Between 80,000-90,000 people who suffer traumatic brain injuries (TBIs) each year develop long-term disabilities related to their TBI. Many others suffer from a variety of long-term, problematic symptoms that continue to interfere with their lives. When they try to get help for these issues, they are often told there’s nothing more that can be done — or worse, that there’s nothing wrong with them at all. Here’s the good news: Recovery can and does continue for patients who find the right help.
At Cognitive FX, we specialize in treating patients who suffer from persistent concussion symptoms, a condition known as post-concussion syndrome. However, we do treat those who have experienced moderate to severe TBIs as well.
While every situation is different, patients who have experienced permanent brain damage (such as cell death or even removal of parts of the brain) should moderate their expectations. Further recovery is always possible, and many of our patients have made life-changing progress as a result of their hard work in treatment, but the recovery journey is different for every person.
Traumatic brain injury is a complicated topic. So before we dig into treatment options and recovery, we’ll provide an overview of traumatic brain injury, its diagnosis, and its symptoms. If you want to skip ahead to a certain topic, you can use this outline to do so:
If you’re suffering from persistent symptoms after brain trauma, you’re not alone. Many of our patients struggle with headaches, word retrieval, feelings of overwhelm, and more before treatment. 95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. In addition, Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To learn if you’re eligible for our program, sign up for a consultation with our staff.
Note: Any data relating to brain function mentioned in this post is from our first-generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What Is a Traumatic Brain Injury?
There’s a lot of confusing vocabulary to describe traumatic brain injuries. To be sure we’re on the same page in this article, we’ll define some terms that are commonly used to describe TBIs, what causes them, and how we evaluate their severity.
Defining Traumatic Brain Injury
A traumatic brain injury is a brain dysfunction caused by an outside source. Very simply: damage occurs to the brain, and the brain doesn’t function normally after that.
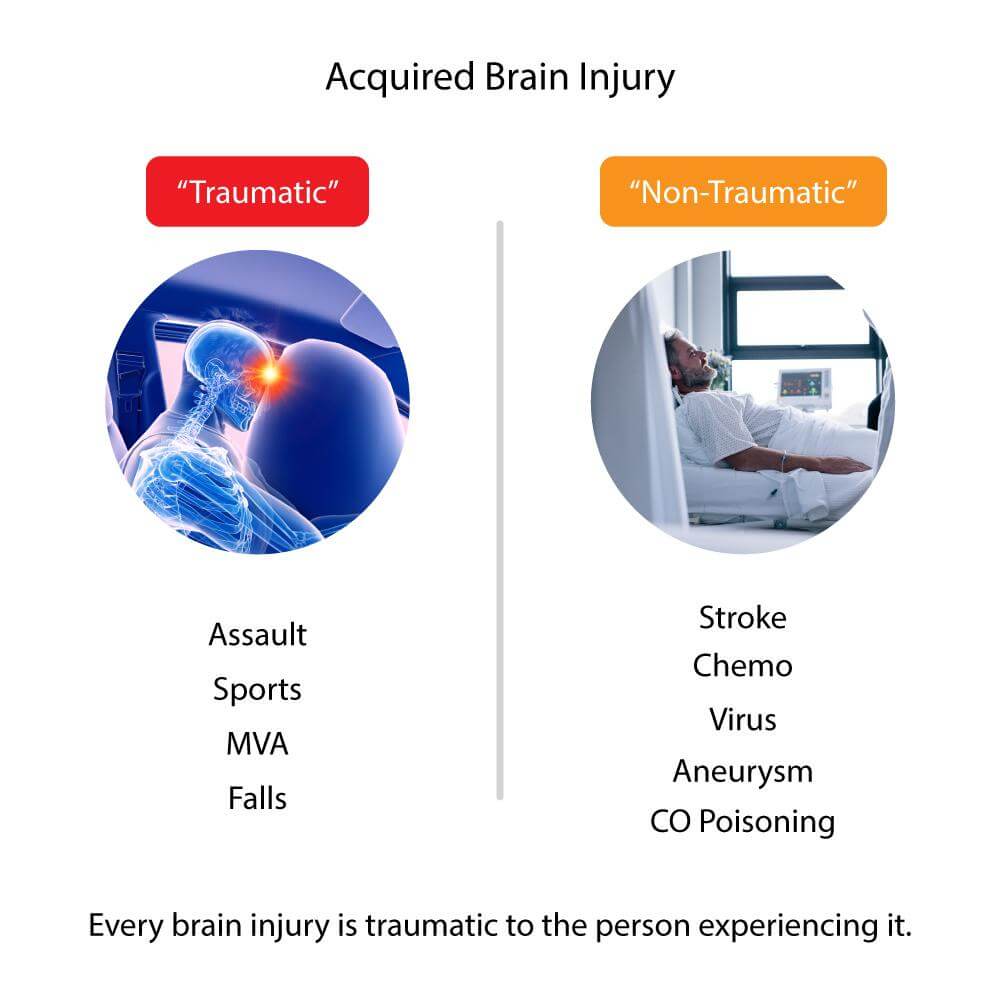
We refer to a brain injury caused by an outside source as an acquired brain injury, meaning it happens after birth. To be clear, other scenarios can result in brain damage that doesn’t come from an outside source. A non-acquired brain injury is a brain injury caused by genetic or hereditary factors, birth trauma, or a degenerative cause, such as Alzheimer’s disease or Parkinson’s disease.
