.
Inevitably, patients feel overwhelmed and anxious, even during activities that wouldn’t normally be a problem. For example, they may lose their temper after being called for dinner two or three times when they are trying to read. This wouldn’t have happened before their TBI, but afterward, the effort needed to shift attention away from the reading to going for a meal becomes overwhelming. Patients often also experience physical symptoms, such as nausea, dizziness, and exercise intolerance as part of ANS dysregulation.
Many of the patients who seek treatment at our clinic also show signs of overstimulation. This happens when certain areas of the brain are not working properly (either due to a direct hit caused by the injury or indirectly due to neurovascular coupling disruption), and other areas of the brain try to compensate.
Inevitably, this is a less efficient way to perform specific tasks, and the areas that take over get easily overstimulated. As a result, patients can feel overwhelmed, anxious, irritated, and agitated, and at some point crash both physically and emotionally.
.jpg?width=1557&height=1072&name=Dr.%20Alina%20Fong%20with%20a%20patient%20at%20Cognitive%20FX%20(V2).jpg)
One common issue that we see in our patients is that their previous healthcare providers dealt with each symptom separately, typically with medication. Painkillers for headaches, antidepressants for depression, and sleeping pills to address sleep disturbances, to name just a few. The problem with this approach is that doctors don’t treat the underlying causes of these issues that their injury has caused.
At Cognitive FX, we know the key to treating mild TBI patients is to consider all the symptoms holistically. This includes physical, cognitive, and psychological symptoms, such as depression and anxiety.
Treatment starts with an in-depth patient assessment. Patients undergo a variety of exams, including:
During the initial evaluation, our team also looks for signs of ANS dysfunction, and a neurointegration specialist evaluates how well the patient’s inner ear, eyes, and body communicate with each other. We repeat the same tests at the end of the treatment to assess how much the patient has improved.
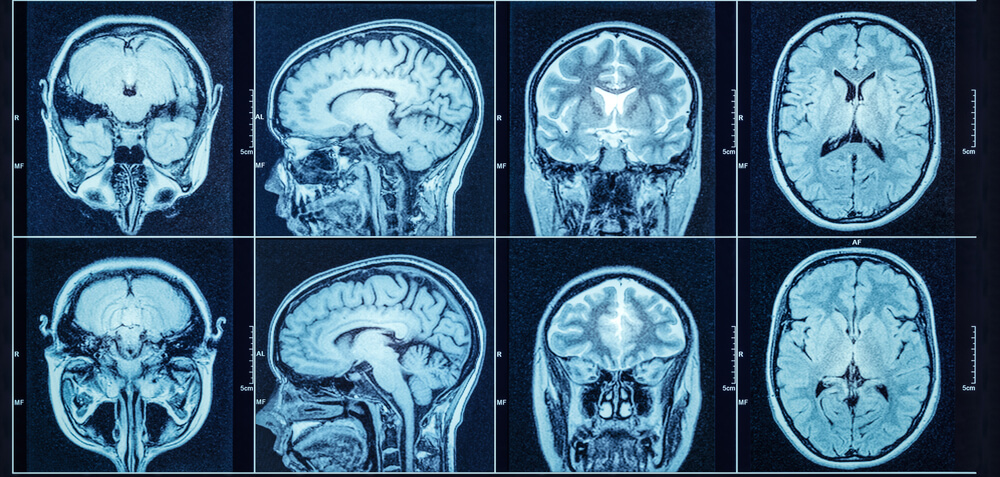
