For a long time, emotional symptoms as a consequence of a traumatic brain injury (TBI) were only recognized in people with severe injuries. In the past two decades, however, there has been tremendous growth in the understanding of how even moderate and mild traumatic brain injuries (mTBIs) can affect mental health.
Studies have found that over half of patients with moderate to severe TBIs develop symptoms of depression in the months and years after their injury. Furthermore, a significant portion of patients who sustain mild TBIs also experience symptoms of depression. For example, over 80% of our patients have reported symptoms related to mood or personality following their head injury.
Unfortunately, despite the growing knowledge of how TBIs affect mental health, the contributing factors to depression in TBI patients are not well understood by the wider medical community (including by many doctors of psychiatry and neurology). As a result, many patients struggle to get the support and treatment they need to resolve their emotional symptoms and feel better.
In this post, we discuss why and how depression in TBI patients needs to be treated differently than depression in non-TBI patients. Below we cover:
Over 80% of our patients have experienced emotional symptoms after a concussion. Many of those symptoms resolve shortly after treatment at our clinic (although serious mental health issues like depression and anxiety can take additional therapy to resolve). If you’d like to learn more about how we can help you, book a consultation.
Why Treating Depression in TBI Patients Requires a Different Approach
.jpg?width=1557&height=1072&name=Dr.%20Alina%20Fong%20with%20a%20patient%20at%20Cognitive%20FX%20(V2).jpg)
The context in which TBI patients come to feel depressed is unique compared to the general population. Specifically, their depressive symptoms often stem from functional changes in the brain that resulted from their injury, such as neurovascular coupling dysregulation (NVC) or autonomic nervous system dysfunction.
These issues, which we describe in more detail below, can lead TBI patients to experience a wide array of symptoms including, for example, regular mental and physical fatigue that leaves them feeling depleted. In turn, this depletion can cause patients to experience low motivation, lack of enthusiasm, and a flattening of mood.
Sometimes, this depletion is mistaken for depression — both by patients and their healthcare providers. In these cases, patients are often prescribed antidepressants that only make matters worse, leading to unwanted side effects and failing to treat the root causes of their symptoms.
This is not to say that TBI patients can’t experience depletion and clinical depression at the same time. This example simply demonstrates the nuance of how underlying factors due to functional changes in the brain can lead to depressive symptoms in TBI patients — and how these issues can’t be addressed with standard depression treatments alone.
Instead, as we’ll explain below, treating depression in TBI patients needs to include treating the physical and cognitive symptoms of the TBI (e.g. depletion) alongside the emotional symptoms.
Common Symptoms of Depression in TBI Patients

The word depression is an umbrella term that can be used to describe various mental health conditions. For TBI patients, we take “depression” to mean a disordered mental state, characterized by having some combination of these types of feelings:
- A negative feeling that goes beyond normal sadness (it might feel a bit like grief, but you recognize it as being distinct from grief)
- Low or no motivation, such that your ability to do what you need or want is compromised
- The inability to feel pleasure (anhedonia)
- A persistent disinterest in things (apathy)
- Feeling of emotional heaviness or like you’re moving through mud
- Feeling empty or robotic
- A negative outlook about yourself, the world, and/or the future
- A sense of worthlessness
- Indecisiveness
- Suicidal ideation
In addition, there are many different factors which may increase the risk of developing this condition, including:
- Multiple concussions: The risk of developing depression increases in patients who sustain multiple concussions. Studies show that the risk of developing depression doubles in patients who report more than three concussions compared to patients who suffered only one.
- Previous mental health problems: Patients with a history of mental health disorders have a higher risk of developing major depression following head injury. For example, a study found that patients with a pre-existing psychiatric condition were five times more likely to develop depression. Even a history of psychological conditions in the family doubled the patient’s risk of developing depressive symptoms.
- Serious traumatic event: Military personnel involved in serious war injuries tend to have higher rates of depression that take longer to recover compared to sports-related injuries, where athletes recover faster from milder symptoms.
- Higher severity of symptoms after the injury: A higher risk of depression is also linked with a higher number of more severe TBI symptoms after a head injury. This relationship occurs in both adults and children with a brain injury.