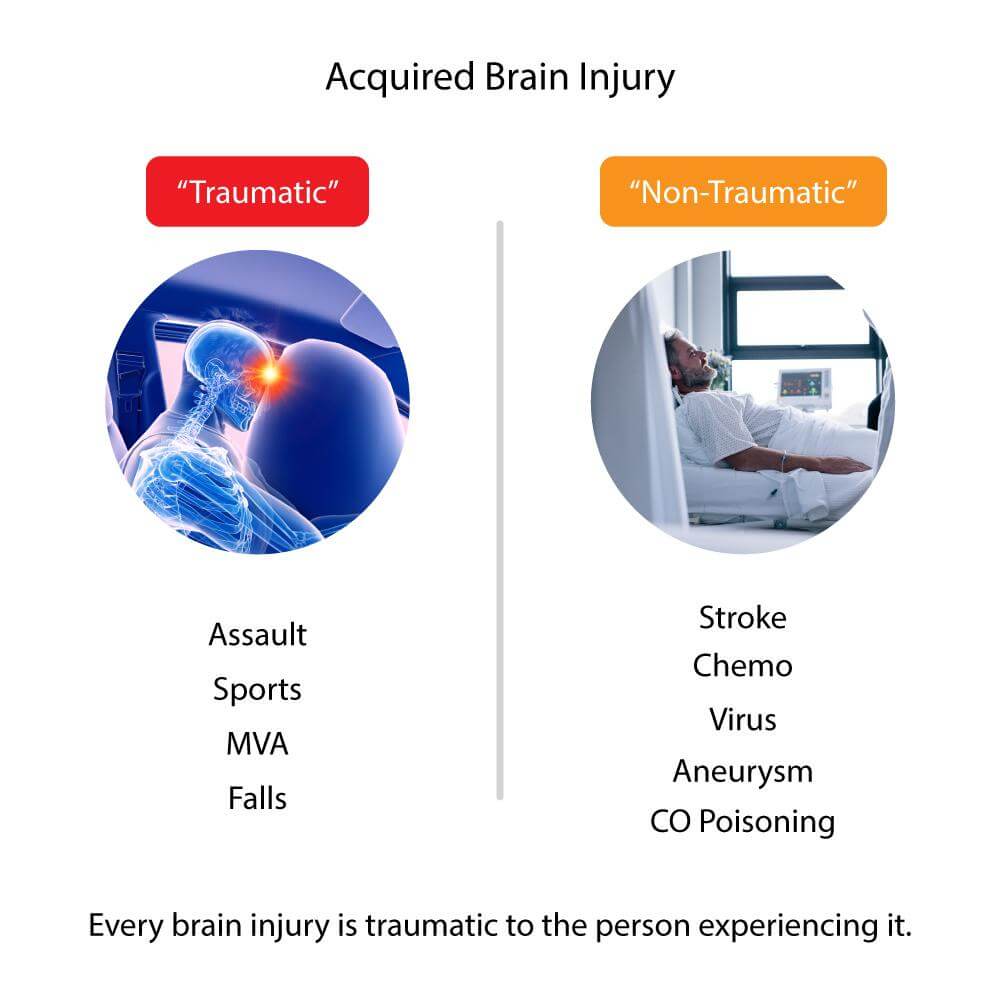
The medical community further divides the term “acquired brain injury” into the terms “traumatic” and “non-traumatic” acquired brain injuries for clarity. A traumatic brain injury is the result of some kind of outside force, such as an object hitting the head. A non-traumatic brain injury is the result of a “closed head injury,” such as a stroke.
We don’t like the term “non-traumatic” because it implies the injury and its consequences are somehow less frightening and distressing than a traumatic injury. Either kind of brain injury is traumatic to the person experiencing it, and they can both result in the same unpleasant, long-term symptoms.
When we refer to TBIs in this article, we’re talking about both “traumatic” and “non-traumatic” acquired brain injuries.
What Causes Traumatic Brain Injury?
Traumatic brain injuries (TBIs) have been on the increase since 2006 according to the Centers for Disease Control and Prevention (CDC). The CDC reported 2.53 million emergency department (ED) visits and 56,800 deaths related to TBI in the year 2014 alone. That’s a staggering number of brain injuries, and it doesn’t even include mild traumatic brain injuries (mTBI), commonly known as concussions, that didn’t result in a trip to the ED.
The majority of traumatic brain injuries are labeled as “mild concussions” that will hopefully resolve within a week or two of the injury. Moderate to severe TBIs might require hospitalization, surgery, and rehabilitation.
Most of our patients at Cognitive FX have suffered from long-term problems from a traumatic brain injury, but we can treat those with non-traumatic brain injuries as well.
Sources of Traumatic Brain Injuries
A traumatic brain injury often happens because of a direct blow to the head, but it can result from any jarring movement that causes the brain to smash into the skull. Inflammation and swelling inside the brain often damage nerves and prevent areas of the brain from receiving the oxygen and glucose it needs to perform. These effects of the injury disrupt the normal function of the brain.
Some of the most common sources of traumatic brain injuries are falls, motor vehicle accidents, assaults, and sporting injuries. Military service members have a fairly high rate of TBI. A TBI can even be a byproduct of a life-saving operation such as neurosurgery.
Sources of Non-Traumatic Brain Injuries
Non-traumatic brain injuries usually damage the brain by a lack of oxygen as a result of internal bleeding, clotting, or toxins, or as a result of pressure being placed on areas of the brain from a tumor. This results in damage or even death of brain tissue.
Common sources of non-traumatic brain injuries are stroke, aneurysm, and near-drowning.
Others that involve toxins include carbon monoxide poisoning, chemotherapy, and lead poisoning. Bacterial and viral infections (including COVID-19), meningitis and encephalitis, and similar conditions can also cause destructive inflammation.
Further reading:
Mild, Moderate, or Severe: Understanding How We Describe Brain Injuries
Traumatic brain injuries are usually categorized as mild, moderate, or severe. These terms don’t necessarily indicate the severity of what patients experience long-term as a result of a brain injury though. A “mild concussion” can still disable a person. Cognitive FX frequently treats patients who are unable to work or are homebound from their persistent concussion symptoms.
However, we can still explain how the medical community differentiates these brain injuries.
A mild traumatic brain injury is commonly called a concussion. Someone with an mTBI may or may not have lost consciousness, but if they did, it was for a very short time. (In fact, less than 10% of people with a concussion lose consciousness.) There is usually no bleeding in the brain and no skull fracture.
With a moderate traumatic brain injury, we might see a skull fracture, such as a fracture under the eye. There could be a visible sign of injury on the head. There might be a loss of consciousness with this injury (less than 24 hours in duration). Any bleeding is not life-threatening. A person with a moderate TBI might be kept under observation for a short time, but the injuries usually heal on their own. They don’t usually require surgery but may require follow-up at a neurology practice.
Someone with a severe traumatic brain injury must experience an extended loss of consciousness or even be in a coma. The skull may have a serious fracture, or some object might have penetrated it. Severe TBIs often require intensive care and emergency neurosurgery:
- A craniectomy removes a portion of the skull to relieve intracranial pressure on healthy areas of the brain due to bleeding or swelling in the brain.
