Many hospitals offer robust medical treatment to help patients survive traumatic brain injuries (TBIs). It’s common for those same hospitals, or affiliated care providers, to offer rehabilitation to patients after the danger of death has passed. These rehabilitation services often focus on activities of daily living (walking, dressing yourself, eating, etc.). It’s less common to find appropriate rehabilitative medical care for long-lasting symptoms following TBI.
Dealing with these long-term effects can be overwhelming and hard to understand, in part because TBIs range considerably in severity. Some patients may be told their brain damage means they’re unlikely to walk again, while others may be told to expect occasional migraines that interfere with work. Some patients function almost like they did pre-injury; others struggle to feed and clothe themselves.
No matter how severe or mild your symptoms, there is hope for improvement. The human brain is flexible and can adapt to your post-injury situation. It does this by using nerve cells that are still healthy after brain injury and developing new communication pathways which try to compensate for injured pathways. The problem is that this mechanism — called neuroplasticity — doesn’t always result in the most effective connections by itself. Sometimes, it requires guidance.
Various therapies — such as cognitive therapy, physical therapy, vision therapy, and others — encourage the brain to recover lost functions via neuroplasticity.
With access to the right therapy, patients can recover from long-term symptoms caused by a traumatic brain injury (or at least experience significant symptom improvement). Patients with severe TBIs face a longer recovery process than those with milder injuries and may never recover fully, but they can still make life-changing progress.
At our clinic, Cognitive FX, we specialize in helping brain injury patients recover from persistent symptoms. Some of our patients have been dealing with their symptoms since childhood. And many were told by their doctors that once their improvement plateaued, they wouldn’t be able to recover further. But we routinely see brain injury recovery that defies expectations. Our patients are fighters and experience real improvement. So can you! Recovering from a TBI doesn’t come with a time limit; it’s never too late to keep getting better.
In this article, we explain…
Over 90% of our patients experience symptom improvement after just one week at our clinic. To see if you are eligible for treatment, sign up for a consultation.
Traumatic Brain Injuries Cause Persistent Symptoms
.jpg?width=1999&height=1333&name=Vision%20Problems%20After%20COVID%20Causes%20and%20Treatment%20(1).jpg)
A Cognitive FX therapist demonstrates sensorimotor therapy.
Traumatic brain injuries (including those classified as “mild”) can lead to a lifetime of physical, cognitive, emotional, and behavioral symptoms. The most common issues include the following:
Direct injury to the brain (stretched or severed nerves, destroyed brain tissue, etc.) obviously causes symptoms. But there are many other ways that brain injuries can result in symptoms. Providers need to be able to assess how an injury is contributing to the patient’s symptom burden, then provide treatment accordingly.
Here are some of the most common culprits that show up regardless of the causes of TBI:
Neurovascular Coupling Dysfunction
Brain injuries can cause damage to the connections between neurons. The brain responds with inflammation and swelling, but this often restricts the amount of blood circulating through those injured areas.
Brain cells rely on an extensive network of blood vessels to bring them the resources needed (oxygen and nutrients) to function normally. If the demand increases to complete a particular task, brain cells call for more nutrients, and blood vessels deliver what’s needed. The call-and-response relationship between neurons and the blood vessels that supply them is called neurovascular coupling.
TBIs disrupt this mechanism in affected parts of the brain. The brain still tries to deliver resources where and when they’re needed, but if the main route is blocked, it will try to find an alternative way. This detour, however, isn’t as efficient as the original pathway.
As long as the brain fails to revert to a healthier relationship between nerve cells and blood vessels, the result is long-term neurovascular coupling dysfunction, which inevitably leads to long-term symptoms of TBI.
Further reading: Why CT scans don’t show neurovascular coupling dysfunction
Hormone Dysfunction
The pituitary gland is often called the "master" gland of the endocrine system, as it controls the secretion of a variety of hormones. Due to its thin structure connecting it to the hypothalamus, the pituitary gland is easily damaged during a brain injury. Twisting or bending — affecting blood flow to this area — can affect the levels of multiple hormones, such as growth hormone, thyroid, cortisol, and sex hormones. In turn, these changes produce symptoms throughout the body, such as low blood pressure, fatigue, weight gain, low libido, amenorrhea, heart palpitations, hair loss, and more.