- Female gender: Women are 50% more likely than men to develop major depressive disorder after suffering a TBI. Researchers aren’t sure why this higher prevalence occurs.
- Teenagers and adolescents: Sustaining a concussion during adolescence or teenage years comes with a high risk of developing depression, often accompanied by thoughts of self-harm or suicide. During this period, fast growth in the limbic and prefrontal cortex regions in the brain often leads to difficulty regulating emotions, making young people particularly vulnerable to psychiatric disorders and emotion dysregulation following head injury.
Again, depression can have various causes, risk factors, and expressions. In this post, we’re focused only on the most common types of depression for TBI patients. If you experienced signs of depression before your head injury, whatever caused your depression previously may also be at work now.
Note: If you are experiencing suicidal thoughts, please seek help from a qualified medical professional. You matter, and you can get better. In emergencies, call the National Suicide Prevention Hotline at 1-800-273-8255.
Understanding How Grief Relates to Post-TBI Depression

Earlier we discussed how sometimes TBI patients and healthcare professionals can mistake depletion for depression. Grief is another aspect of TBI that can be mistaken for depression.
You may be familiar with the five facets of grief: denial, bargaining, anger, sadness, and acceptance. Not everyone experiences all five and might not experience them in that order; they might bounce back and forth between the five facets.
The “sadness” stage of grief has some similarities to clinical depression: You may experience feelings of loss, emptiness, and sadness. You might even experience some disinterest. But key differences between grief and depression are feelings of worthlessness, low motivation, apathy, meaninglessness, hopelessness, and suicidal thoughts. Depression sufferers often have these features whereas those suffering from grief generally don’t.
When grief about injury-related losses and limits is at the heart of your sadness, your depression-like symptoms often will resolve more quickly than depression once you’ve been through treatment for the physical and cognitive impairments from your TBI and are less limited by the injury.
Key Factors That Contribute to Depression in TBI Patients
The following are all possible contributors to depression in TBI patients:
Note: None of these issues can be addressed through standard methods for depression treatment. They require specialized treatment like what we offer at our clinic (described below).
Structural Damage to the Brain
For patients who started experiencing depression shortly after their injury, these symptoms likely resulted from damage to the areas of the brain that control emotions and mood, including the amygdala, the thalamus, and the hippocampus. For example, in patients with depression, the hippocampus (an area involved in long-term memories), as well as the left superior parietal gyrus and the bilateral orbitofrontal cortex (involved in decision making) were less active than normal, whereas the amygdala (an area associated with emotions such as anger, sorrow, and fear) is more active.
Neurovascular Coupling Dysregulation
In many of our patients, depression arises due to changes in neurovascular coupling. In a healthy brain, when nerve cells need to complete a particular task, they can request what they need — energy and oxygen — from a network of surrounding blood vessels. These blood vessels then ensure that these resources are delivered at the right time to the right place. This dynamic relationship is called neurovascular coupling (NVC).
Brain injuries often disrupt this neurological mechanism, and some areas of the brain don’t receive what they need (either get too much or too little) or they get delivered at the wrong time. This disruption can cause headaches, fatigue, poor sleep, irritability, and sensory sensitivity. If this disruption occurs in any of the areas mentioned above, it can also lead to depressive symptoms.
Autonomic Nervous System Dysfunction
Head injuries can also lead to an imbalance between two key parts of the autonomic nervous system (ANS): the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
Under normal circumstances, the SNS and PNS work together to regulate many bodily functions, including heart rate, speed of digestion, blood pressure, breathing rate, and sleep. In simple terms, the SNS governs the fight-or-flight response and prepares the body to handle stressful situations, while the PNS has a more calming effect on the body.
Instead of working together, the SNS often becomes dominant after a brain injury, and PNS’s influence is limited. This creates a constant state of tension and stress which disrupts the patient’s emotional regulation and increases the risk of depression, anxiety, and other negative feelings.
Patients feel overwhelmed and anxious, even during activities they enjoyed before the injury. For example, they may get angry after being called for dinner two or three times while trying to read. Normally, this wouldn’t be a problem, but after the injury, it takes enormous effort to shift attention away from the book and go for the meal. Even in simple scenarios like this, patients experience physical symptoms, such as nausea, dizziness, and exercise intolerance as part of their ANS dysfunction.
