In 2022, a reanalysis of the largest antidepressant study ever conducted found that traditional antidepressant medications only relieve depression symptoms in about one-third of patients who take them.
As a result, researchers and clinicians are focused on developing safe, evidence-based, and effective treatment alternatives. One of the most promising is transcranial magnetic stimulation (TMS) which is FDA-approved and has minimal side effects compared to antidepressant medications.
In this article, we compare and contrast today’s standard depression treatment options with various types of TMS including a new form of accelerated TMS that is producing the best short-term treatment outcomes to date. We’ll look at how each treatment compares in terms of effectiveness, side effects, length of treatment, and accessibility.
Below we cover the following:
Cognitive FX offers the most advanced, safe, and precise method of accelerated TMS for people with treatment-resistant depression. Click here to learn more and see if you’re a good fit for treatment.
Antidepressant Medications: Types, Effectiveness, and Considerations
Antidepressant medications are a category of prescription drugs used to treat moderate to severe depression. They are hypothesized to work by controlling a group of chemicals in the brain called neurotransmitters. These chemicals carry messages between cells in the brain and the rest of the body and are essential for many bodily functions.
Different medications aim to affect neurotransmitters in slightly different ways. The most common types of antidepressant medications include:
- Selective serotonin reuptake inhibitors (SSRIs): SSRIs aim to increase the level of a chemical called serotonin in the brain. They’re often the first option primary care doctors prescribe because they generally cause fewer side effects. Examples include fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft), citalopram (Celexa), and escitalopram (Lexapro).
- Serotonin and norepinephrine reuptake inhibitors (SNRIs): In addition to serotonin, SNRIs aim to increase the levels of another chemical called norepinephrine. Examples include duloxetine (Cymbalta, Drizalma Sprinkle), venlafaxine (Effexor XR), desvenlafaxine (Pristiq), and levomilnacipran (Fetzima).
- Atypical antidepressants: These antidepressants don’t fit into any other category. Examples include trazodone, mirtazapine (Remeron), vortioxetine (Trintellix), vilazodone (Viibryd), and bupropion (Forfivo XL, Wellbutrin SR, others).
- Tricyclic antidepressants (TCAs): Similarly to SNRIs, these antidepressants aim to increase the levels of serotonin and norepinephrine. However, they also aim to affect other chemical messengers, which can lead to various side effects and have been generally replaced by SSRIs and SNRIs. They’re typically only prescribed for patients who have tried other antidepressants without improvement. Examples include imipramine, nortriptyline (Pamelor), amitriptyline, doxepin, and desipramine (Norpramin).
- Monoamine oxidase inhibitors (MAOIs). MAOIs are usually prescribed as a last resort when other medicines haven't worked, but they’re associated with serious side effects. In addition, using an MAOI requires patients to follow a strict diet due to interactions with foods that contain tyramine (such as certain cheeses, pickles, and wine) and some medicines (such as some painkillers, decongestants, and certain herbal supplements). Also, these medicines can't be combined with SSRIs or medicines that aim to increase serotonin. Examples include tranylcypromine (Parnate), phenelzine (Nardil), and isocarboxazid (Marplan).
2022 Study Finds Antidepressants Far Less Effective Than Previously Thought
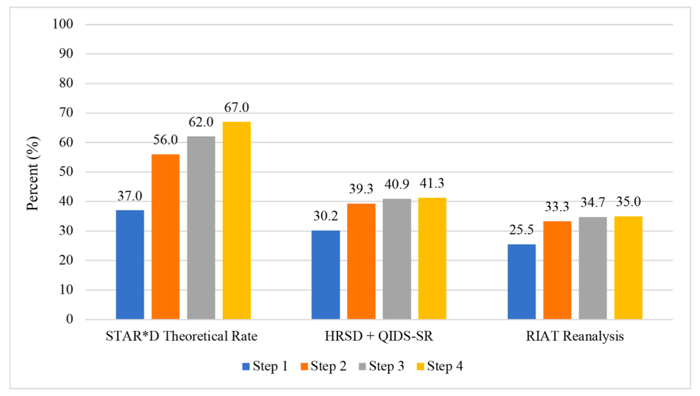
In 2006, the largest and most expensive prospective antidepressant trial ever conducted — the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study — reported that the theoretical cumulative remission rate after four antidepressant therapies was 67% in adults with major depressive disorder (MDD).