Further reading: Hormone dysfunction following head injury
Dysfunction of the Autonomic Nervous System (ANS)
.jpg?width=552&height=349&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(3).jpg)
The ANS controls many different functions in the body, including blood pressure, breathing rates, and heart rate. Under normal conditions, the two main parts of the ANS — the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) — work together in harmony. The SNS (which you can think of as the fight-or-flight branch of the nervous system) prepares the body for stressful or emergency situations by increasing blood pressure and breathing rates. In contrast, the PNS (rest-and-digest) slows heart rate, lowers blood pressure, and stimulates the digestive tract.
However, in TBI patients, the SNS often becomes dominant. As a result, patients can experience a host of concussing symptoms, such as irregular breathing and sensitivity to light.
Further reading: Guide to Post-Concussion Autonomic Dysfunction (Dysautonomia)
Vision Problems
Vision problems are common after a traumatic brain injury. Brain injuries not only affect the way your brain and eyes communicate with each other, but they can also disrupt neurovascular coupling in the regions of the brain that process visual information. As a consequence, patients may experience deficits or changes in peripheral vision, eye teaming (how the eyes work together), depth perception, and focusing. These issues can cause headaches, tired eyes, double vision, difficulty reading, and more.
Further reading: Vision problems after head injury
Vestibular Dysfunction
The vestibular system — located in your inner ears — works in combination with your eyes, body, and brain to determine your position in space, maintain your balance, and help your vision remain stable when you move. After a traumatic brain injury, the connection between some or all of those components can be affected. Problems with the vestibular system can lead to various symptoms such as headache, dizziness or vertigo, difficulty balancing, sleep problems, spatial disorientation, and more.
Further reading: Why vestibular therapy helps brain injury patients
Recovering From a Traumatic Brain Injury
.jpg?width=1333&height=1816&name=Physical%20therapy%20covid%20(2).jpg)
Patients with a traumatic brain injury need specialized medical care and rehabilitation. The aim of rehabilitation programs is to improve the overall quality of life for TBI patients and reduce the chances of developing long-term, permanent disabilities.
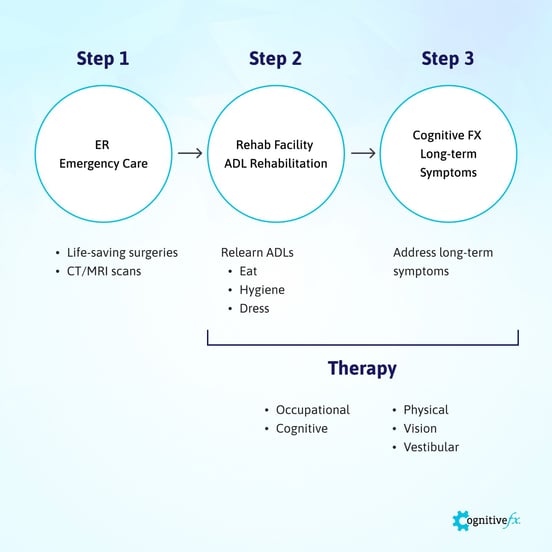
Immediately after the injury, patients need emergency care, most likely in an ER or an urgent care clinic. Patients with these injuries may need surgical interventions to treat bleeding in the brain, a blood clot, or a skull fracture. (This initial treatment is not part of the scope of this article.)
Once the patient is stable, the hospital may recommend inpatient or outpatient brain injury rehabilitation programs, depending on the severity of the injury. The aim at this stage is to use therapy to help patients recover function to be able to live independently. Healthcare providers such as nursing staff, therapists, physical medicine practitioners, and others focus on helping patients practice activities of daily living (ADLs), such as eating, dressing, and personal hygiene.
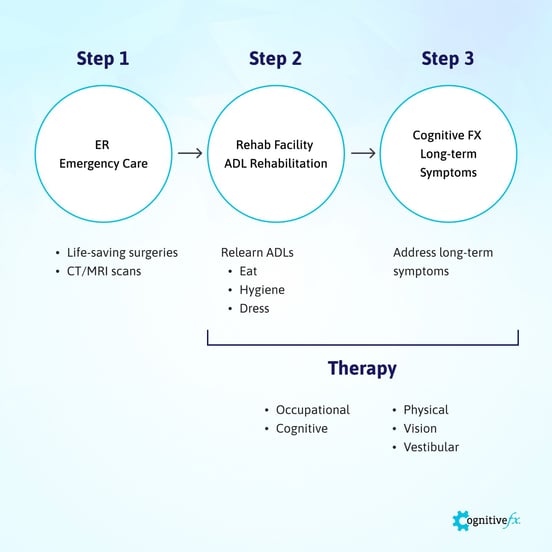
After patients complete their ADL rehabilitation, the next step involves addressing long-term symptoms that interfere with their daily lives. This is where Cognitive FX can be of assistance. Our team uses multidisciplinary therapies to create a tailor-made treatment for each patient (more on that later).
