Personality changes (or what feels like them) are common following a traumatic brain injury. Even a concussion can affect the brain long after it’s healed from the initial injury. The way we process and understand information can change due to the injury, so it’s not surprising that our emotions are affected too.
After a brain injury, you might suffer from social anxiety, irritability, anger, depression, feelings of overwhelm, general anxiety, mood swings, or emotional lability (teariness). But make no mistake: While these symptoms can make it seem like you’re a different person now, your personality is intact. It’s just buried under the weight of emotional symptoms that are so, so hard to handle.
Think of personality as a collection of traits, and your mood as your current state of being. Normally, our moods don’t last for weeks or months on end. But after a head injury, negative moods like sadness, anxiety, or irritation can drag on, making patients and their families mistake the emotional symptoms for personality changes.
But post-injury emotional changes don’t usually lead to a true personality disorder. Instead, they’re from symptoms that will disappear if you get the right treatment.
Undergoing these emotional changes or watching your loved one suffer through them is really hard. It’s OK to be frustrated with the changes, struggle to understand them, or grieve for the past.
But if you’d like to learn more about why they’re happening and what you can do about it, keep reading. We’ll cover…
Over 80% of our patients have experienced emotional symptoms after a concussion. Many of those symptoms resolve shortly after treatment at our clinic (although serious mental health issues like depression and anxiety can take additional therapy to resolve). If you’d like to learn more about how we can help you, book a consultation.
Note: Data relating to brain function mentioned in this post may be from our first-generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1 and averages are still forthcoming.
Why You Experience Mood Changes (Personality Changes) After Head Injury

Personality changes can originate from three sources following a brain injury:
- Specific physiological changes in the brain, which affect how it takes in, processes, and perceives information.
- Emotional reactions (a natural response) to the changes in your life brought on by a brain injury. Other concussion symptoms can contribute to this response.
- Medication side effects.
On the most basic level, a concussion can disrupt the connections between neurons and the blood vessels in your brain (called neurovascular coupling). In most post-concussion patients, those pathways return to normal after a few weeks. But in as much as 30% of concussion patients, this altered, inefficient way of processing information and responding to the brain’s needs results in long-lasting symptoms.
Read more about persistent post-concussion symptoms and why they happen here.
Note: Keep in mind that you can have lingering symptoms from even a quote-unquote “mild concussion.” Every brain injury—even ones that don’t stem from a blow to the head — can cause serious symptoms and may need treatment to resolve.
The location of the injury can contribute too. Brain injuries can damage connections that go from the cerebral cortex (the part of the brain that has a role in memory, attention, perception, cognition, and awareness) to the limbic system (the part of the brain that supports functions like emotions, behavior, and motivation).
These connections allow us to evaluate our emotional reactions, understand how important events are, and decide on a response appropriate for the situation. When these connections are injured, the emotional response differs from what it was before the injury and is not always in sync with the current situation.
The hippocampus is a part of your brain known for converting short-term memories into long-term memories. Your memories advise how you respond to your environment or the world around you, including determining your emotional response. About 63% of the patients we see at Cognitive FX have abnormal fMRI scans in one or both of their hippocampi.
In other words, there are ample opportunities for a brain injury to disrupt the way your brain normally processes information and emotions, leaving you vulnerable to a host of unpleasant mood changes. But those mood changes don’t have to last forever: Brain dysfunction after a concussion is not the same as irreversible brain damage.
Second, don’t discount the trauma you’ve experienced: It’s normal to be upset and frustrated after sustaining a life-changing injury. It can take time to process your emotions and return to some kind of 'normal'. Plus, the physical symptoms you experience may also take a toll on your emotional health. If you’re feeling fatigued, plagued by headaches, becoming overwhelmed by the sights and sounds around you, or drowning in a mental fog, it makes sense that you might also feel anger or sadness!
To learn about other cognitive and physical contributors to your symptom burden, please see the following resources:
- Post-concussion headaches: Learn what causes headaches after a mild head injury, how they manifest, and how to treat them.
- Post-concussion fatigue: Learn what’s making you so tired and how to reclaim your energy.
- Functional vision problems and light sensitivity: Learn all the ways a head injury can affect your vision and how therapy can help you recover.
- Sleep with post-concussion syndrome: Learn about the most common post-injury sleep problems and what you can do about them.
- Brain fog and PCS: Learn what causes cognitive impairment after a brain injury and how to overcome cognitive deficits from a brain injury.
- Difficulty exercising post-concussion: Learn how to exercise safely after a concussion, even if you’re feeling dizzy or getting headaches when you try cardio.
- Gastrointestinal symptoms and nausea: Learn about concussion-related symptoms like loss of appetite, stomach upset, food intolerances, acid reflux, and more.