In the study, patients began with one type of antidepressant. If it was ineffective, they could try up to three additional types of antidepressants, stopping at whichever step was successful. Of the patients in their study who received the fourth antidepressant medication, they reported 67% of them were in remission (i.e., they no longer had significant depression symptoms and could resume daily activities as normal). These were impressive and encouraging outcomes.
However, a 2022 reanalysis of the STAR*D study found numerous scientific errors that inflated the positive outcomes. Specifically, the remission rate after four antidepressant therapies was only 35%.
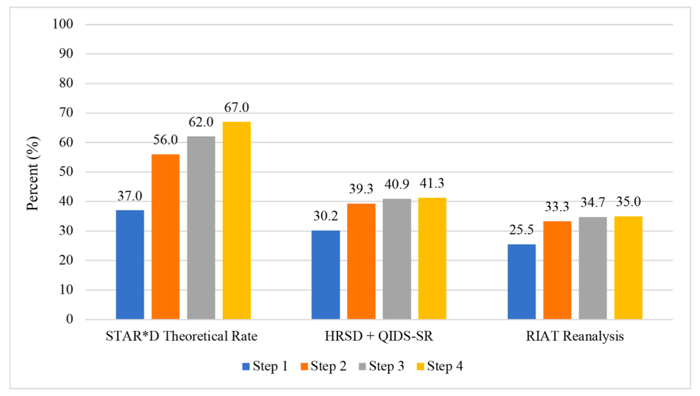
Source: National Institute of Health
This means that only about one-third of patients in the study achieved remission after trying four different antidepressant medications. Furthermore, among patients whose symptoms persisted after two types of antidepressant medications failed, less than 2% experienced success with a third or fourth medication.
With so few people responding to a third or fourth type of antidepressant medication, doctors and patients need to weigh the risks and side effects of taking additional medications past a second unsuccessful treatment. At this stage, patients will likely benefit more from seeking other treatment options.
Additional Challenges and Considerations
Predicting which patients will improve on antidepressants has been challenging. Some genetic screening tests can be used to suggest how efficiently the patient’s body will metabolize the drug and assess possible adverse reactions, but these tests do not indicate effectiveness. Patients still need to try each medication for a few weeks to months to determine if it can help or not, with the risk of developing unwanted side effects, such as headaches, digestive problems, and brain fog. It can take time and patience to test multiple medications all of which may not provide much benefit. In the meantime, these side effects may significantly impact the patient’s quality of life and well-being, especially if patients have other health conditions.
Furthermore, patients may find it difficult to stop taking antidepressants, as the dose must be gradually reduced over several weeks as the medication is being discontinued. If patients decide to stop abruptly, they are likely to experience severe side effects such as problems sleeping, nausea, and headaches.
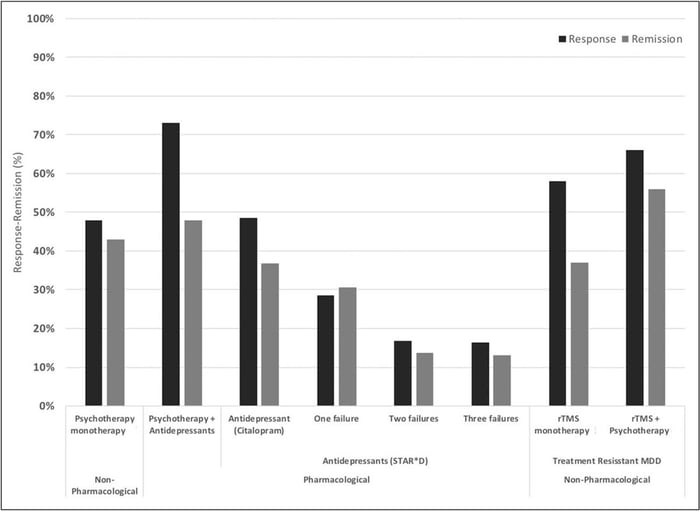
Research shows that combining antidepressant medications with some forms of psychotherapy can improve patient outcomes. However, with some forms of psychotherapy such as cognitive behavioral therapy (CBT), it is not necessarily the case that adding medication to CBT has added benefits compared to CBT alone.