Over 90% of our patients experience symptom improvement after just one week at our clinic. To see if you are eligible for treatment, sign up for a consultation.
Note: Pediatric rehabilitation looks a little different than adult rehab. To learn more, see our post on children’s recovery from persistent TBI symptoms.
Therapy for Traumatic Brain Injuries
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(5).jpg)
Traumatic brain injuries can be treated with psychiatric care, physical therapy, occupational therapy, speech therapy, social support, and more. Over time, therapy needs to change as the patients’ needs and abilities change. At first, patients may need more physical and occupational therapy to be able to cope with daily activities. They may then move to vision or vestibular therapy, for example, to deal with lingering symptoms.
Recovery programs may include one or more of these therapies from trained health professionals:
- Physical therapy
- Occupational therapy
- Cognitive therapy
- Speech and language therapy
- Vision therapy
- Vestibular therapy
- Psychiatric and psychological care
Physical Therapy
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(2).jpg)
Brain injuries can affect parts of the brain that involve motor coordination, sensory processing, and other movement-related communication. In addition, patients may have restricted movement during recovery, leading to stiff, atrophied muscles.
Physical therapists teach patients techniques and exercises to relearn how to use their muscles and regain movement. Therapists can help patients rebuild cardiovascular endurance and lead them through exercises to promote posture, balance, flexibility, body awareness, and more. If needed, therapists can also teach you to use assistive or adaptive devices, such as prosthetics, wheelchairs, or walkers.
Physical therapy also has a significant impact on brain function and TBI recovery.
Read more on how physical therapy helps after a traumatic brain injury.
Occupational Therapy
Occupational therapists help patients relearn how to perform daily tasks in order to maintain independence. This can be anything from basic skills, such as eating and getting dressed, to more advanced tasks, such as driving or keeping track of finances. Occupational therapists may also advise changes around the home to ensure the patient’s safety and well-being.
Below are some practical ways in which an occupational therapist can help a patient after a traumatic brain injury:
- Implement strategies to help with memory, such as to-do lists and reminders.
- Plan a daily routine for the patient.
- Support the patient’s return to work or school.
- Support the patient’s return to social activities, sports, and hobbies.
- Help the patient follow healthy sleep patterns.
- Suggest home modifications or equipment purchases based on patient needs, such as wheelchairs, specialty beds, or stair lifts.
- Educate and support caregivers and family members.
Cognitive Rehabilitation Therapy
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(7).jpg)
Depending on which part of the brain is injured — and to what extent — patients may experience cognitive impairments, such as memory problems, difficulty concentrating, or poor decision-making skills. These symptoms can severely lower quality of life and increase withdrawal from social life.
Ideally, cognitive rehabilitation therapy can start when someone with a brain injury is admitted to the hospital. Therapists start by assessing level of alertness, orientation to surroundings, and memory of recent events, which in turn will be used to suggest the best course of action for these patients.
For example, activities for patients with a moderate degree of cognitive impairment may include group therapy oriented to being active in the community or going back to work/school. For more severe cases, patients may need individual therapy addressing cognitive issues like loss of short-term memory or difficulty following directions.
As the patient improves, cognitive therapy can be used to further the brain’s recovery from injury.
Read more about cognitive therapy for brain injury.
Speech and Language Therapy
A speech and language therapist helps patients improve their communication skills. This may include understanding and expressing both written and spoken language, as well as improving the clarity of speech. They also assess the patient’s language skills, such as memory, attention, concentration, calculation, problem-solving, reasoning, and judgment.
Speech therapists can assess whether the patient is experiencing swallowing difficulties and recommend the use of communication aids, especially after a severe injury.
Further reading: How speech therapy helps TBI patients
Vision Therapy
.jpg?width=1999&height=1333&name=Why%20Most%20Post-Trauma%20Vision%20Syndrome%20Treatment%20Falls%20Short%20(3).jpg)
Multiple studies show that vision therapy — also called neuro-optometric rehabilitation — can help patients improve their vision skills after a traumatic brain injury. This therapy covers many different areas, such as improving visual tracking, depth perception, accommodation, and peripheral vision, among others.
Each program should be tailored to the patient’s specific needs. It’s important to note that patients often need vision therapy for several months, as progress can be slow.
Further reading: Symptoms and treatment for vision issues after head injury
Vestibular Therapy
A therapist specializing in vestibular symptoms can evaluate balance problems and dizziness and develop a treatment plan to address these issues. This assessment includes asking patients to move their heads to different positions to determine what triggers symptoms, examining eye movements, assessing the ability to focus on a specific target while moving, and checking balance.