- If there is a cerebrospinal fluid leak, surgery might be needed to install a shunt to drain the fluid or to repair the leak.
- Two types of bleeding within the brain after a TBI can be life-threatening: epidural hematomas and subdural hematomas. Occasionally, these bleeds are small and don’t cause swelling. In this case, they can be watched and might not require surgery. However, if the bleeding continues and causes swelling within or on the brain, emergency surgery is necessary. It is important to note that those 60 years of age and older have the highest death rate after experiencing a TBI. In this population, even a minor fall could cause lethal bleeding.
Again, just because an injury isn’t categorized as “severe” doesn’t mean it won’t have very serious and real consequences in your life.
What Are the Acute Signs of a Traumatic Brain Injury?

Sometimes it’s clear that someone has experienced a traumatic brain injury and needs to get to a hospital immediately. For example, if someone is bleeding and unconscious after a car accident or a fall from a ladder, we know to call emergency responders right away.
Very often, however, people are unsure. Depending on where you live and what medical coverage you have, visits to the emergency department are expensive; people don’t want to overreact. To make things even more confusing, sometimes a person seems fine right after an incident, but alarming symptoms develop over the next few hours or days.
While this list isn’t exhaustive, here are some guidelines to determine if someone might have a concussion or a moderate to severe traumatic brain injury. If you’re unsure about the severity of the injury, it’s best to get checked out by a medical professional.
Signs that it might be a concussion:
- Difficulty balancing or dizziness
- Headache
- Blurry vision
- Confusion about where they are or what day it is
- Slowness in thinking or acting
- Neck pain
- Ringing in the ears
- Sensitivity to light or sound.
In addition to any sign of a concussion, signs of a moderate or severe TBI are:
- Bleeding
- Alteration in consciousness
- Person becomes unresponsive
- Eyes aren’t tracking properly
- Pupils are dilated
- Convulsions or seizures
- Vomiting or nausea.
Traumatic Brain Injury in Children
The Brain Injury Association of America reports that brain injuries are the leading cause of death and disability in children and teenagers.
Children’s brains are different from adults. Sometimes their injuries aren’t immediately evident, and children can’t always verbalize what they’re experiencing.
Additional signs of TBI in children are:
- Nausea and vomiting
- Being unresponsive or losing consciousness
- Being excessively sleepy
- Trouble walking or problems with balance
- Weakness on one side of the body
- Slurring their speech
- Blood or a clear fluid draining from the ears or nose.
Unfortunately, the damaging effects of a brain injury on a child might not be evident until later in life, so it’s important to get a possible injury checked out and treated by a health care provider if there’s any question.
Note: If you’re suffering from persistent symptoms after head trauma, you’re not alone. Many of our patients struggle with headaches, word retrieval, feelings of overwhelm, and more before treatment. 95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. To learn if you’re eligible for our program, sign up for a consultation with our staff.
Symptoms and Long-Term Effects of Traumatic Brain Injury
Most people who sustain a concussion completely recover within a couple of weeks of their injury. A few, however, along with those who sustained a moderate or severe TBI, have to deal with a host of persistent symptoms indefinitely.
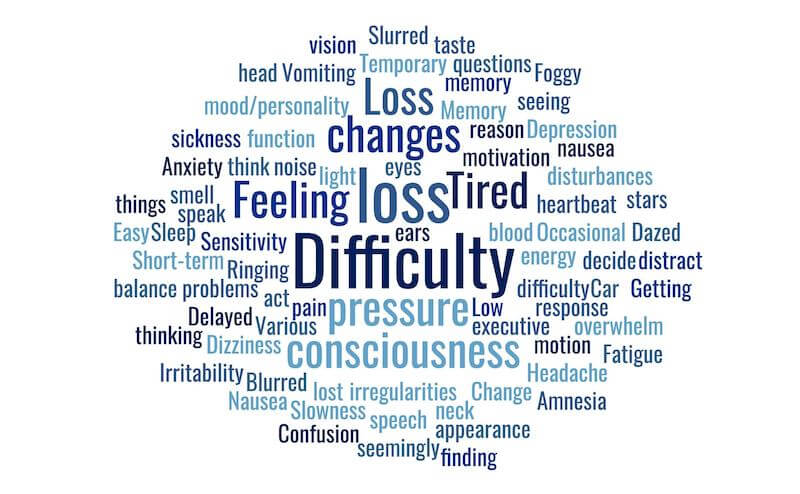
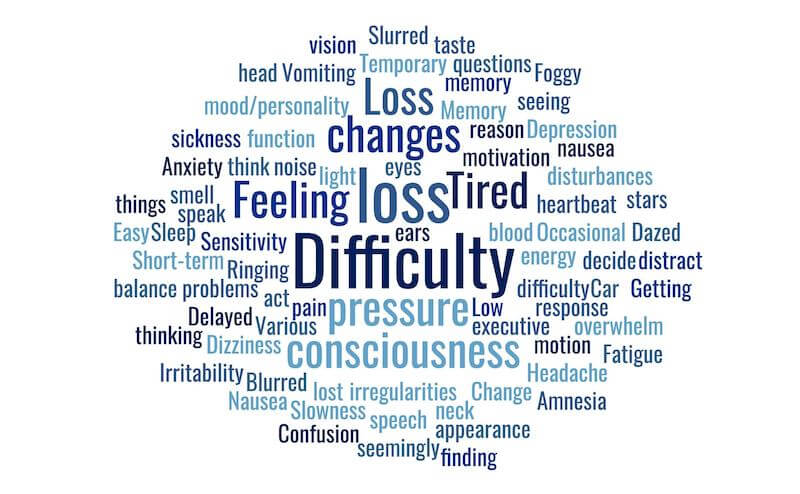
Whether you’ve suffered a mild, moderate, or severe TBI, many of these symptoms and long-term effects are the same. Of course, they vary in intensity from person to person. Some of them tend to appear immediately after an injury. Others sometimes develop later. Some symptoms might seem to come and go, triggered by certain environments or situations.