- Blood pressure changes and POTS: Learn how concussions can affect your blood pressure and cause a secondary condition called POTS.
- Feeling hot, cold, or fevered: Learn how concussions affect your body temperature, what symptoms to watch for, and how to handle them.
- Memory loss, short-term memory problems, and long-term memory problems: Learn how memory loss has affected some of our patients and how it improved after treatment.
- Intolerance of caffeine or alcohol: Learn why a head injury could mean you’re no longer able to enjoy caffeinated or alcoholic beverages.
- Difficulty balancing, vertigo, and other vestibular symptoms: Learn why vestibular problems happen after a concussion and how to find relief via vestibular therapy.
- Heart rate changes, palpitations, and more: Learn how concussions can affect your heart and how to address those changes.
- Post-concussion neck pain: Learn what to do when concussions cause neck pain after a head injury.
Finally, don’t rule out medication as a possible source of neuropsychological distress. Some health care providers prescribe various antidepressants, anti-seizure medications, pain meds, and other pharmacological substances when concussion patients don’t show improvement after a short period of time.
Further reading: Medications for post-concussion syndrome (and why so many patients struggle while taking them)
Post-Concussion Emotional Symptoms
A brain injury is emotionally traumatic. It is normal to mourn the life you once had and to try to find ways to cope with ongoing symptoms. Brain injury survivors can be affected by the impaired neuronal connections described earlier and may have unexpected behavioral changes.
If your brain has dysregulated neurovascular coupling, that means some regions of your brain regions are hypoactive (not doing their fair share). Other areas in your brain might work overtime in an attempt to make up the difference.
That makes it very easy for you to be overstimulated: Overwhelmed by sensory inputs, like light and noise, and cognitive inputs, like a conversation, reading, or work. That overstimulation can be the culprit behind many emotional symptoms.
Let’s explore each.
Anger and Irritability After Concussion
We see a high incidence of irritation and impatience in our patient population (and for good reason). For example, this attorney (who was injured in a car accident) was unable to fix a broken ice maker, which caused him to explode at family members. Previously, it wouldn’t have bothered him at all. But when he visited the emergency department, no one warned him he could experience anger, depression, and other emotional effects from his injury!
After head trauma, it’s easy to react more dramatically to a given situation than you would have before the injury. Why? Because you’re already dealing with so much!
If you have lingering post-concussion symptoms, then your body and brain are trying to handle more than they ever had to before. What was previously a minor inconvenience feels like a national emergency to a brain that’s already juggling more than it can handle. Plus, other common symptoms like headaches, neck pain, and poor sleep quality can shorten your fuse, too.
That overstimulation is behind much of the irritation, angry outbursts, aggressive behavior, and mood swings you may experience after a head injury. Try to remain patient with yourself and look for ways to keep yourself from getting overstimulated. (We’ll provide some tips later in the post.)
Also, keep in mind that you may have unresolved feelings of anger at the situation you’re in. Most people don’t expect to have lingering symptoms. They didn’t ask for their injury. They might be belittled by their doctors and start to doubt themselves. That confusion and frustration can absolutely contribute to emotional difficulties.
Anxiety After Concussion
After a concussion, you may find yourself worrying in ways you never did before. Or, you may find that your previous worrying becomes even worse. Feeling on edge, struggling to fall and stay asleep, and constantly thinking about what could go wrong are characteristics of concussion anxiety.
We’ve written a whole post on the topic of post-concussion anxiety. You can read that post to learn more about why concussions can result in anxiety and how to cope. If you think you’re suffering from post-traumatic stress disorder, read our post on concussion-related PTSD instead.
Depression After Concussion
Depression after a concussion is common, especially if you’ve suffered from depression in the past.
A recent study showed that students who have experienced a concussion have a higher risk of self-harm, depressive symptoms, attempted suicide, injury from attempted suicide, and overall poorer mental health outcomes. Another study showed that the suicide rate was almost twice as high among individuals with TBI than those without a brain injury. Finally, people who sustained multiple brain injuries are at increased risk of developing symptoms of depression and committing suicide.
Seek professional help immediately if you experience suicidal thoughts. Your life is worth living and you can get better. For immediate assistance, call the national suicide prevention lifeline: 1-800-273-8255. Follow up with a local psychological care provider or similar medical professional.
Read this post to learn more about depression after a mild traumatic brain injury.
Emotional Lability (Crying) After Concussion
It’s normal to cry from feelings of grief or loss after a mild TBI results in lingering and traumatic symptoms. In fact, it’s healthy to cry and process some of the emotions you’re feeling.
But some patients find themselves confusedly crying over trivial matters or for seemingly no reason. If you find yourself teary-eyed after commercials, you are likely experiencing something called emotional lability. Emotional lability causes uncontrollable tears (or laughter), sometimes at the most inconvenient moments.