Further reading: Dysautonomia after a head injury
Inflammatory Response
Researchers don’t fully understand the mechanism behind this process, but inflammation in the brain triggered by the TBI may cause (or at least exacerbate) depression in some patients. An exaggerated inflammatory response in the brain may cause changes in areas of the brain involved in behavior. These patients typically respond poorly to antidepressants; targeting the inflammation rather than the depression symptoms may be a better way to provide care.
Hormonal Imbalance
TBIs can lead to hormonal problems when the hypothalamus and pituitary gland are affected. These two glands are the main players in the endocrine system and control major bodily functions, such as the heart rate and blood pressure, body temperature, appetite and body weight, sleep cycle, and function of the gastrointestinal tract.
If they’re affected after a head injury, they can lead to a variety of psychological and emotional problems. For example, low thyroid levels can cause patients to feel sluggish, tired, less interested in activities, and irritable. We’ll delve into this in more detail later, but this is a case where taking antidepressants is not going to solve the problem. Instead, patients need to see an endocrinologist to check hormone levels. This is not something we offer at Cognitive FX, but can refer you to a specialist if needed.
Emotional Response to Injury
Some patients develop depression if they struggle to function in their day-to-day activities due to their head injury. This is particularly true for patients who are experiencing symptoms so severe that they have to stop working or engaging in activities they enjoy because of their head injury.
This significant impact on their quality of life often leads to feelings of meaningless and loss of purpose, with patients feeling disaffected at home and work and constantly ruminating about the person they were before the injury. Patients may feel hopeless, and unable to find enjoyment in the things that used to bring them pleasure, which in turn can lead to depression and anxiety, especially when patients feel that they’re never going to recover.
Seeking Treatment for Post-TBI Depression
When is it time to seek treatment for post-TBI depression? That depends on a few factors. Always seek treatment if you’re experiencing suicidal ideation.
If how you’re feeling is interfering with your day-to-day life, that’s a good sign to seek treatment. And if you’re asking the question, “Should I get treatment?” the answer is probably yes.
With that said, there are two types of treatment to pursue: treatment for post-TBI brain dysfunction and treatment for depression. If you’re still experiencing symptoms in addition to depression months or years after your brain injury, then we strongly recommend getting treatment; those symptoms are unlikely to resolve without professional intervention.
The outcome of post-TBI treatment can then determine whether you need follow-up care from a psychologist or other mental health care provider regarding your depression.
How We Treat Post-TBI Brain Dysfunction Alongside Emotional Symptoms at Cognitive FX
At Cognitive FX, we specialize in treating patients with post-concussion syndrome (PCS). However, we also help patients with other forms of TBI, such as transient ischemic attacks (TIAs) and carbon monoxide poisoning.
One common issue that we see in our patients is that their previous healthcare providers dealt with each symptom separately, typically with medication — painkillers for headaches, antidepressants for depression, and sleeping pills to address sleep disturbances, for example. The problem with this approach is that doctors don’t treat the underlying causes of these issues that their injury has caused.
In contrast, we use a multidisciplinary approach that considers all the symptoms holistically. This includes physical, cognitive, and psychological symptoms, such as depression and anxiety.
Treatment starts with an in-depth patient assessment. Patients undergo a variety of exams, including:
- A review of the patient’s medical history and symptoms present.
- A physical exam to assess balance, hand-eye coordination, functional vision, reaction times, and other physical abilities. For example, patients perform tests using digital eye-tracking software to help our therapists identify vision deficits, such as difficulty tracking or poor peripheral vision.
- A cognitive assessment to evaluate memory, focus, thinking, and other cognitive functions.
- A psychological evaluation to assess mood disorders such as anxiety and depression, as well as other psychological conditions. This includes, for example, assessing emotional states, thought patterns, and overstimulation.
- A structural brain and cervical spine MRI to identify serious structural injuries that need medical treatment.
During the initial evaluation, our team also looks for signs of ANS dysfunction, and a neurointegration specialist evaluates how well the patient’s inner ear, eyes, and body communicate with each other. We repeat the same tests at the end of the treatment to assess how much the patient has improved.
