rTMS vs dTMS for Depression: Which Is Better?
If you’re considering brain stimulation therapy for treating major depression, you may wish to understand the differences between repetitive transcranial magnetic stimulation (rTMS) and deep...

To understand why your depressive symptoms aren’t going away, it’s important first to recognize that major depression is a complex disorder influenced by various factors. Effective treatment requires identifying and addressing these factors for each individual.
Unfortunately, many healthcare providers rely on a one-size-fits-all approach, often prescribing antidepressant medications without thoroughly assessing the root cause of a patient’s depression. As a result, many patients don’t receive the care they need.
If you or a loved one have been struggling with depression, there are likely still treatment options available. This article highlights key insights to help you get the support you deserve.
We cover:
For most people, many different aspects of their lives come together to cause depression. Here, we’ll break down the three main types of factors that contribute to depression:
These factors don’t directly cause depression, but they can increase the risk of developing depression later in life.
Researchers have identified a genetic component that may contribute to the risk of developing depression, meaning it tends to run in families. Some experts report that if a sibling, parent, or grandparent has depression, you may be two to three times more likely to develop it than those without a family history.
People with certain traits are at a higher risk of developing depression than others. Some of these traits include:
Perfectionism: Those with high standards and perfectionistic tendencies are more likely to become depressed.
High reactivity: Individuals who are more sensitive to negative emotions from stressful events are at greater risk.
Negative thinking: People who are anxious and pessimistic tend to ruminate on negative thoughts, which increases their likelihood of depression.
Low self-esteem: Low self-esteem has been linked to depression, though the relationship between the two is complex.
Social inhibition: Those who feel vulnerable in large groups and struggle to connect with others may feel isolated, increasing their risk of depression.
Impulsiveness or poor self-discipline: People who are impulsive or disorganized may be prone to depression.
Sensitivity to rejection: Those who perceive rejection or criticism from others are more likely to develop depression.
If you have any of these traits, it doesn’t mean you’ll develop depression. They’re just risk factors more common in those with depression, and the good news is they’re often learned behaviors that can be unlearned.
Women are twice as likely as men to develop depression at some point in their lives. In the United States, the lifetime risk for depression is 17.1% for women, compared to just 9% for men.
There are many potential reasons for the greater risk of depression in women compared to men. Depression is more common during phases of women's reproductive life, such as puberty, postpartum, and menopause, pointing to hormonal differences as a contributor to the gender gap in depression rates.
While some types of depression are triggered by hormonal changes (e.g. postpartum depression), the vast majority of women experience similar hormonal changes without significant depression. Current theory suggests hormonal issues may contribute to certain types of depression and cause sleep disturbances, which can also play a role.
Gender differences in depression rates can also be explained by differences in exposure to other risk factors, such as certain negative life events. These events, which are linked to depression in both women and men, are more common in women and include experiences like sexual and physical abuse, poverty, appearance pressure, negative body image, and inequality/discrimination.
Research shows that experiencing traumatic or abusive events during childhood is strongly linked to depression in adulthood. These events include neglect, domestic violence, parental substance abuse, physical or sexual abuse, extreme poverty, rejection, and death of a parent.
Up to three-quarters of adults with depression have experienced significant childhood trauma. In addition, those who experienced multiple incidents are more likely to have more severe symptoms. Researchers believe early exposure to these adverse conditions can lead to more challenging life circumstances later on and lower the threshold for reacting to and coping with stress, increasing the risk of depression.
This link may also explain why children of depressed parents are more likely to experience depression themselves. These children inherit a genetic predisposition for depression and are also often raised in high-risk conditions, including marital conflict, instability, lack of affection, poor parenting, and limited adult support.
Some of these factors are more likely to trigger depression in patients who already have risk factors, while others can trigger depression on their own, even in patients without any predisposing factors.
Stressful life events are one of the most common triggers for depression, with approximately 70% of depressive episodes being triggered by such events. Some patients experience a single traumatic event severe enough to trigger depression, while others describe a gradual downward spiral involving a series of stressful events or chronic difficulties, eventually leading to their breaking point.