Effective therapy strategies often include repositioning techniques, gaze stabilization exercises, and binocular vision training. Dizziness and balance problems can increase the risk of falling, potentially causing a second brain injury, so it’s important to use strategies to lower the risk.
Further reading: Vestibular therapy for TBI symptoms
Psychotherapy
Traumatic brain injuries can cause a great deal of emotional distress, especially for patients with a severe condition or struggling with long-term symptoms that affect their quality of life. Depression, anxiety, and post-traumatic stress are frequent in TBI patients, as are apathy, aggression, impulsivity, and other behavioral changes.
Psychotherapy, conducted by neuropsychologists or neuropsychiatrists, is a form of therapy designed to assess and treat behavioral, emotional, and cognitive problems after a TBI. These therapists often also advise family members on how to provide emotional support and may offer referrals to support groups.
Further reading: Mental health considerations after TBI
How Much Therapy Do You Need?
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(8).jpg)
How much and what type of therapy you need depends on many factors, such as how persistent your symptoms are, which type of symptoms you have, how severely your brain was damaged by the injury, and more.
As a general rule, patients who experienced prolonged loss of consciousness or were in a vegetative state after head trauma often need more specialized medical care. In contrast, patients with a mild traumatic brain injury (mTBI) — commonly known as a concussion — often recover fully within a few weeks, with or without therapy. About a third of mild TBI patients, however, continue to experience symptoms for months or even years after the concussion. This condition is called post-concussion syndrome (PCS), and it can be debilitating. These patients need therapy to address their lingering symptoms.
The good news is that patients can continue to recover indefinitely. In the past, doctors assumed that healing could only occur during the first two years after an injury, and after that, the brain was incapable of changing. However, we now know that is not correct. Severe traumatic brain injury patients continue to improve long after the two-year mark.
At Cognitive FX, we’ve seen many patients who made tremendous progress decades after their initial injury!
Multidisciplinary Therapy Programs Get the Best Results
%20(5).jpg?width=552&height=368&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(5).jpg)
Often, patients see only one or two therapists at a time, which limits the benefit they can receive from treatment. Physical therapy by itself is helpful, but it’s more powerful combined with cognitive and sensorimotor therapy, for example.
At Cognitive FX, we offer a multidisciplinary approach which combines treatment modalities from different types of therapy for greater effect on recovery.
Our treatment program — called Enhanced Performance in Cognition (EPIC) — tackles the underlying brain dysfunction, autonomic dysfunction, vision, and vestibular issues experienced by each patient and resolves or improves many symptoms at the same time. Our treatment can be used for all forms of traumatic brain injuries, though the length and type of treatment can vary based on the particular injury.
Two keys to our treatment success are the advanced brain imaging protocols we use to more accurately diagnose patients and the way that we combine cardio with multidisciplinary therapies. We explain more about both below.
We conduct research at our clinic and have numerous published papers with our findings. Our treatment program is based on our research and the findings of other research teams throughout the world. You can view our publications here.
What to Expect at Cognitive FX
.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(7).jpg)
If you are approved for treatment at our clinic, your time with us begins with a thorough evaluation, including a review of your medical history, an assessment of your symptoms, and a series of physical exams.
You’ll also undergo a brain imaging scan to determine exactly how the injury affected your brain. The scan — called functional Neurocognitive Imaging (fNCI) — is a type of functional MRI. It can identify which regions in the brain are suffering from neurovascular coupling dysfunction. It looks at blood flow dynamics in 56 areas of the brain, as well as at how well these areas communicate with each other.
-1.jpg?width=552&height=303&name=Physical%20therapy%20covid%20(3)-1.jpg)
We also perform regular MRI scans of the cervical spinal cord and the brain to understand any physical damage caused by your injury. If we find issues that need to be resolved before therapy continues, we will refer you to neurosurgery experts or another neurotrauma specialist.
Once the initial evaluation and brain scan are completed, our team designs your custom-made treatment plan. You will receive, in combination or in quick succession, the following types of therapy:
- Physical therapy
- Vision therapy
- Neuromuscular therapy
- Occupational therapy
- Vestibular therapy
- Cognitive therapy
- Sensorimotor therapy
- Neurointegration therapy
- Psychotherapy
- And more
Each day of treatment begins with physical exercise. You’ll engage in short bursts of cardio on a treadmill or stationary bike. This improves blood flow to the brain and triggers the release of neurochemicals that help your brain respond to therapy. One of these chemicals is called brain-derived neurotrophic factor (BDNF).