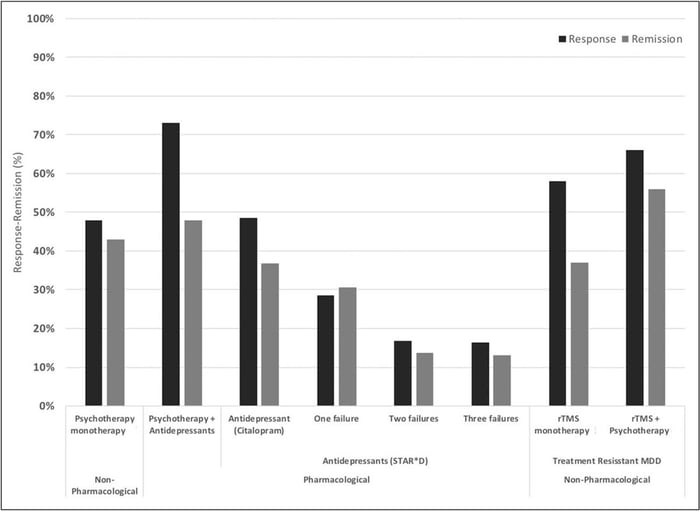
Response and remission rates of various monotherapeutic and combinatory antidepressant treatments based on the largest studies and datasets available. [Source]
Psychotherapy: Types and Effectiveness
Besides antidepressant medication, psychotherapy (also known as talk therapy) plays a key role in treating depression. In general terms, patients meet with a mental health professional, such as a psychology or psychiatry specialist, to discuss and find ways to cope with their symptoms, process difficult experiences, change thinking patterns, and gain a better understanding of their depression.
Skilled therapists can work with depressed patients to:
- Pinpoint the life problems that contribute to their depression and help them understand which aspects of those problems they may be able to solve or improve.
- Set realistic goals for the future to enable them to enhance their mental and emotional well-being.
- Identify and modify negative or distorted thinking patterns and content that contribute to feelings of hopelessness and sadness.
- Modify how thoughts are processed.
- Nurture a more positive outlook on life.
- Help them regain a sense of control over their life.
Several well-tested types of psychotherapy have been developed specifically for treating depression. These include:
- Cognitive behavioral therapy (CBT) for depression: CBT teaches patients how to identify and evaluate problematic thoughts, feelings, and behaviors associated with their depression, and modify both the content and the way thoughts are processed. It provides various strategies to cope with symptoms, such as helping patients identify and re-engage in activities they have enjoyed in the past. The goal is to help patients develop healthier thinking patterns and behaviors and move toward their goals leading to improved mood, emotional regulation, and overall functioning.
- Behavioral therapy (BT) for depression: In contrast to CBT, which focuses on both thoughts and behaviors, behavioral therapy focuses only on changing behaviors and environmental factors that contribute to a patient’s depression. Also known as “behavioral activation,” BT for depression encourages patients to participate in activities that are enjoyable and rewarding to combat the withdrawal and inactivity typical of depression.
- Interpersonal therapy (IPT): IPT aims to improve the patient’s relationships with others (friends, family members, etc.) by using strategies to communicate emotions and needs. It also focuses on helping patients adapt to social role transitions. As relationships with others improve and patients adapt better to their social roles, the depressive symptoms can subside, and the patient can experience improved functioning in multiple areas of life.
Cognitive Behavioral Therapy Is the Most Researched Type of Psychotherapy for Depression and Produces the Best Long-Term Outcomes
In comparison to other types of psychotherapy, CBT has far more scientific and empirical support for treating depression, including a significantly greater number of randomized controlled trials supporting its efficacy. Most meta-analyses comparing different types of psychotherapy for depression indicate that CBT outperforms others, in both the short-term and particularly in the long term (e.g., 6 months to 1-year post-treatment). That is, once treatment is concluded, the beneficial effects of CBT are sustained over time. In contrast, the benefits of other forms of psychotherapy and medications are not as durable, with patients often experiencing relapses of depression once these treatments conclude.
Overall, research shows that CBT is superior to other psychotherapies and medication for depression in both short- and long-term outcomes, with a notable advantage in the long term. The response rate to CBT across studies ranges from 61%–87% with large effect sizes.