Some examples of stressful life events that trigger depression include:
Any of these stressful life events or chronic difficulties can trigger the initial depressive episode, but they can also aggravate symptoms for patients already dealing with depression. In such cases, they can be described as both precipitating and perpetuating factors (more on this in the next section).
Some medications may trigger symptoms of depression; examples include:
If you suspect your medication is causing depression symptoms, it’s important to seek medical advice. Your provider will consider the benefits of the medication against any adverse effects and may suggest an alternative drug or adjustment in dosage.
Living with a chronic physical illness, such as cancer, cardiovascular disease, dementia, diabetes, multiple sclerosis, or post-concussion syndrome/TBI, is exhausting and can severely affect a patient’s life and emotional state. Not surprisingly, patients with these and other debilitating conditions are at higher risk of developing depression.
It’s estimated that up to 85% of these patients will experience depressive symptoms at some point, and they often face a poorer prognosis compared to those who have depression without chronic physical pain or illness.
Physical pain and disability may also lead to job loss, strained social connections, and prevent individuals from exercising or getting enough sleep, further increasing the risk of depression.
Perpetuating factors maintain, aggravate, or prolong the duration of symptoms in patients already experiencing depression. There is some overlap between precipitating and perpetuating factors.
For instance, in some patients, the initial trigger for depression may be the loss of a loved one, which is further exacerbated by social isolation and withdrawal. In other cases, patients who are already struggling with social interactions and depression may find that losing a loved one makes their symptoms significantly worse.
It’s not uncommon for patients with depression to drink excessively or use illegal drugs, such as cocaine, MDMA, or amphetamines, as a way to self-medicate and alleviate their symptoms.
While these substances may provide short-term euphoria and a sense of happiness, they are likely to worsen depressive symptoms in the long term and prolong the time patients deal with depression. Alcohol and drug use can also lower the efficacy of prescription antidepressant medications and contribute to an addictive cycle, where the patient needs increasingly higher doses to achieve the same effect.
The following are signs that patients may be self-medicating their depression with substances:
Patients with depression often isolate themselves and avoid social interactions, frequently coming up with excuses to avoid what they perceive as uncomfortable or difficult.
Signs of social isolation in these patients include:
This behavior can create a downward spiral, reinforcing negative thoughts about oneself, others, and the world, which further exacerbates symptoms of depression. Social isolation often leads to less exercise, poor sleep, and an unhealthy diet. It may also contribute to alcohol and substance abuse and increase the risk of suicidal thoughts.
Depression and sleep problems are closely linked. Among people with depression, about 60%–80% have trouble falling asleep or staying asleep. The relationship works both ways: people with insomnia have a tenfold higher risk of developing depression compared to those who manage to get a good night’s sleep.
For patients with depression, sleeping disturbances are a major perpetuating factor. Stressful life events, as described earlier, can lead to sleepless nights, which cause daytime fatigue and exacerbate depressive symptoms. Over time, this creates a vicious cycle of inactivity and disturbed sleep, affecting both physical and emotional health. Additionally, medications prescribed to treat depression can worsen insomnia, further aggravating symptoms.
Chronic conditions such as stroke, diabetes, arthritis, kidney disease, HIV/AIDS, multiple sclerosis, and even depression itself cause long-term debilitating symptoms. These conditions can lead to significant life changes, limiting a patient's mobility and independence, making it overwhelming to navigate such ongoing challenges.
This reality can be hard to manage, often triggering or worsening depression. It's estimated that up to one-third of people with a serious medical condition have symptoms of depression. Furthermore, the combination of chronic illness and depression may lead patients to isolate themselves or turn to alcohol, which can further exacerbate their depression.
The most common ways patients with depression receive medical support are through primary care doctors or psychiatrists. Unfortunately, both types of doctors often:
Dedicate limited time to evaluating patients and identifying the specific factors contributing to their depression.