BDNF promotes communication between different brain areas and helps your brain benefit more from subsequent therapies.
Our therapists also combine and integrate different therapies. For example, you may have to balance on a Bosu ball while tossing color-coordinated tennis balls back and forth and naming foods for each letter of the alphabet. This activity helps your brain to train balance, hand-eye coordination, and word recall at the same time, which in turn promotes healthy neuroplasticity and recovery.
.jpg?width=778&height=1167&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(4).jpg)
Throughout the day, you’ll have periods of rest and relaxation to allow your brain time to recover before the next therapy session. This may include neuromuscular massage to the neck and shoulders, mindfulness and breathing exercises, or going into a dark room and listening to binaural beats.
At the end of treatment, you’ll undergo a follow-up fNCI to allow our team to see how brain function is improving. Most of our patients experience significant symptom improvements during treatment and continue improving at home.
Finally, you’ll have a meeting with a member of our team to discuss your results. They will also give you some homework to do at home which typically includes some aerobic exercises, cognitive games, and cognitive rest. This regimen promotes further healing at home.
At this point, you may find that you’re able (under a doctor’s supervision) to reduce medications, which can bring further relief due to reduced side effects. (Read more about the difficulties of managing medication for post-TBI symptoms.)
If you’ve tried isolated types of therapy with limited success, Cognitive FX may be the way forward to treat your condition. Why not schedule a consultation to see what we can do for you? We offer access to many different therapies under one roof, and our treatment is tailor-made for you based on an in-depth analysis of your symptoms and your brain imaging results. To our knowledge, there is nowhere else in the world where you can get this kind of treatment for traumatic brain injuries.
How to Maximize Recovery at Home
.jpg?width=1000&height=475&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(9).jpg)
As you undergo your rehabilitation process, here are a few suggestions of what you can do at home to maximize your chances of recovery:
- Complete the homework that our therapists suggested at the end of your treatment. This includes aerobic exercises, cognitive activities, and breathing exercises, and it’s the best way to continue improving after treatment.
- Limit alcohol and caffeinated drinks while you recover from TBI. It’s helpful if you can avoid them entirely during the initial stages of your recovery, but it’s also important not to introduce an abrupt change (such as going from five cups of coffee to none). Gradual adjustments are easier on your brain.
- Follow a brain-friendly and balanced diet.
- Use an app on your phone to remind you of what you have to do, such as doctor's appointments or work meetings. To help your memory improve, try to remember each task before checking your notes.
- Focus on a single task rather than attempting to multitask. If you struggle with focus, find a quiet environment with minimal distractions and develop routines which help you get in the zone.
- If you feel overwhelmed about something, walk away and try relaxation or breathing techniques to help your brain calm down. Self-care is important all the time, but especially when your brain is recovering from injury.
- Follow a good sleep routine and take short breaks during the day when you feel tired. If you need a nap, don’t sleep more than 20-30 minutes to avoid disrupting your sleep at night. Getting quality sleep after a brain injury can be difficult, but there are steps you can take to improve your rest.
- Pace yourself during the day, especially if you need to do something that may trigger your symptoms.
- Talk to family members or close friends before making important decisions.
- Avoid excessive screen time, such as playing video games or working on a computer, for long hours.
- For sports injuries that are milder, consult the Centers for Disease Control and Prevention (CDC) HEADS UP program for advice on return to play.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in therapy for persistent brain injury issues. To see if you are eligible for treatment, sign up for a consultation.

.jpg?width=1999&height=1333&name=Vision%20Problems%20After%20COVID%20Causes%20and%20Treatment%20(1).jpg)
.jpg?width=552&height=349&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(3).jpg)
.jpg?width=1333&height=1816&name=Physical%20therapy%20covid%20(2).jpg)
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(5).jpg)
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(2).jpg)
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(7).jpg)
.jpg?width=1999&height=1333&name=Why%20Most%20Post-Trauma%20Vision%20Syndrome%20Treatment%20Falls%20Short%20(3).jpg)
.jpg?width=1999&height=1333&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(8).jpg)
%20(5).jpg?width=552&height=368&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(5).jpg)
.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(7).jpg)
-1.jpg?width=552&height=303&name=Physical%20therapy%20covid%20(3)-1.jpg)
.jpg?width=778&height=1167&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(4).jpg)
.jpg?width=1000&height=475&name=Therapy%20for%20Traumatic%20Brain%20Injury%20Can%20It%20Help%20Patients%20(9).jpg)