In post-concussion patients, this can be related to overstimulation—it may be your body’s way of coping when your brain can’t handle everything it needs to. Rather than being frustrated with yourself (or, if you’re a family member, getting angry about the crying), handle the situation with levity. It’s healthier to laugh and acknowledge that the tears are out of your control than to struggle against them and increase your frustration.
Note: Did you know that loss of consciousness does not make you more likely to suffer from lingering concussion symptoms? Instead, you’re more likely to suffer from long-term effects of concussion if you have a history of concussions, are female, or had mental confusion at the time of injury.
Impulsivity After Concussion
Concussions can cause memory loss, long or short-term memory problems, difficulties with focus and conversation tracking, brain fog, and more. It shouldn’t come as a surprise that head injuries can affect impulse control as well.
We often see concussions and ADD together. Teasing out exactly what’s responsible for impulsivity requires examination by an experienced clinician.
For example, we might use imaging to discover that the concussion caused dysregulation in the cingulate gyrus or anterior insula, both of which are brain regions involved in emotions and impulse control. Alternatively, disinhibition and related behavioral changes could arise from sleep disruption due to the injury.
All of those causes are treatable, but you have to know what the root issue is in order to solve it, which means visiting a doctor who can correctly diagnose the problem.
Social Struggles After Concussion
A common complaint we hear from patients is that they used to be outgoing, but now they don’t want to visit friends or spend a night out. It’s not that you switched from being extroverted to introverted: Instead, your symptoms are likely causing that "night on the town" to cease being fun.
Avoiding social functions might be rooted in a symptom like fatigue — some people are just too tired to go out. Or, it might be that you no longer enjoy conversations because you struggle to follow what everyone is saying. Maybe finding the right words to say is difficult and frustrating. Perhaps the noise or light contributes to your headaches. Maybe you just get overstimulated quickly.
There are so many reasons why post-concussion patients avoid social outings. The good news is that none of them involve permanent personality trait changes.
What to Do About Post-Concussion Emotional Symptoms

We recommend working with a psychologist or neuropsychologist to manage emotional changes until you’re able to receive treatment for post-concussion syndrome. In the meantime, there are a few things you can do (with or without the help of a therapist).
Identify Your Triggers
Identify your triggers, especially for overstimulation. What do you feel right before an angry outburst or before you get overwhelmed? If you know when you’re headed for trouble, it’s easier to change course. For example, some patients notice feeling brain fog, dizziness, or nausea.
Get a Family Member to Help
If you’re comfortable with it, have trusted family members or caregivers monitor your overstimulation. They might pick up on cues that you don’t notice, like getting a glassy-eyed look. They can tactfully remind you to take care of yourself and destimulate.
If you’re a caregiver, just be aware that unsolicited interventions may not help the situation. For example, someone who usually would be comforted by a touch on the shoulder might get worse due to the additional sensory input. It’s important to talk to your loved one about what helps them or hurts them in the moment.
Make a Plan for Brain Breaks
Speaking of destimulation, have a plan for when you’re getting overwhelmed. You might hide in the bathroom for five minutes (or any quiet room you can find), close your eyes for a bit, or even purposefully disengage from your current activity (e.g., if you’re stuck in a lecture hall, you might need to “space out” for a few minutes).
Do what you need to do to reduce environmental, cognitive, and emotional stimuli until you’re feeling more normal again.
Further reading: How to know when your brain needs a break (and what to do when you take one)
Name the Emotion
Name each emotion you’ve experienced postinjury. Examine how your feelings about yourself have been affected by these changes. Sometimes, just acknowledging and understanding what has happened to you can help.
Get Some Exercise
Some folks have difficulty exercising after a concussion, but it’s still important to do whatever exercise you can do safely. It will help relieve stress and tension, plus it provides your brain with a biochemical boost to help it handle the day’s needs and may even help you manage other health problems. This post on post-concussion exercise can help you get started.
Keep a Journal
Don’t have anyone to talk to? Struggling with verbal expression of your feelings? Just need another outlet? Journaling can help with that. It gives you a way to process your thoughts and feelings on your timetable.
Join a Support Group
You can look for support groups for your specific emotional struggles (such as anger management), or you can follow the link to look for a post-concussion syndrome support group. Look for a group that encourages you and equips you with strategies to better manage your symptoms.
Above All, Get the Right Treatment
Long-lasting symptoms will not resolve without treatment. If you’ve experienced emotional problems and other common concussion symptoms for over three months, it’s time to seek help. We’ll explain what that looks like in the next section.