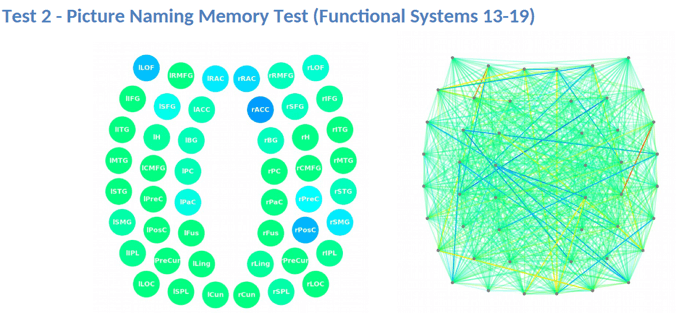
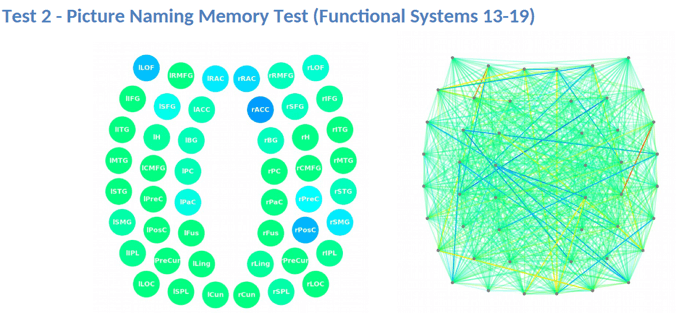
Our patient assessment continues with a brain scan called functional neurocognitive imaging (fNCI). In contrast to CT scans or standard MRIs, fNCI scans measure blood flow in 100 different brain regions while patients carry out a set of standardized cognitive tasks. They produce a series of real-time images that are combined and compared with scans from healthy people to identify the areas where neurovascular coupling (NVC) dysfunction is affecting normal brain function.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with NVC dysfunction.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
This information provides our staff with huge advantages when it comes to treating patients.
Once we’ve finished our patient evaluation, we use a combination of exercise and multidisciplinary therapies, including (but not limited to) cognitive, occupational, neuromuscular, and sensorimotor therapy.

During cognitive therapy, you might listen to recorded restaurant sounds while listening to a therapist list random words. Your job would be to tune out the background noise well enough to identify opposite word pairs and tap the table whenever they happen (for example, “chair, table, south, up, down, band, stretch, dog, east, west…”).
Or, during sensorimotor therapy, you might be asked to state out loud arrow directions while stepping, tapping, and clapping in a four-step pattern along with a metronome. It might sound easy, but saying “right” while moving your left foot in time with a rhythm gets tricky quickly!
All of these therapies help your brain and body work together more healthily to alleviate physical, cognitive, and psychological symptoms. They’re based on the best neuroscience research available today. For example, addressing ANS dysfunction can help with anxiety, and dealing with physical problems can help patients feel less tired, which in turn boosts their engagement in life and well-being.
Patients engage in supervised aerobic activity to make treatment as effective as possible. Cardio exercise results in a Post Exercise Cognitive Boost (PECB): an increase of essential neurotransmitters and proteins in your brain that help develop and promote healthy blood flow. The PECB means your brain is in better condition to tackle the challenges we give you in therapy and engage in neuroplasticity for recovery.
For example, exercise releases brain-derived neurotrophic factor (BDNF), which has been shown to improve therapy outcomes for post-concussion patients.

Patients also meet with a psychologist at least twice during their treatment. These sessions aim to help patients understand which of their symptoms are caused by psychological or emotional issues ( and can be addressed with psychological treatments) and which of their symptoms are due to depletion, ANS dysfunction, or other neurologic dysfunction (and can be addressed by staff in our clinic).
At the end of treatment, every patient gets a follow-up fNCI scan to see how well their brains are progressing. The average amount of improvement is a 77% reduction in symptoms! If patients keep up with their homework after treatment, they typically see further improvement at home.
We ensure every patient has a tailored plan to continue appropriate therapy in their hometown (if needed). This aspect of recovery is far easier when the primary issue — brain dysfunction due to injury — is better.