The chart below contains some of the most common long-term effects of TBI and when they frequently appear following a TBI.
|
Immediate or Early
|
Early or Delayed
|
- Amnesia (about the traumatic event)
|
|
- Brief loss of consciousness
|
|
|
|
- Car sickness or nausea with motion
|
|
|
- Change in (or loss of) taste or smell
|
- Delayed response to questions
|
|
- Dizziness or “seeing stars”
|
|
|
|
- Difficulty finding things
|
- Feeling of pressure in the head
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- Occasional heartbeat irregularities or changes in blood pressure
|
- Temporary loss of consciousness
|
|
|
|
|
|
|
|
| |
- Slowness to decide, think, speak, or act (difficulty with executive function)
|
| |
- Tired for seemingly no reason
|
| |
|
As you can see from these lists, TBI can cause physical symptoms and affect the nervous system in addition to cognitive function.
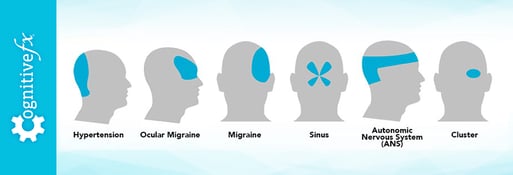
There are a couple of symptoms on this list that appear to vary depending on whether a patient has an mTBI or a severe TBI. Frequent headaches are very common in patients who had an mTBI, but less so among those who suffered a severe TBI.
Nevertheless, if you do suffer from frequent headaches, they can be debilitating. To help, we created an online course that covers which types of headaches you can get after a concussion, as well as specific techniques for coping with those types of headaches. If you want to learn how to manage your headaches at home, visit our course.
Also, it’s very common that someone who has a severe TBI continues to have amnesia about the injury itself. People who suffer a concussion often remember the injury immediately, or the memory eventually returns.
Emotional Problems After Traumatic Brain Injury
A range of mental health and emotional issues can affect those who have suffered a TBI. Anxiety and depression are common. Personality (mood) changes, mood swings, and difficulty controlling impulses can also be an issue.
The challenges associated with life after a TBI and the emotional and personality changes that sometimes go along with it can also contribute to relationship difficulties. Sometimes patients don’t feel like themselves anymore, and their partners can feel like they are involved with a completely different person.
The injury can cause roles in a partnership to change. A study by Virginia Commonwealth University investigated divorce rates following TBI and identified some important potential factors in separation and divorce. Some of the findings were not definitive; however, they did find that older people and those who had been married longer before the injury were less likely to divorce.
Another condition related to TBI worth mentioning is that sometimes an event that causes a TBI can also cause post-traumatic stress disorder. Common causes of PTSD are motor vehicle accidents, violent assault, and combat injuries, all of which are also common causes of TBI. It is possible to have both and need medical care for both.
Patients with behavioral changes and psychiatric disorders benefit from additional emotional support, patience, and encouragement as they pursue recovery.
Further reading: Support groups for brain injury patients and their family members
Lingering brain injury symptoms can range from frustrating to incapacitating. But they don’t have to be that way forever. To learn more about how we can help you recover, book a consultation.
What Causes the Long-Term Effects of TBI?
What causes some people to experience traumatic brain injury effects years after their injury?
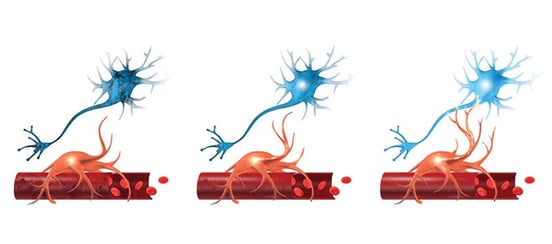
The key to that answer is understanding a process called neurovascular coupling and what happens when it malfunctions.
Neurovascular Coupling: The Brain’s Communication System
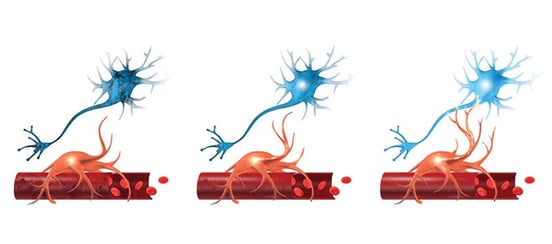 Neurovascular coupling is the communication system between brain cells (neurons) and blood vessels. Neurons are the cells that carry messages back and forth between the brain and the body. Glucose and oxygen are the fuel the brain needs to operate, and they are carried through the blood vessels.
Neurovascular coupling is the communication system between brain cells (neurons) and blood vessels. Neurons are the cells that carry messages back and forth between the brain and the body. Glucose and oxygen are the fuel the brain needs to operate, and they are carried through the blood vessels.
When the body has a demand, the brain anticipates the need for the right amount of fuel at the right time to fulfill that demand. When the demand in an area increases, the brain calls for more fuel. This causes the brain to direct more glucose and oxygen to that area.
For example, as soon as you think you need to read something, your brain anticipates how much fuel it needs and where it needs it to allow you to complete this task of reading — even before you begin to read! The brain needs to be ready at the precise moment that you begin to read. It sets this all up through neurovascular coupling.
Neurovascular Coupling Dysfunction
An injury to the brain sometimes damages neuronal connections. Inflammation and swelling in response to the injury can diminish the amount of blood traveling to or through those injured areas. This disrupts the established neurovascular coupling pathways (without resulting in cell death).
The brain still tries to deliver fuel to where it’s needed, but if its normal route is blocked, it forms new routes around the damaged area. This detour, unfortunately, isn’t as efficient as the original pathway.
Usually after a TBI, the brain suppresses blood flow to injured areas, which means those areas aren’t getting enough blood when they need it. As a result, these brain regions are hypoactive (underperforming). Other areas of the brain may try to compensate, but taking on extra tasks wears them out more quickly. TBI symptoms are the consequence of this dysfunction.
When people recover from a brain injury, those pathways will either return to normal or continue malfunctioning. If they fail to revert to healthier signaling after the trauma of the acute injury subsides, the result is long-term dysfunction of neurovascular coupling and thus long-term symptoms of TBI.
The good news is that dysfunctional neurovascular coupling is detectable and treatable with the right diagnostic tools and therapy. We’ll explain that later in this article.
Other Causes of Long-Term Traumatic Brain Injury Symptoms
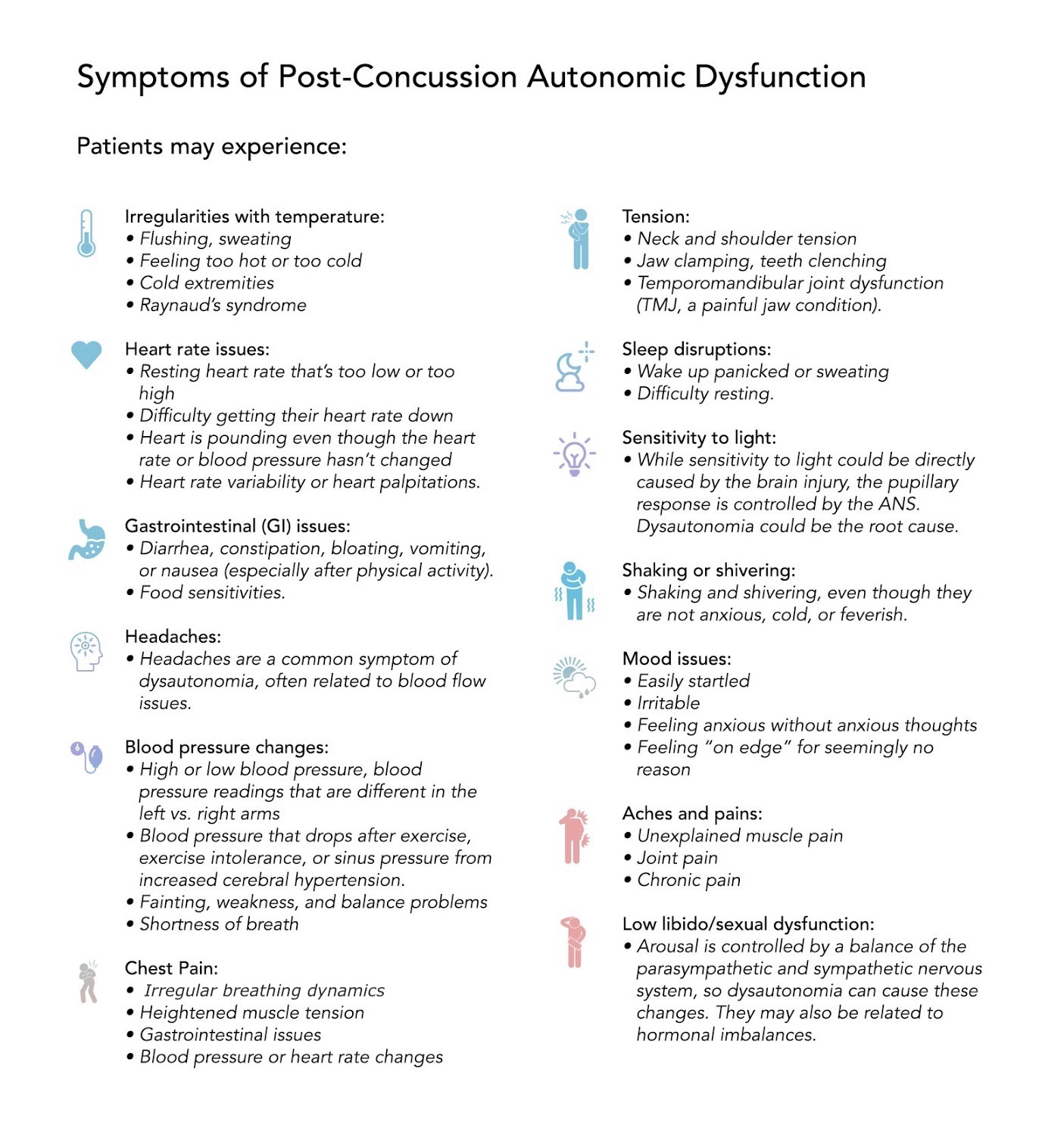
A traumatic brain injury can result in hormonal changes, autonomic nervous system dysfunction, vestibular dysfunction, and vision problems. Here’s a quick look at each.
Hormone Dysfunction: The pituitary gland dangles from a thin stalk in your brain. It is easily damaged during a brain injury. If twisting or shearing of the nerves occurs — or if neurovascular coupling affects the pituitary gland, hypothalamus, or other regions involving hormone regulation — then you might experience changes in growth hormone, thyroid, cortisol, or sex hormone levels. In turn, those changes can produce symptoms throughout the body. A good endocrinologist can test your hormone levels and provide treatment while taking your history of TBI into account.
Further reading: Hormone dysfunction after a traumatic brain injury
Autonomic nervous system dysfunction (dysautonomia): The autonomic nervous system (ANS) influences nearly every organ in your body. It communicates closely with the brain and with local body systems to keep everything running smoothly, whether you’re settling in for a meal or running a marathon. Normally, the main two parts of the ANS — the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) — dynamically balance each other throughout the day. But in TBI patients, the SNS, which controls the “fight or flight” response, often becomes dominant. Patients can experience a host of cognitive impairments and physical symptoms as a consequence.
Further reading: Dysautonomia after a head injury
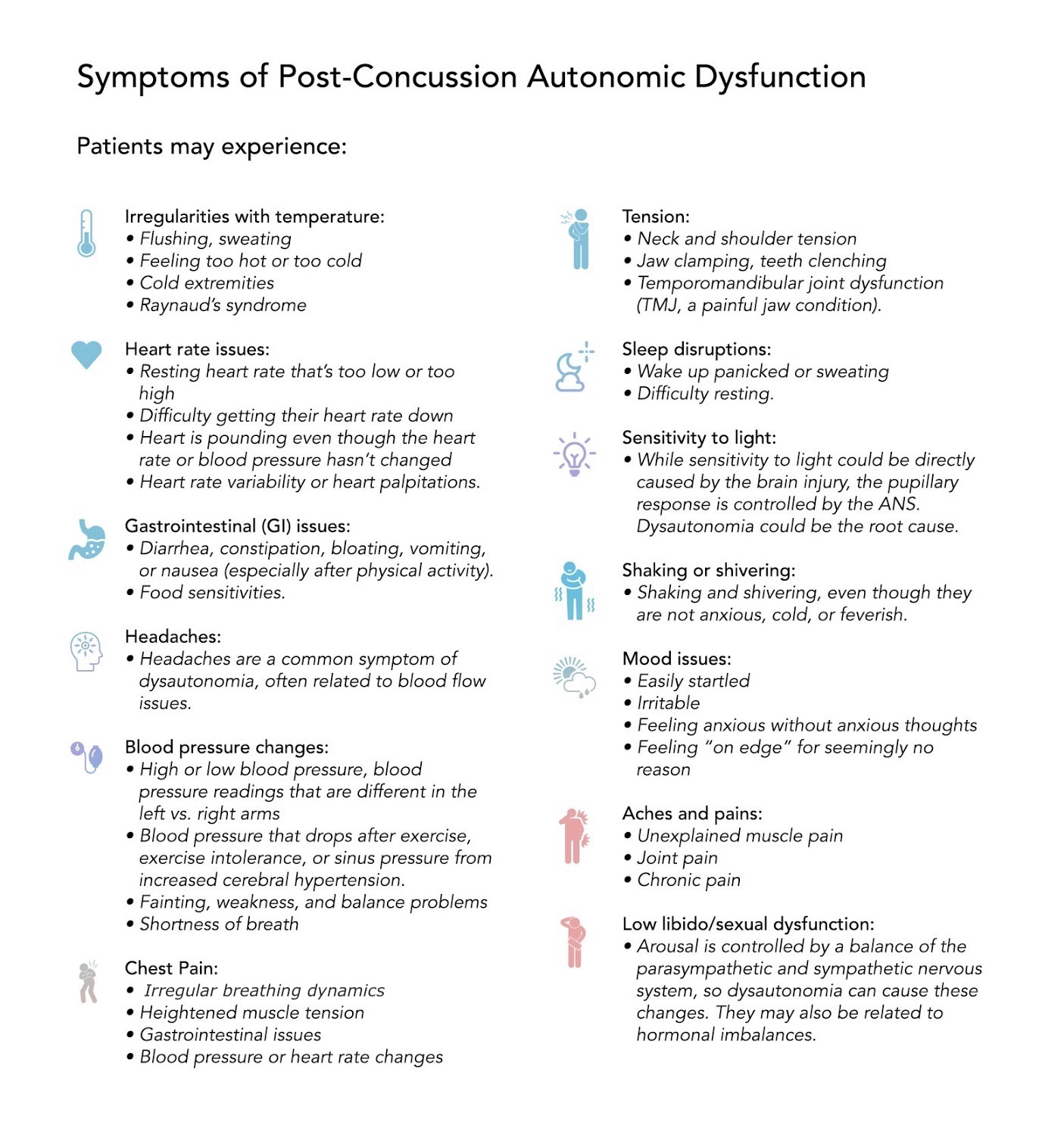
Vision problems: The communication between your eyes and your brain, along with neurovascular coupling in the regions that process visual information, can be disrupted after a brain injury. You might experience changes in your peripheral vision (seeing too much or too little), eye teaming (how the eyes work together), depth perception, focusing, and more. These changes can then cause symptoms such as headaches, tired eyes, double vision, difficulty reading, and more.
Further reading: Vision problems and therapy after a head injury
Vestibular dysfunction: The vestibular system, an organ located in your inner ears, works with your vision, body, and brain to determine your position in space, keep you balanced, and help your vision stay clear when you move. After a concussion, communication between some or all of those systems could be affected. Vestibular dysfunction can produce symptoms such as headache, dizziness or vertigo, difficulty balancing, sleep problems, spatial disorientation, and more.
Further reading: Vestibular therapy after TBI
Diagnosing a Traumatic Brain Injury
Of the approximately 2.8 million TBIs that occur in the U.S. every year, the majority are diagnosed as concussions.
Currently, there is no definitive test to diagnose a concussion with 100% accuracy. A concussion is generally diagnosed by observing the injured person for typical symptoms and by evaluating their reactions and responses.
In sports, a variety of protocols have been implemented to try to detect a possible concussion in athletes. Some athletes are required to take a pre-season baseline test so that before- and after-injury health information can be compared if necessary. Some use the Balance Error Scoring System because balance problems after an injury are indicative of a concussion. Others use standard guidelines such as the Concussion Recognition Tool 5 or one of the Sport Concussion Assessment Tools, which vary according to the age of the athlete.
If symptoms or circumstances indicate the possibility of a moderate to severe TBI, a trip to the emergency room is necessary to look for life-threatening bleeding, swelling, and fractures.
Imaging for TBI Diagnosis

The two most common types of imaging tests used to diagnose a brain injury are magnetic resonance imaging (MRI) and computerized tomography (CT). If severe injuries are not suspected, it’s often best to wait on neuroimaging to see how the patient progresses.
An MRI uses magnets and radio waves to look at soft tissue within the brain and the body. It is best used for detecting bruises (contusions), blood clots (hematoma), minor bleeding, tumors, excessive fluid, or even signs of dementia in the brain. It is not the best scan to start with immediately after a severe head injury. It might be done after the patient is more stable.
A CT scan (computed tomography scan) uses X-ray beams and, if performed after a head injury, can detect bleeding (hemorrhage), brain swelling, and skull fractures. In an emergency, a CT scan is most commonly ordered to determine if a patient needs to be watched or if emergency neurosurgery is necessary.
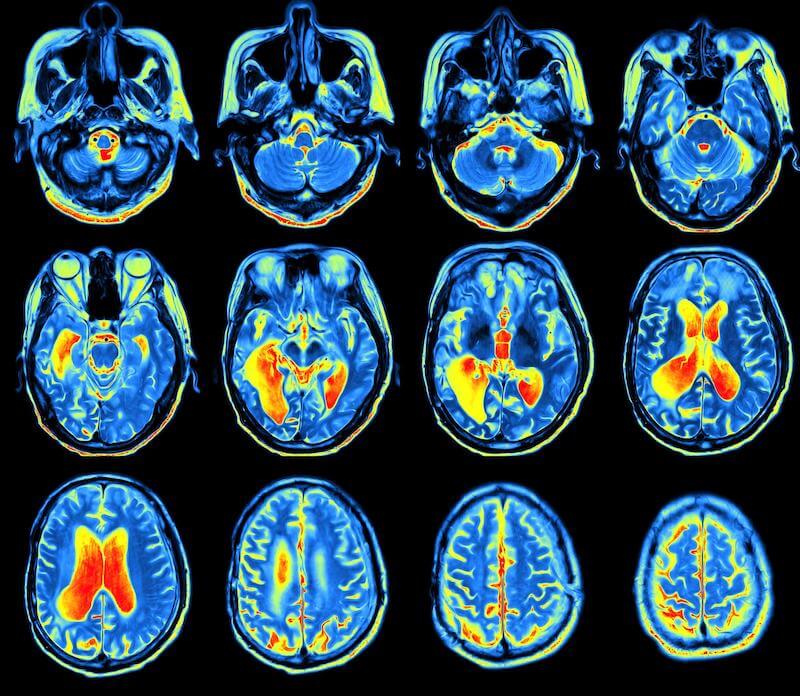
Neither a standard MRI nor a CT scan can detect a concussion because they only detect structural problems within the brain. A concussion does not cause this type of problem. As we discussed earlier, a concussion damages the neurovascular coupling system within the brain. This type of dysfunction can be seen with functional MRI (fMRI), which shows how blood flows through the brain in real time.
Further reading:
‘Seeing’ Neurovascular Coupling Dysfunction with fNCI Scans
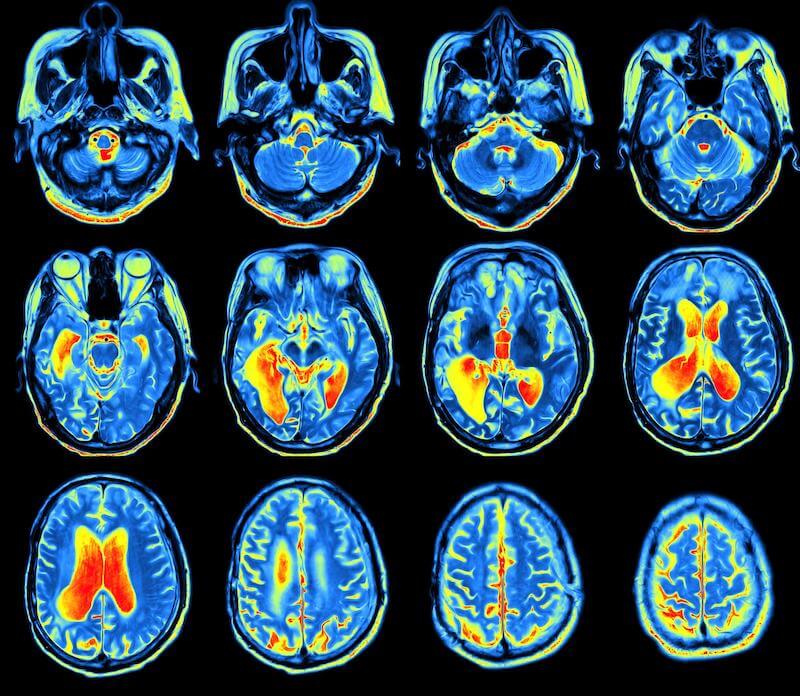
An fMRI is a type of MRI that can map brain activity by seeing and measuring the amount of blood flow to areas of the brain in response to cognitive activity.
We developed a special use of fMRI called functional neurocognitive imaging (fNCI) to take real-time images of the brain while a patient performs a series of cognitive tasks. We’ve done intensive studies to develop a reliable database of images from people who have never had a brain injury and who do not have any post-concussion symptoms performing these same tasks. We can then compare patients’ images with that database to determine if any areas of the brain are experiencing neurovascular coupling dysfunction.
We know which areas of the brain should activate during a specific task and how much blood flow should be going to that region. Through the fNCI scans, we can easily identify areas that aren’t using resources the way they ought. That tells us exactly which areas of the brain are injured and how they are injured, which allows us to tailor treatment to each patient’s specific injury.
Traumatic Brain Injury Treatment
Treatment for brain injury varies depending on the severity of the injury and its consequences. The more severe the injury is, the less chance the patient has of returning to their full, pre-injury abilities.
According to the American Association of Neurological Surgeons, approximately 60% of those with a moderate traumatic head injury fully recover with minimal lingering symptoms. However, of those with a severe TBI, the statistics are more grim: Thirty-three percent do not survive, another 33% have moderate to severe disability, and approximately 25%-33% recover to a functional degree.
It’s important to note that even if a patient doesn’t recover full functionality, a lot of progress can be made through rehabilitation.
Factors That Make Recovery More Difficult
That said, there are a few situations that make recovery more challenging.
One is if part of the brain has been removed. Sometimes this is done to remove a tumor or to control seizures (epilepsy is another possible consequence of TBI). In this situation, other parts of the brain might learn to compensate, doing at least some of the work that the removed part used to do.
Another is when parts of the brain atrophied from lack of oxygen due to swelling.
Finally, if a more central part of the brain is injured, it’s harder to recover because those areas of the brain have more control over the body’s ability to survive and function.
Author’s note: At the same time, I’ve seen miracles happen with moderate and severe brain injuries. Years ago, my husband at the time was T-boned by a drunk driver and life-flighted to a nearby hospital. He was in a coma for two weeks. He had to have part of his skull removed because of swelling and part of his temporal lobe removed as well. Now, he’s back in the workforce. Aside from a visible scar, people who interact with him briefly wouldn’t even know that he had a severe TBI.
Rehabilitation for TBI

Rehabilitation for a severe TBI usually begins in either an inpatient or an outpatient rehabilitation facility. Facilities that specialize in activities of daily living (ADL) rehab help patients relearn how to walk, feed themselves, and bathe and dress themselves. Types of rehabilitation can include physical therapy, speech therapy, cognitive therapy, and psychological care.
The brain can compensate for injuries in the frontal, occipital, or temporal lobes. It can be retaught how to perform these daily activities, sometimes in an alternative way, so the patient can function as independently as possible. Many patients can and do live a full life after a TBI.
The timeline for the possibility of recovery after an injury has changed over time. Neurologists used to think that most recovery would take place within three months of the injury. Later, that timeline was extended to six months, with some additional recovery being thought possible up to a year after the injury.
Now, as we learn more about neuroplasticity in the brain, there is more disagreement among medical professionals about the window for recovery. At Cognitive FX, we believe people can continue to improve indefinitely. We’ve seen so many patients improve beyond their expectations, even years after their injury. (You can read about some of them at the end of this article.)
Further reading: How to help someone with TBI (and avoid caregiver burnout)
Further Therapy for TBI: Treatment at Cognitive FX

Therapy for basic life skills is critical, but patients who have completed their ADL rehabilitation (or who didn’t need it in the first place) may still want to improve further. Many are struggling with long-term consequences of TBI that interfere with their daily lives.
Sometimes, they hear about the success other patients have had in overcoming post-concussion syndrome at our clinic. When they contact us, they almost always ask if they’ll see the results that concussion patients see. They want to know, “Will it work for me?”
The answer is yes, with some caveats.
To be honest, a brain that has suffered a severe TBI has more challenges than one that’s suffered an mTBI. We can’t expect as much recovery as our typical PCS patients see, nor is it likely to happen as quickly.
Author’s note: Most people don’t know that I spent the early years of my career as a neuropsychologist treating patients with severe TBIs. During that time, I realized a huge percentage of people who suffered a mild TBI were being ignored or underserved. Because they were able to perform most activities of daily living, they were told they were “fine” despite continuing to suffer from persistent symptoms. So, we adapted the therapies I had been using to treat patients with severe TBI to treat the post-concussion population. They’re still effective regardless of the severity of brain injury you’ve experienced.
In-house treatment at Cognitive FX typically lasts one week for someone who has had an mTBI. It often takes two weeks of treatment for someone who has had a severe TBI. It’s just harder for the brain to handle intense therapy after a TBI. We also advise TBI patients to come back for some follow-up “booster days.”

Even knowing that, many patients tell us that even if they only see a 5% improvement, it would be life-changing and worth it (that said, we typically see greater improvement than 5%!). Even small progress can make a significant impact on your quality of life.
There are some basic requirements necessary to be able to complete our treatment. Patients must have:
- The cognitive ability of an average 3rd grader (so they can complete the cognitive tasks during the fNCI scan)
- Enough mobility to do some kind of aerobic exercise, such as riding a stationary bike (aerobic activity is a vital part of our therapy process).
EPIC Treatment

Enhanced Performance in Cognition (EPIC) Treatment is our unique therapy program that corrects neurovascular coupling dysfunction and restores normal blood flow to the areas of the brain that are not working correctly. We also work to correct autonomic nervous system dysfunction, vestibular dysfunction, and vision changes, though some of these require additional therapy over a longer period of time to fully resolve.
The first day of treatment starts with three MRIs:
- First, we do a standard structural brain MRI to rule out any underlying problems that need to be addressed before moving forward with treatment. Examples of things we sometimes find are brain tumors; evidence of stroke; cerebral atrophy; and Multiple Sclerosis. Sometimes we find issues that need immediate attention. Others don’t prevent treatment, but they need follow-up by local medical specialists.
- Next, we do a cervical spine MRI to look for anything that could interfere with treatment or that needs to be addressed. Sometimes the injury that caused the TBI also damaged the neck, or patients have unknown pre-existing conditions that we need to be aware of. Examples of things we sometimes find are degenerative disc disease; spinal stenosis (the narrowing of the spinal cord openings that house nerves); and other degenerative conditions that need to be checked out. We’re looking for anything that could cause therapists to avoid or alter certain treatments they normally provide.
- Finally, we do the fNCI to pinpoint specific areas of dysfunction in the brain. We use that information to inform each patient’s treatment plan.
Our therapists work together to deliver individualized treatments that will be effective for each person’s specific areas of injury. Some of the therapies included in our program for traumatic brain injury treatment include:

We also teach patients how to continue these exercises at home after their treatment week. Each patient is sent home with a personal aftercare plan.
The last step of the EPIC Treatment process is a follow-up fNCI. We take the results of this scan and compare it to the scan done earlier in the week to see how much each area has improved. 95% of our patients show statistically verified restoration of brain function. Post-concussion patients show, on average, 77.5% improvement in their scans after just one week. Long-term follow-ups we’ve conducted showed that these improvements held, and in many cases, continued to progress.
In addition, there is now third-party peer-reviewed research (the first of its kind) specifically evaluating and validating these results. A study in the Netherlands found that Cognitive FX treatment led to meaningful symptom reduction in post-concussion symptoms for 77% of study participants.
Recovering from Traumatic Brain Injury

Each brain injury is unique. Each recovery will be too. There is no set timeline that every injury follows. Not every patient sees 100% recovery, but it’s important to keep looking for help because you never know how much more you could recover.
Cognitive FX is open to seeing anyone who has suffered any kind of brain injury causing long-lasting symptoms, whether it’s from an accident or traumatic injury, or something like neurosurgery complications or neurotoxicity. We’ve successfully treated patients whose injury happened years ago. If you’re not happy with where you are in your recovery, don’t give up hope.
Further reading: Five brain injury recovery stories
We’d like to introduce you to a few of our patients who suffered moderate to severe TBIs and who came to us for treatment:
Michael Ray came to Cognitive FX three years after a severe stroke left him unable to walk or talk. Michael’s fNCI at the end of the week showed a noticeable improvement in blood flow to damaged areas of his brain.
Aimee was in a car accident that resulted in a severe TBI. She had constant headaches, personality changes, memory problems, exercise intolerance, and narcolepsy after the accident. She came to Cognitive FX seventeen years after that accident. After treatment, her memory improved, she was able to multitask again, and her headaches are less severe and much less frequent. She’s been able to dramatically reduce the medication she takes for narcolepsy.
Samuel Gray found Cognitive FX 33 years after childhood neurotrauma. Sam suffered from many typical long-term TBI symptoms. He began to see improvement mid-week during his treatment week and went on to become more successful at work than he ever expected.
Jamie Crane Mauzy was a professional skier who suffered a severe TBI during a competition. She was in a coma for eight days. Jamie came to Cognitive FX four years after her accident. After one week of treatment, Jamie found she was able to recall words and follow conversations again.
If you’re suffering from persistent symptoms after brain trauma, you’re not alone. Many of our patients struggle with headaches, word retrieval, feelings of overwhelm, and more before treatment. 95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. To learn if you’re eligible for our program, sign up for a consultation with our staff.


 Neurovascular coupling is the communication system between brain cells (neurons) and blood vessels. Neurons are the cells that carry messages back and forth between the brain and the body. Glucose and oxygen are the fuel the brain needs to operate, and they are carried through the blood vessels.
Neurovascular coupling is the communication system between brain cells (neurons) and blood vessels. Neurons are the cells that carry messages back and forth between the brain and the body. Glucose and oxygen are the fuel the brain needs to operate, and they are carried through the blood vessels.