Note: While our program primarily serves mTBI patients, we are often able to help severe traumatic brain injury survivors as well. For example, one of our patients feels “95% recovered” after a life-threatening fall that left her in a coma for three months. Follow the link for more information on our treatment for severe TBI patients.
Getting Treatment for Post-Concussion Emotional Changes

Treating a brain injury isn’t one size fits all. Many programs will provide the same 2-3 therapies or other treatment options for each patient who comes through their program. Some of their patients get better, but some don’t (as this high school student found out). That’s because concussions don’t cause brain dysfunction in the exact same brain regions for everyone. Knowing which regions to treat means you can tailor the treatment experience to the individual person.
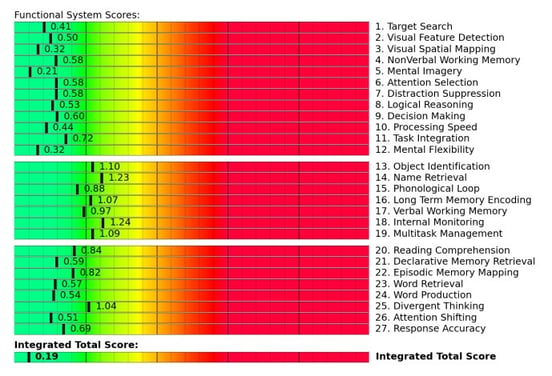
That’s why our assessment includes an fNCI scan. It allows us to look at blood flow dynamics in 56 areas of the brain, along with the connections between them. As a result, we have a good idea of which brain regions were affected by the concussion(s).
Here’s an example of the fNCI report for a healthy patient:
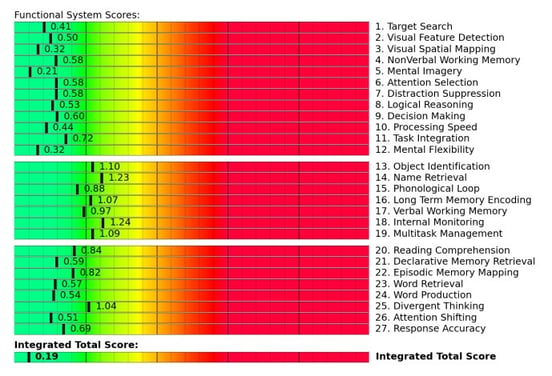
The report scores the overall health of brain functions such as name retrieval, problem-solving, multitasking, decision making, tuning out distractions, and many other cognitive processes. This information helps therapists tailor the treatment regimen to your brain’s specific needs.
Once we’ve finished the evaluation (collecting data on your physical response times, cognitive function, and medical history in addition to the fNCI scan), it’s time to get to work.
We use a combination of exercise and multidisciplinary therapies, including (but not limited to) cognitive, occupational, neuromuscular, and sensorimotor therapy. Patients meet with a psychologist (psychotherapy) at least twice during treatment.

For example, during cognitive therapy, you might listen to recorded restaurant sounds while listening to a therapist list random words. Your job would be to tune out the background noise well enough to identify opposite word pairs and tap the table whenever they happen (for example, “chair, table, south, up, down, band, stretch, dog, east, west…”).
Or, during sensorimotor therapy, you might be asked to state out loud arrow directions while stepping, tapping, and clapping in a four-step pattern along with a metronome. It might sound easy, but saying “right” while moving your left foot in time with a rhythm gets tricky quickly!
All of these therapies help your brain and body work together in a healthier manner to alleviate physical and cognitive symptoms. They’re based on the best neuroscience research available today.
To make treatment as effective as possible, patients engage in supervised aerobic activity. Cardio exercise results in a Post Exercise Cognitive Boost (PECB): an increase of essential neurotransmitters and proteins in your brain that help develop and promote healthy blood flow. The PECB means your brain is in better condition to tackle the challenges we give you in therapy and engage in neuroplasticity for recovery.
For example, exercise releases brain-derived neurotrophic factor (BDNF), which has been shown to improve therapy outcomes for post-concussion patients.

At the end of the week, every patient gets a second fNCI scan so we can see how well their brains are progressing. The average improvement on the second scan is 77%! If patients keep up with their homework after treatment, they typically see further improvement at home.
In the clinic, we’re primarily focused on resolving brain dysfunction. When that happens, many of the emotional and behavioral changes resolve too. Each patient is also assessed for psychological disorders (like PTSD and depression). We make sure that every patient has a tailored plan to continue appropriate therapy in their hometown (if needed). This aspect of recovery is far easier when the primary issue — brain dysfunction due to injury — is better.
If you've experienced one or more concussions and your symptoms persist, you're not alone — and you're not imagining it. Help is available. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. If you’d like to learn more about how we can help you recover, sign up for a consultation with our team.