It’s important to note that while CBT can be fast-acting for some patients, in general, CBT takes time (weeks or months) to achieve full remission of depression. This is why faster-acting treatment alternatives such as TMS, discussed next, are also helpful and needed.
Transcranial Magnetic Stimulation: How It Works, Types, and Effectiveness
The treatments described above can help many patients with major depression, but there is still a large proportion who do not benefit from either antidepressant medications or psychotherapy.
For these patients, transcranial magnetic stimulation (TMS) is an alternative option. TMS is a noninvasive brain stimulation procedure that applies a magnetic pulse to the brain that induces neural plasticity. The aim is to stimulate nerve cells in parts of the brain that are linked to depression.
TMS is regarded as an effective and safe stimulation technique. Common side effects include headaches, drowsiness, and a tingling sensation on the scalp and face. However, these are short-term and tend to go away soon after treatment.
TMS has been approved by the U.S. Food and Drug Administration (FDA) to be used in patients with treatment-resistant depression (i.e., several other treatment types have failed to alleviate their symptoms).
How TMS Works
TMS targets a specific area in the brain called the prefrontal cortex. To understand how TMS can be used for the treatment of depression, it first helps to understand what the prefrontal cortex does.
The prefrontal cortex is involved in many processes. Still, its main job is to regulate “executive functions” such as problem-solving and decision-making, helping us to weigh available information and respond to our environment to control our behavior. The prefrontal lobe allows you to understand the relationship between actions and consequences. Instead of behaving impulsively, the prefrontal cortex helps you decide what’s best for you in the long run. It also plays a significant role in personality development by helping you solidify your goals and values and allowing you to act consistently in different environments.
This region is one of the most consistently affected by depression. Low activity is especially pronounced in the left dorsolateral prefrontal cortex, which is responsible for positive feelings, including feeling rewarded for certain behaviors. In contrast, the right dorsolateral prefrontal cortex can become too active, exacerbating negative feelings.
As a result, depressed patients can have difficulty believing that goals are achievable or withdraw from desired rewards. When making decisions, patients can feel that the drawbacks outweigh the possible benefits or advantages. Some symptoms of depression, such as lack of motivation or a sense that nothing is worth doing, are linked directly to problems with the prefrontal cortex.
TMS therapy aims to restore normal levels of activity in the dorsolateral prefrontal cortex (DLPFC). In patients where the right side of the dorsolateral prefrontal cortex is too active, it’s also possible to use lower-frequency pulses to reduce activity in that area.
Types and Effectiveness Rates of TMS
Repetitive Transcranial Magnetic Stimulation
The first type of TMS developed is called repetitive transcranial magnetic stimulation (rTMS) and was first applied to treat depression in the mid-90s. This procedure involves repeated electromagnetic pulses delivered by a magnetic coil placed on the patient’s scalp to improve neuronal activity. Standard treatments using rTMS involve daily sessions, five days a week, with 20–30 sessions delivered over 4–6 weeks. Typically, patients start to see improvements after 2–4 weeks. However, some only see the benefits after treatment is completed. About 50% of patients respond well to treatment with over 30% showing complete remission.
Accelerated TMS
The main downside of rTMS is the amount of time it takes to complete treatment. Patients often struggle to complete a 6-week treatment plan due to family and work commitments. To solve this issue, researchers developed accelerated TMS. With this option, patients undergo multiple sessions per day and treatment lasts only a few days making it easier for patients to complete.
Studies show accelerated TMS is as safe as daily rTMS and potentially more effective. Patients receiving multiple sessions each day tend to experience improvements in symptoms faster than patients receiving daily sessions, and the effects are still visible months after their treatment.
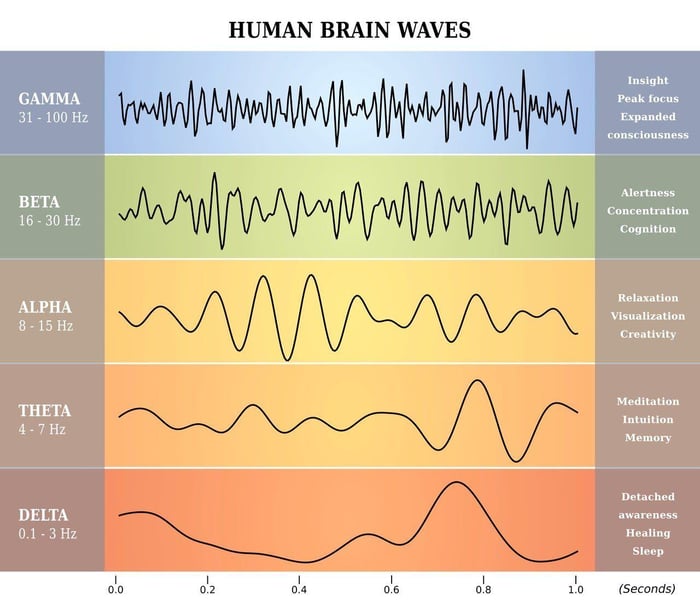
Intermittent Theta-Burst Stimulation (iTBS)
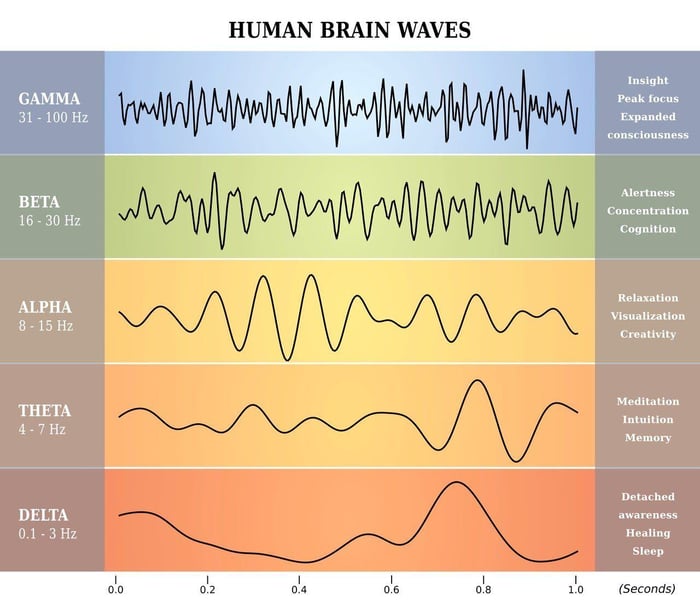
In 2018, the FDA approved a new version of accelerated TMS called Intermittent Theta-Burst Stimulation (iTBS). Theta waves are the frequencies the hippocampus uses to connect to other brain circuits and are utilized in memory formation, meditation, and certain phases of sleep. Theta burst stimulation also uses a different magnetic pulse (in triplets), delivering the treatment in three minutes (compared to 37 minutes in rTMS).
This method is safe and effective; many patients experience improvements shortly after starting treatment. In addition, patients also noticed a decrease in suicidal ideation, suggesting that iTBS could be an option to rapidly treat patients at high risk of suicide.
Accelerated fMRI-Guided iTBS (SAINT™ TMS)
In the standard rTMS and iTBS protocols, the location to apply the coil is calculated based on triangulation between the patient’s nose, ears, and top of the head.
Coil placement involves measuring the scalp 5cm along the parasagittal plane anterior to the activation hotspot in the motor cortex. This method is easy to implement and requires no further equipment, but it does not account for variations in head size and shape or differences in brain organization between patients.
In addition, it relies heavily on how well technicians can find the right spot. Even missing the DLPFC by a few millimeters is enough to produce poorer results.
A much more accurate way involves using functional MRI and neuronavigation to determine exactly where the DLPFC is located in the brain. This method, developed by a team from Stanford University, is known as the SAINT™ protocol.
Stanford Intelligent Accelerated Neuromodulation Therapy (SAINT™) is a depression treatment approved by the FDA in September 2022.

A comparison of remission rates for rTMS/iTBS, electroconvulsive therapy (ECT), and SAINT-iTBS.
SAINT treatment involves 10 sessions per day over 5 days for 50 sessions total. Following this protocol significantly reduced depressive symptoms and suicidal ideation within 5 days, without negative side effects. In a double-blind randomized controlled trial, about 85.7% of patients responded to the treatment (meaning they met prespecified criteria for reduced depressive symptoms) and around 78.6% met the remission criterion. All the individuals in the study had treatment-resistant depression and had failed at least two other depression treatments. At the one-month mark, 60% were still in remission.
The speed with which SAINT-iTBS can achieve high response and remission rates, combined with minimal side effects, makes it one of the best fact-acting treatments available today. With that said, there is limited data on the durability of these outcomes and how well they hold up over time. Some patients may see lasting remission or symptom reduction, while others may need follow-up treatments to maintain the effectiveness. As such, combining TMS with CBT, as we do at our clinic, is likely to produce the best results for patients. SAINT-iTBS can be used to get quick relief, while CBT can support long-term outcomes.
Summary: How These Treatments Compare
| |
Antidepressant Medication
|
Cognitive Behavioral Therapy (CBT)
|
Transcranial Magnetic Stimulation (TMS)
|
|
Effectiveness
|
~35% of patients achieve remission (this may involve trying up to four different antidepressant medications).
|
Response rate to CBT across studies ranges from 61%–87% with large effect sizes.
|
rTMS procedures helped ~30% of patients achieve remission. With the latest TMS protocols (SAINT-iTBS), randomized controlled trials have found that ~60% of participants were in remission 4 weeks after treatment.
|
|
Side Effects
|
Side effects are common and may include nausea, brain fog, loss of appetite and libido, sleeping problems, emotional numbing, headaches, and others.
|
No side effects.
|
Side effects are short-lived and minor. They include headaches, drowsiness, and a tingling sensation in the scalp shortly after treatment. Seizures can happen but are extremely rare (1 in 40,000 sessions).
|
|
Length of Treatment
|
Varies greatly.
It's usually recommended that patients take antidepressants for at least six months after they start to feel better. Some patients with recurrent symptoms may be advised to take these meds for a long time.
|
CBT treatment protocols for depression range from 8–20 weeks of once-per-week hourly sessions.
|
rTMS treatments are conducted over 4–6 weeks once per day, but accelerated TMS has reduced treatment time to just 5 days of 10 administrations per day.
|
|
Relapse Rate (Frequency of depression symptoms returning)
|
Relapse rate for antidepressant medications at 1 year after discontinuation ranges from 60%–76%.
|
Relapse rate for CBT 1 year after treatment discontinuation ranges from 26%–31%.
|
Relapse rate for SAINT-iTBS is estimated to be up to 50% 6 months after treatment discontinuation.
|
|
Accessibility
|
Easy, typically family doctors can prescribe these drugs.
|
Easy, but it may take some time to find a well-trained, certified CBT therapist.
|
rTMS is relatively easy to access. Newer forms of TMS, such as fMRI-guided iTBS, are only offered by a few healthcare providers in the US.
|
Receiving Accelerated fMRI-Guided TMS at Cognitive FX
Our clinic in Provo, Utah, provides an alternative to SAINT™ TMS that offers the same precision of personalized treatment targeting, combined with FDA-approved theta burst stimulation at a significantly lower cost. This approach delivers the same core elements that make SAINT so revolutionary.
The only difference between our treatment and SAINT™ (a trademark licensed to Stanford Medical) is our targeting method. Our target locations are determined by fMRI and our prescribing neuroscientist and physician, rather than their proprietary software.
This accelerated protocol of TMS is:
- Safe: Widely tolerated and associated with mild, short-lasting side effects.
- Precise: fMRI ensures that the treatment target area is precisely located for each patient, accounting for variations in head size and shape. Neuronavigation ensures the magnetic coil is placed over that exact spot for every treatment session.
- Fast: Treatment courses are reduced to a single week, making it easier to complete alongside life and work commitments (compared to 4 to 6 weeks of standard TMS and accelerated TMS protocols).
To improve patient outcomes, we also include cognitive behavioral therapy (CBT) as a part of our treatment. When combined with the traditional method of TMS (rTMS), CBT improved response and remission rates by ~8% and ~19%, respectively. Additionally, CBT is likely to produce sustained improvement over time once treatment has concluded.
Our brain stimulation treatment is ideal for most patients with treatment-resistant depression. However, we do not treat patients under the age of 18 or over 65. Additionally, as a safety measure, we do not treat patients who have a history of seizures or who are currently actively suicidal and in need of crisis care.
Click here to learn more about receiving accelerated fMRI TMS therapy at Cognitive FX.
Cited Research