Our patient assessment continues with a brain scan called functional neurocognitive imaging (fNCI). In contrast to CT scans or standard MRIs, fNCI scans measure blood flow in 100 different regions of the brain while patients carry out a set of standardized cognitive tasks. They produce a series of real-time images that are combined and compared with scans from healthy people to identify the areas where neurovascular coupling (NVC) dysfunction is affecting normal brain function.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with NVC dysfunction.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
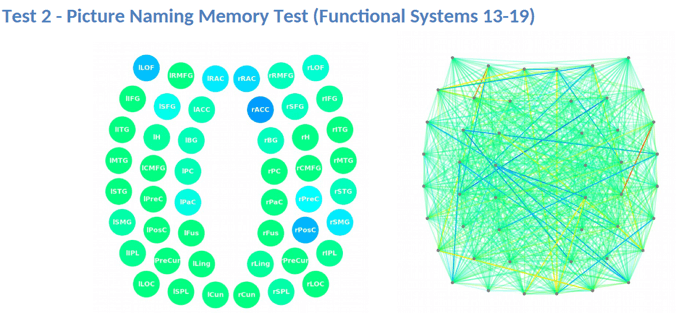
This information provides our staff with huge advantages when it comes to treating patients.
Once we’ve finished our patient evaluation, we use a combination of exercise and multidisciplinary therapies, including (but not limited to) cognitive, occupational, neuromuscular, and sensorimotor therapy.
![EPIC Treatment exercise with headphones [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg?width=2265&height=1425&name=EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg)
During cognitive therapy, you might listen to recorded restaurant sounds while listening to a therapist list random words. Your job would be to tune out the background noise well enough to identify opposite word pairs and tap the table whenever they happen (for example, “chair, table, south, up, down, band, stretch, dog, east, west…”).
Or, during sensorimotor therapy, you might be asked to state out loud arrow directions while stepping, tapping, and clapping in a four-step pattern along with a metronome. It might sound easy, but saying “right” while moving your left foot in time with a rhythm gets tricky quickly!
All of these therapies help your brain and body work together more healthily to alleviate physical, cognitive, and psychological symptoms. They’re based on the best neuroscience research available today. For example, addressing ANS dysfunction can help with anxiety, and dealing with physical problems can help patients feel less tired, which in turn boosts their engagement in life and well-being.
To make treatment as effective as possible, patients engage in supervised aerobic activity. Cardio exercise results in a Post Exercise Cognitive Boost (PECB): an increase of essential neurotransmitters and proteins in your brain that help develop and promote healthy blood flow. The PECB means your brain is in better condition to tackle the challenges we give you in therapy and engage in neuroplasticity for recovery.
For example, exercise releases brain-derived neurotrophic factor (BDNF), which has been shown to improve therapy outcomes for post-concussion patients.