Jump directly to prescribing antidepressant medications without exploring alternative treatment options that may be better suited to the patient’s unique needs and situation.
Primary care doctors, who prescribe 90% of antidepressant medications in the U.S., lack the time, training, and resources to conduct thorough assessments for major depressive disorder. While some psychiatrists provide more specialized care, many focus solely on medication management through short, 15-minute appointments, failing to understand which treatment options best match the patient’s unique needs.
As we’ve written about previously, there are numerous issues with relying solely on antidepressant medications for treating depression. These include:
It’s been shown that traditional antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), only work for about one-third of patients. Even when prescribed new drugs after a first or second medication fails, data suggest that less than 2% of patients have success with a third or fourth medication.
Traditional antidepressant medications involve a trial period of weeks or months before it can be determined whether or not they are working. If a medication doesn’t work, the patient must begin another trial with a different drug and go through the process all over again.
Traditional antidepressant medications commonly cause unwanted side effects, such as headaches, digestive problems, emotional numbing, decreased libido, and brain fog. These side effects can significantly impact the patient’s quality of life and well-being, especially if patients have other health conditions.
Studies show that 50%–75% of patients relapse after stopping their medication. If symptoms return, the common response is to put patients back on medication, leading many with recurrent depression to stay on antidepressant medications long-term.
To be clear, about one-third of patients do get relief from antidepressant medications. However, the current one-size-fits-all approach is failing the majority of people who suffer from moderate to severe depression.
In the next section, we’ll explain what you should be looking for to get better support.
Ideally, patients with prolonged or treatment-resistant depression (TRD) should work with a provider who specializes in treating clinical depression. It’s usually best when evaluation and treatment are orchestrated by a single doctor.
Good providers will be thorough and seek to deeply understand the patient and what may be contributing to their depression. They’ll use these insights to inform the treatment plan they prescribe, which may or may not include medication.
In our experience, psychologists are often the most comprehensive healthcare provider to assess various factors that may be contributing to a patient’s depression. While psychiatrists can treat patients with serious mental health conditions that require medication, including bipolar disorder and schizophrenia, psychologists are more likely to employ a variety of different approaches, including psychotherapy (i.e. talk therapy) to help patients understand their symptoms, the factors that contribute to their depression, and learn how to change or manage them.
In addition, psychologists are more likely to have knowledge of and/or offer alternative depression treatments that may be a good fit for certain patients.
Several well-tested types of psychotherapy have been developed specifically for treating depression. These include:
Cognitive behavioral therapy (CBT) for depression: CBT teaches patients how to identify and evaluate problematic thoughts, feelings, and behaviors associated with their depression, and modify both the content and the way thoughts are processed. It provides various strategies to cope with symptoms, such as helping patients identify and re-engage in activities they have enjoyed in the past. The goal is to help patients develop healthier thinking patterns and behaviors and move toward their goals leading to improved mood, emotional regulation, and overall functioning.
Behavioral therapy (BT) for depression: In contrast to CBT, which focuses on both thoughts and behaviors, behavioral therapy focuses only on changing behaviors and environmental factors that contribute to a patient’s depression. Also known as “behavioral activation,” BT for depression encourages patients to participate in activities that are enjoyable and rewarding to combat the withdrawal and inactivity typical of depression.
Interpersonal therapy (IPT): IPT aims to improve the patient’s relationships with others (friends, family members, etc.) by using strategies to communicate emotions and needs. It also focuses on helping patients adapt to social role transitions. As relationships with others improve and patients adapt better to their social roles, the depressive symptoms can subside, and the patient can experience improved functioning in multiple areas of life.
Compared to other psychotherapies, CBT has far more scientific and empirical support for treating depression, including a greater number of randomized controlled trials. Most meta-analyses indicate that CBT outperforms other therapies, both in the short term and especially in the long term (e.g., 6 months to 1 year post-treatment). Once treatment ends, the beneficial effects of CBT are sustained, whereas other therapies and medications often lead to relapses of depression.
Overall, research shows that CBT is superior to other psychotherapies and medications for depression in both short- and long-term outcomes, with a notable advantage in the long term. The response rate to CBT across studies ranges from 61%–87%, with large effect sizes.
It’s important to note that while CBT can be fast-acting for some patients, it generally takes weeks or months to achieve full remission of depression. This is why faster-acting treatments, such as TMS (discussed next), are also beneficial.
Due to the high demand for evidence-based depression treatment alternatives, more options are becoming available for patients who haven’t found success with traditional antidepressant medications or prefer alternatives.
These treatments include electroconvulsive therapy (ECT) and ketamine, with transcranial magnetic stimulation therapy (TMS) being one of the leading alternatives.
We’ve written an in-depth article about TMS therapy for depression.
The article answers the following questions for patients:
In contrast to antidepressant medications, TMS has milder and only brief side effects. Newer TMS protocols also provide a faster-acting solution, with many patients experiencing significant symptom reduction or complete relief after just one week of treatment.
At our Utah-based clinic, Cognitive FX, we offer a close alternative to the newly FDA-approved and revolutionary SAINT™ protocol of TMS. Of all the types of TMS available, this is the most targeted, safe, and effective protocol for patients with treatment-resistant depression.
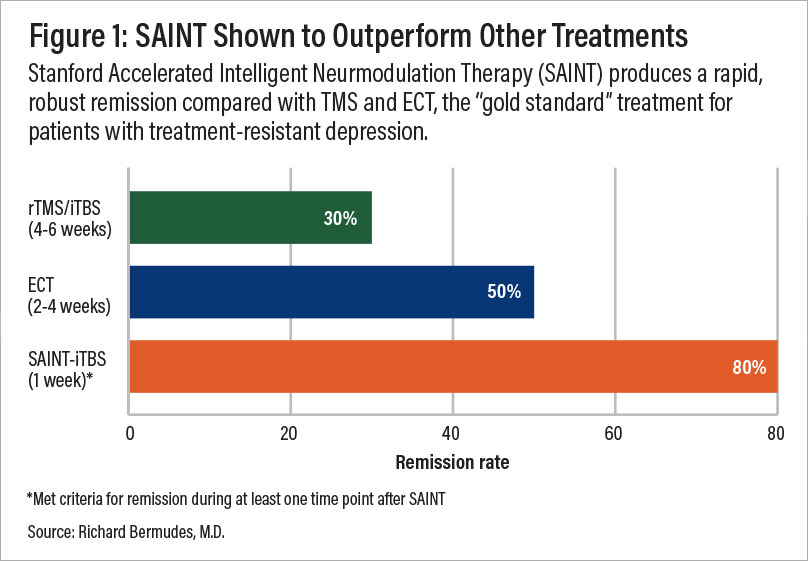
A comparison of remission rates for rTMS/iTBS, electroconvulsive therapy (ECT), and SAINT-iTBS.
The only difference between our treatment and SAINT™ (a trademark licensed to Stanford Medical) is our targeting method. Our target locations are determined by fMRI and our prescribing neuroscientist and physician, rather than their proprietary software.
| Accelerated fMRI - TMS | Magnus SAINT™ TMS | |
|---|---|---|
| FDA-Approved iTBS | ✔ | ✔ |
| FDA-Approved Neuronavigators | ✔ | ✔ |
| FDA-Approved Figure 8 Coils | ✔ | ✔ |
| Number of Treatment Days | 5 | 5 |
| Treatments per Day | 10 | 10 |
| Total Treatments | 50 | 50 |
| Number of TMS Pulses | Approx. 90,000 | 90,000 |
| Resting motor threshold pulse intensity | 90–120% | 90–120% |
| FDA-Approved Personalized DLPFC Targeting | ✘ | ✔ |
| Personalized DLPFC Targeting Assists Doctor in Target Location | ✔ | ✘ |
| Personalized E Field Coil orientation | ✔ | ✘ |
| Cost | $9,000 to $12,000 | $30,000+ |
This accelerated protocol of iTBS is:
To improve patient outcomes, we also include cognitive behavioral therapy (CBT) as a part of our treatment. When combined with the traditional method of TMS (rTMS), CBT improved response and remission rates by ~8% and ~19%, respectively. Additionally, CBT is likely to produce sustained improvement over time once treatment has concluded.
Our brain stimulation treatment is ideal for most patients with treatment-resistant depression. However, we do not treat patients under the age of 18 or over 65. Additionally, as a safety measure, we do not treat patients who have a history of seizures or who are currently actively suicidal and in need of crisis care.
Click here to learn more about receiving accelerated fMRI TMS therapy at Cognitive FX.
Flawed depression assessment and treatment: Many healthcare providers use a one-size-fits-all approach to treating depression, often immediately prescribing antidepressant medications without thoroughly assessing the individual factors contributing to each patient’s condition. This approach frequently leads to inadequate care and persistent symptoms.
Limitations of antidepressant medications: Traditional antidepressants, such as SSRIs, are effective for only about one-third of patients, and finding the right medication often requires a lengthy trial-and-error process. Even when effective, there's a high relapse rate after medication discontinuation, leading many patients to remain on medication long-term.
Importance of specialized care: For patients with prolonged or treatment-resistant depression, working with a provider who thoroughly understands their unique needs and offers personalized care is crucial. Psychologists, in particular, may offer a broader range of therapies and alternative treatments beyond medication.
Best types of psychotherapy for depression: Several types of psychotherapies have been developed specifically for treating depression. Overall, research shows that cognitive behavioral therapy (CBT) is the most effective in both short- and long-term outcomes, with a notable advantage in the long term.
TMS as an alternative treatment option: Transcranial Magnetic Stimulation (TMS) is a leading alternative for patients who have not responded well to traditional antidepressants. TMS offers faster results with fewer side effects, especially with newer protocols like accelerated fMRI-guided iTBS, which is more targeted and effective.

Dr. Spangler is a Clinical Psychologist with over 20 years of experience working in both clinical and academic settings. She earned her doctorate degree in Clinical Psychology at the University of Oregon followed by a Postdoctoral Research Fellowship in the Department of Psychiatry at the Stanford University School of Medicine. Dr. Spangler served as a Professor of Psychology at Brigham Young University for 15 years where she directed training in Cognitive Behavioral Therapy for the Clinical Psychology Doctoral Program, and conducted research on the etiology and treatment of depressive, anxiety, and eating disorders. She also served as a Visiting Professor in the Department of Psychiatry Cognitive Therapy Centre at Oxford University in England. Dr Spangler has authored over 60 publications and has lectured worldwide. She has received numerous awards for her collective work from the National Institute of Mental Health, the American Psychological Association, the International Association for Cognitive Psychotherapy, the Association for Behavioral and Cognitive Therapies, the Beck Institute, and the National Association of Professional Women.

If you’re considering brain stimulation therapy for treating major depression, you may wish to understand the differences between repetitive transcranial magnetic stimulation (rTMS) and deep...

Clinics across the U.S. now offer TMS therapy specifically for anxiety. While early research suggests TMS may be an effective treatment, only a handful of studies have focused exclusively on anxiety.

A major challenge for patients with depression is that traditional antidepressant medications often take weeks or months to show results — if they work at all. This delay can be especially...

Anxious depression, clinically referred to as mixed anxiety depressive disorder (MADD), is a challenging condition to treat. Standard approaches — such as antidepressant medication and psychotherapy...

Transcranial magnetic stimulation (TMS) and neurofeedback are gaining popularity as non-invasive, medication-free options for treating depression—especially for people who haven’t found relief from ...

Transcranial magnetic stimulation (TMS) has been FDA-approved for treating major depressive disorder (MDD) since 2008 and is a well-established treatment option, especially for patients who haven’t...