Note: While our program primarily serves patients with mild TBIs, in some cases we can help patients who’ve suffered severe injuries as well. For example, one of our patients feels “95% recovered” after a life-threatening fall that left her in a coma for three months. If you’d like to learn more about how we can help you recover, sign up for a consultation with our team.
Considerations Regarding Antidepressant Medications

Antidepressants are commonly prescribed for treating depression in TBI patients. However, the results of antidepressant interventions are inconsistent, especially for patients with brain injuries. For example, Sertraline, a selective serotonin reuptake inhibitor (SSRI), can work preventatively and reduce the onset of depression in PCS patients. However, it’s no more effective than a placebo in patients who already developed depression following a TBI.
This is likely because TBI-related depression can have many causes, as described above, and antidepressant medications are not designed to help with many of them. For some patients, depressive symptoms won’t go away until the underlying factors triggered by the brain injury — such as neurovascular disruption or dysfunction of the autonomic nervous system, for example — are treated. For these patients, antidepressants are often of very little value.
Should TBI Patients Take Antidepressants?
We believe antidepressants are rarely the best option to treat depression in TBI patients. At best, we see these drugs as being part of a larger treatment plan for some patients, which also includes psychotherapy (such as Cognitive Behavioral Therapy) and the multidisciplinary therapies discussed above.
Scientific evidence supports our views. There is very limited research suggesting that antidepressants can help neurotrauma patients. Some studies show that antidepressants can help patients when accompanied by psychotherapy, but when used alone, most studies found no improvements in TBI patients receiving antidepressants.
The issue is that antidepressant medications don’t address the root causes of depression in TBI patients. Antidepressant medications are thought to address chemical imbalances in the brain, such as low serotonin levels (although this has yet to be proven). If TBI patients are experiencing depressive symptoms caused by NVC disruption or ANS dysfunction (as described above), these anti-depressant medications are not likely to help.
The decision to start taking an antidepressant medication is something you need to discuss with your psychiatrist or neurologist. Here are some points to consider:
- Antidepressant medications cause side effects: Side effects are common in patients treated with antidepressants and may include headaches, dizziness, stomach upset, sleep disturbances, fatigue, and difficulties with sexual intimacy. TBI patients seem more sensitive to side effects compared to patients who haven’t suffered a TBI. This happens because of metabolism changes after the injury: Instead of going to the liver (where most medications are processed and eliminated from the body), blood is diverted to the brain instead. As more blood reaches the brain, it can change the concentration of medication delivered, and increase the risk of side effects.
- Antidepressant medications take time to work: Patients may need to wait weeks to months to see any benefits. If you need to change and start on a new medication, you may have to wait for a long time to notice any improvements.
- It can be difficult to stop taking antidepressant medications: Stopping antidepressants needs to be done carefully and with the support of your doctor. You should never stop abruptly, as this may cause severe side effects.
- Antidepressant medications are not FDA-approved to treat TBI depression: At this moment, the U.S. Food and Drug Administration has not approved any medications specifically for the treatment of post-TBI depression. In practical terms, this means any drugs prescribed to TBI patients have not been tested on people who sustained a brain injury and may not operate as expected in these patients, or they may produce unexpected side effects.
- Consider that adolescents need to exercise extra caution with antidepressant medications. For example, a systematic review of publications that investigated suicide rates (and suicide attempt rates) in adolescents showed a significant increase in suicide for adolescents taking antidepressants vs. those who did not take them.
Further reading: Antidepressants for PCS patients
Key Takeaways on Post-TBI Depression
- The root causes of depression in TBI patients are often related to functional changes in the brain that result from their injury, such as neurovascular coupling dysregulation or autonomic nervous system dysfunction.
- Standard depression treatments such as antidepressants and psychotherapy cannot address these underlying factors that contribute to depression in TBI patients.
- Therefore, treating depression in TBI patients needs to involve treating their brain dysfunction first and foremost. Oftentimes, in treating their brain dysfunction, their depressive symptoms will resolve naturally.
- Additional psychological support, including psychotherapy and antidepressant medications, can be used when necessary after patients’ brain dysfunction has been addressed.

.jpg?width=1557&height=1072&name=Dr.%20Alina%20Fong%20with%20a%20patient%20at%20Cognitive%20FX%20(V2).jpg)