Patients also meet with a psychologist at least twice during their treatment. These sessions aim to help patients understand which of their symptoms are caused by psychological or emotional issues ( and can be addressed with psychological treatments) and which of their symptoms are due to overstimulation, ANS dysfunction, or other neurologic dysfunction (and can be addressed by other staff in our clinic).
At the end of treatment, every patient gets a follow-up fNCI scan so we can see how well their brains are progressing. The average amount of improvement is a 77% reduction in symptoms! If patients keep up with their homework after treatment, they typically see further improvement at home.
We make sure that every patient has a tailored plan to continue appropriate therapy in their hometown (if needed). This aspect of recovery is far easier when the primary issue — brain dysfunction due to injury — is better.
If you’d like to learn more about how we can help you recover, sign up for a consultation with our team.

We recommend working with a psychologist or neuropsychologist to manage emotional changes until you’re able to receive treatment for TBI symptoms. In the short-term, there are a few things you can do (with or without the help of a therapist).
Identify your triggers, especially for overstimulation. What do you feel right before an angry outburst or before you get overwhelmed? If you know when you’re headed for trouble, it’s easier to change course. For example, some patients notice feeling brain fog, dizziness, or nausea.
If you’re comfortable with it, have trusted family members or caregivers monitor your overstimulation. They might pick up on cues that you don’t notice, like getting a glassy-eyed look. They can tactfully remind you to take care of yourself and destimulate.
If you’re a caregiver, just be aware that unsolicited interventions may not help the situation. For example, someone who usually would be comforted by a touch on the shoulder might get worse due to the additional sensory input. It’s important to talk to your loved one about what helps them or hurts them in the moment.
Speaking of destimulation, have a plan for when you’re getting overwhelmed. You might hide in the bathroom for five minutes (or any quiet room you can find), close your eyes for a bit, or even purposefully disengage from your current activity (e.g. if you’re stuck in a lecture hall, you might need to “space out” for a few minutes).
Do what you need to reduce environmental, cognitive, and emotional stimuli until you feel less stimulated.
Further reading: How to know when your brain needs a break (and what to do when you take one)
Name each emotion you’ve experienced post-injury. Examine how your feelings about yourself have been affected by these changes. Sometimes, just acknowledging and understanding what has happened to you can help.
Some folks have difficulty exercising after a concussion, but it’s still important to do whatever exercise you can do safely. It will help relieve stress and tension, plus it provides your brain with a biochemical boost to help it handle the day’s needs and may even help you manage other health problems. This post on post-concussion exercise can help you get started.
Don’t have anyone to talk to? Are you struggling with verbal expression of your feelings? Do you just need another outlet? Journaling can help with that. It gives you a way to process your thoughts and feelings on your timetable.
Support groups can be tremendously helpful for improving emotional well-being and quality of life. You can look for support groups for your specific emotional struggles (such as anger management), or you can follow the link to look for a post-concussion syndrome support group. Look for a group that encourages you and equips you with strategies to better manage your symptoms.
Long-lasting symptoms will not resolve without treatment. If you’ve experienced emotional problems and other common TBI symptoms for over three months, consider seeking help from a specialized care provider like Cognitive FX.
Note: While our program primarily serves patients with mild TBIs, in some cases we can help patients who’ve suffered severe injuries as well. For example, one of our patients feels “95% recovered” after a life-threatening fall that left her in a coma for three months. Follow the link for more information on our treatment for severe TBI patients.

Dr. Spangler is a Clinical Psychologist with over 20 years of experience working in both clinical and academic settings. She earned her doctorate degree in Clinical Psychology at the University of Oregon followed by a Postdoctoral Research Fellowship in the Department of Psychiatry at the Stanford University School of Medicine. Dr. Spangler served as a Professor of Psychology at Brigham Young University for 15 years where she directed training in Cognitive Behavioral Therapy for the Clinical Psychology Doctoral Program, and conducted research on the etiology and treatment of depressive, anxiety, and eating disorders. She also served as a Visiting Professor in the Department of Psychiatry Cognitive Therapy Centre at Oxford University in England. Dr Spangler has authored over 60 publications and has lectured worldwide. She has received numerous awards for her collective work from the National Institute of Mental Health, the American Psychological Association, the International Association for Cognitive Psychotherapy, the Association for Behavioral and Cognitive Therapies, the Beck Institute, and the National Association of Professional Women.

Depression, one of the five stages of grief, may be the most familiar, and frustrating, feeling experienced after a traumatic brain injury (TBI) or concussion. And it’s not a fun one. Depression is a...
Living with the lingering symptoms of a concussion for months or even years is life-changing. Patients with post-concussion syndrome (PCS) can feel worthless, misunderstood, lonely, and frustrated....
Mild or severe traumatic brain injury (concussion and TBI) can cause upsettingchangesto your mental health. Brain injury can worsen pre-existing mental illness or cause new symptoms — such as...

Living with the mental health effects of a traumatic brain injury (TBI) can be an isolating and overwhelming journey. Not all patients realize that brain injuries can cause significant emotional...

It should come as no surprise that COVID-19 — both the illness itself and all the situational changes that come with the coronavirus pandemic — is messing with our minds. Many people are experiencing...

After a traumatic brain injury or concussion, relationships can become strained. Communication can be difficult. Let’s be honest, thinking can be difficult. Sorting out your feelings and sharing them...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY