Antidepressant medication is often the first treatment offered to patients with major depressive disorder. However, these medications are not as effective as once thought and frequently trigger unwanted side effects.
A 2022 reanalysis of the largest antidepressant study ever conducted found that traditional antidepressant medications only relieve symptoms in about one-third of patients who take them. To compound this problem, doctors often continue to prescribe increasingly stronger antidepressants to patients who don’t immediately respond to their first or second medication. These come with a higher risk of side effects, and data suggest that less than 2% of patients have success with a third or fourth medication.
There is a great need for evidence-based treatment alternatives, especially for patients who have tried and failed multiple medications. In this article, we present some of the leading alternative therapies for people with treatment-resistant depression. We discuss success rates and side effects for each treatment to help you weigh which option might be worth considering for yourself or a loved one.
We cover:
Transcranial Magnetic Stimulation (TMS)
Despite having been around for over 20 years (and FDA-approved for treating depression since 2008), TMS is a lesser-known treatment option for depression. However, it is considered one of the safest and most effective depression treatments available today.
It also has relatively mild side effects compared to antidepressant medications. Common side effects include headaches, drowsiness, and a tingling sensation on the scalp and face. These are short-term and tend to go away soon after treatment.
The Effectiveness of TMS
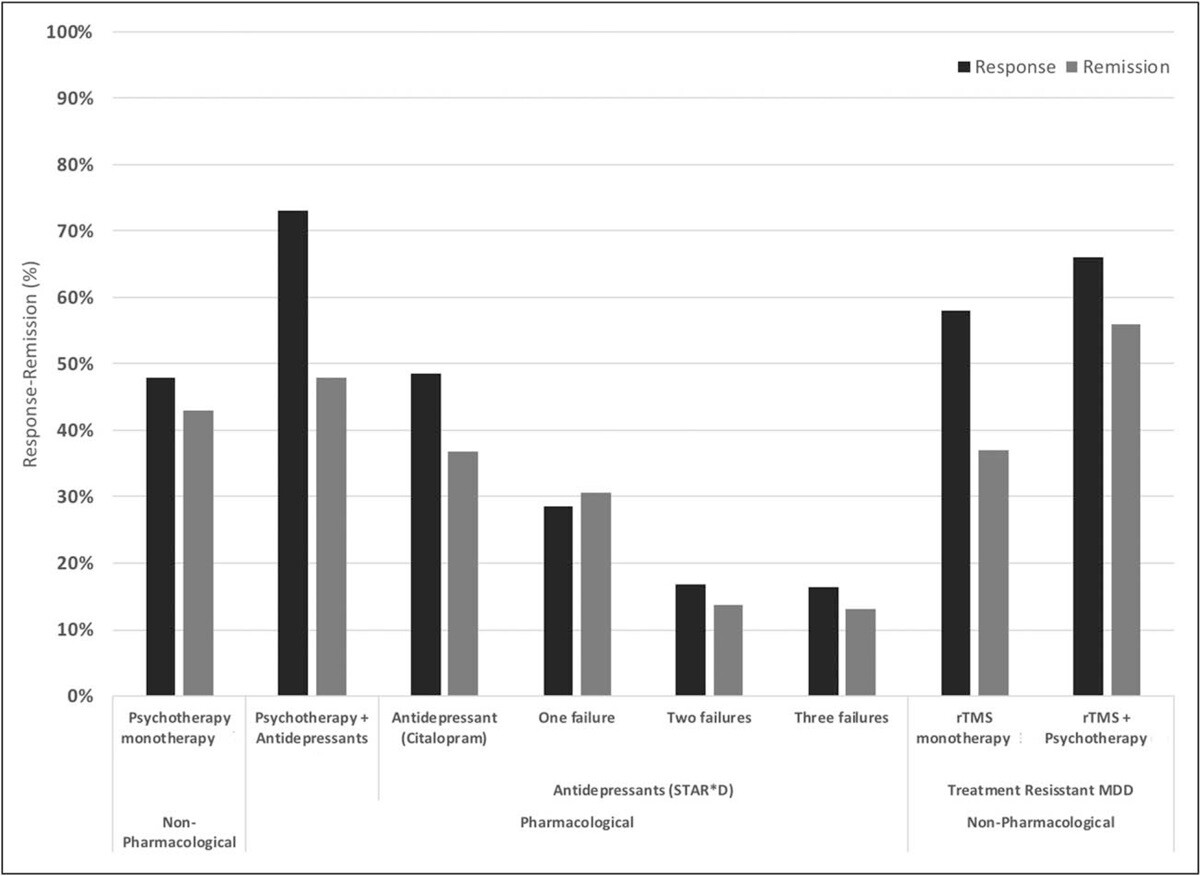
The original form of TMS, repetitive transcranial magnetic stimulation (rTMS), has been shown to improve depression symptoms in about 50% of patients, with over 30% achieving remission (i.e., a significant decrease in or disappearance of signs and symptoms of depression). When combined with psychotherapy, success rates are even more impressive with response and remission rates of ~66% and ~55% respectively.
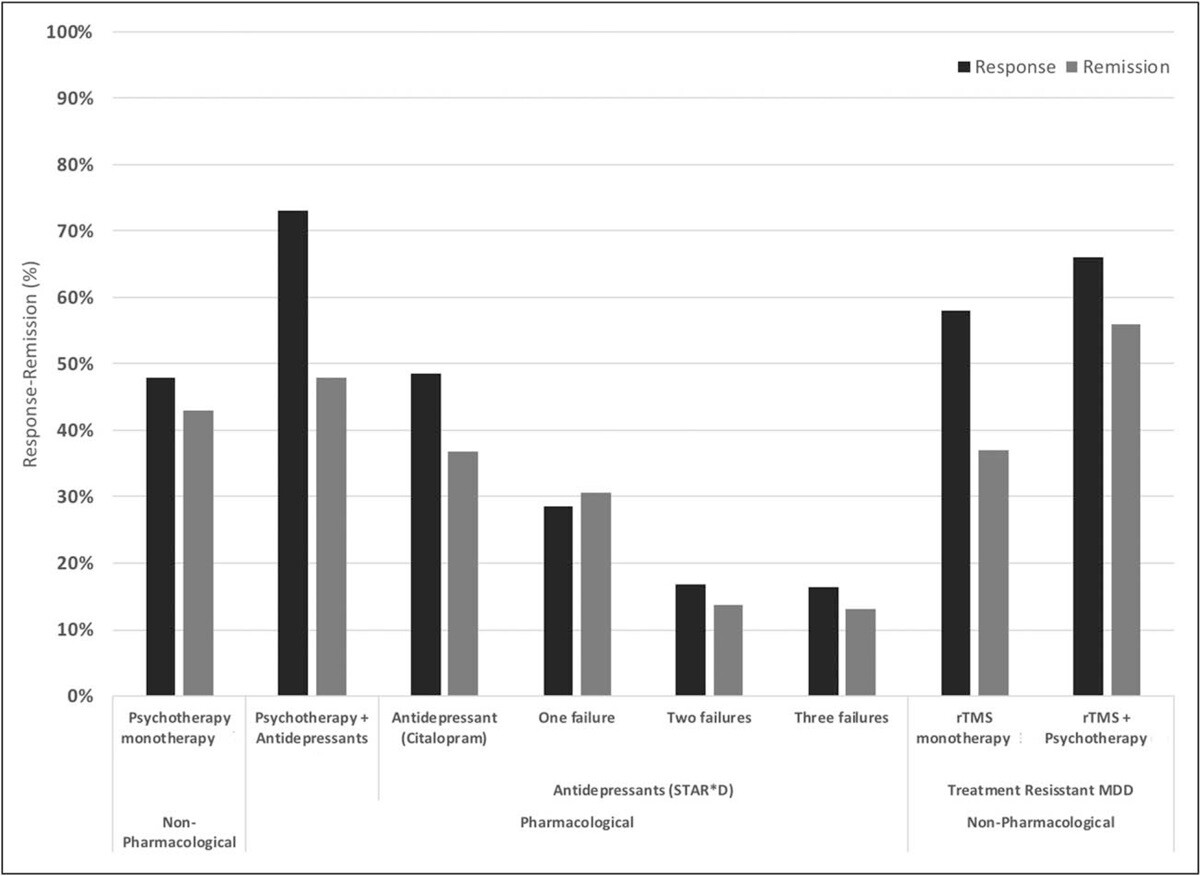
Response and remission rates of various monotherapeutic and combinatory antidepressant treatments based on the largest studies and datasets available. [Source]
Compared to antidepressant medications, these are already significant improvements. However, a new form of accelerated TMS, the SAINT™ protocol (FDA-approved in 2022), is producing even better outcomes.
In a double-blind randomized controlled trial, about 85.7% of patients responded to the SAINT-iTBS treatment (meaning they met pre-specified criteria for reduced depressive symptoms) and around 78.6% met the remission criterion. All the individuals in the study had treatment-resistant depression and had failed at least two other depression treatments. One month after treatment, 60% were still in remission.
The speed with which SAINT™ can achieve high response and remission rates, combined with minimal side effects, makes it one of the best fast-acting treatments available today. With that said, there is limited data on the durability of these outcomes and how well they hold up over time. Some patients may see lasting remission or symptom reduction, while others may need periodic follow-up treatments to maintain the effectiveness. As such, combining TMS with cognitive behavioral therapy (CBT), which has been shown to have particularly strong long-term outcomes as we’ll discuss below, is likely to produce the best results for patients.
How TMS Works
TMS is a noninvasive procedure that uses magnetic pulses to restore normal activity levels in a part of the brain called the dorsolateral prefrontal cortex (DLPFC) which is consistently affected by depression and other mood disorders. During a TMS session, an electromagnetic coil is placed over the patient’s head directly above the DLPFC, and pulses are applied at specific intervals to stimulate nerve cells in that area.
Standard treatments using rTMS involve daily sessions, five days a week, with 20-30 sessions delivered over 4-6 weeks. Typically, patients start to see improvements after 2-4 weeks. However, some only see the benefits after treatment is completed.
The main downside of rTMS is the time it takes to complete treatment. Patients often struggle to complete a 6-week treatment plan due to family and work commitments, which led researchers to develop accelerated TMS. With this option, patients undergo multiple sessions per day and treatment lasts just one week making it easier for patients to complete.
Studies show accelerated TMS is as safe as daily rTMS and potentially more effective. Patients receiving multiple sessions each day tend to experience improvements in symptoms faster than patients receiving daily sessions, and the effects are still visible months after their treatment.
Advances in TMS Are Producing the Best Outcomes to Date
In 2018, the FDA approved a new version of accelerated TMS called Intermittent Theta-Burst Stimulation (iTBS). Theta waves are the frequencies the hippocampus uses to connect to other brain circuits and are utilized in memory formation, meditation, and certain phases of sleep. Theta burst stimulation uses a different magnetic pulse (in triplets) and delivers the treatment in three minutes (compared to 37 minutes in rTMS).
Many patients experience improvements shortly after starting treatment. In addition, patients also noticed a decrease in suicidal ideation, suggesting that iTBS could be an option to rapidly treat patients at high risk of suicide.

The SAINT™ protocol, mentioned above, uses iTBS in coordination with functional MRI and neuronavigation for precision coil placement over the exact section of the brain that TMS targets. This is an important advancement.
In the standard rTMS and iTBS protocols, the location to apply the coil is calculated based on taking manual measurements between the patient’s nose, ears, and top of the head. However, due to variations in head size and shape, or differences in brain organization between patients, studies have found this method of coil placement can be imprecise and lead to less consistent outcomes for patients.
By using fMRI and neuronavigation, practitioners can ensure that the magnetic coil is placed precisely over the DLPFC for each individual patient. This is now regarded as the “gold standard” treatment for treatment-resistant depression.

A comparison of remission rates for rTMS/iTBS, electroconvulsive therapy (ECT), and SAINT-iTBS.
Receiving Accelerated fMRI-Guided TMS Treatment for Depression at Cognitive FX
Our clinic in Provo, Utah, provides an alternative to SAINT™ TMS that offers the same precision of personalized treatment targeting, combined with FDA-approved theta burst stimulation at a significantly lower cost. This approach delivers the same core elements that make SAINT so revolutionary.
The only difference between our treatment and SAINT™ (a trademark licensed to Stanford Medical) is our targeting method. Our target locations are determined by fMRI and our prescribing neuroscientist and physician, rather than their proprietary software.
This accelerated protocol of iTBS is:
- Safe: Widely tolerated and associated with mild, short-lasting side effects.
- Precise: fMRI ensures that the treatment target area is precisely located for each patient, accounting for variations in head size and shape. Neuronavigation ensures the magnetic coil is placed over that exact spot for every treatment session.
- Fast: Treatment courses are reduced to a single week, making it easier to complete alongside life and work commitments (compared to 4 to 6 weeks of standard TMS and accelerated TMS protocols).
To improve patient outcomes, we also include cognitive behavioral therapy (CBT) as a part of our treatment. When combined with the traditional method of TMS (rTMS), CBT improved response and remission rates by ~8% and ~19%, respectively. Additionally, CBT is likely to produce sustained improvement over time once treatment has concluded.
Our brain stimulation treatment is ideal for most patients with treatment-resistant depression. However, we do not treat patients under the age of 18 or over 65. Additionally, as a safety measure, we do not treat patients who have a history of seizures or who are currently actively suicidal and in need of crisis care.
Click here to learn more about receiving accelerated fMRI TMS therapy at Cognitive FX.
Electroconvulsive Therapy (ECT)
Electroconvulsive therapy (ECT) is another FDA-approved treatment that involves sending an electric current through the patient’s brain while they’re under general anesthesia. Typically, ECT is applied 2-3 times per week and acute courses can range between 6-18 total sessions. It can be done as an inpatient or outpatient procedure. The aim is to cause a seizure, which in turn triggers changes in the brain that can reverse symptoms of depression, especially in patients with treatment-resistant depression and bipolar disorder.
ECT is associated with several side effects, including loss of memory and other cognitive issues, as well as headaches, nausea, dizziness, muscle pain, insomnia, high blood pressure, and heart problems.
Despite the worrying side effects, ECT can be beneficial for some patients and can produce better results than antidepressant medication. In a large-scale study, over 50% of patients experienced improvements during the first week. Overall, almost 80% of patients responded to ECT sessions and 65% reached remission after 4 weeks.
As a general rule, patients who previously failed to experience improvements after trying multiple antidepressant medication trials are less likely to respond to ECT treatment compared to patients not resistant to medication.
Ketamine
Ketamine is a type of anesthetic drug used to treat patients with treatment-resistant depression. However, shortly after it received approval from the FDA, they warned healthcare providers about potential risks for patients. At the moment, patients need to be closely followed by a healthcare professional because ketamine is a dissociative drug, which means patients can feel disconnected from reality and engage in dangerous and life-threatening behaviors. In addition, patients with a history of severe mental illness or substance use should not take this drug.
Ketamine’s antidepressant properties are hypothesized to work by inhibiting the activity of a chemical in the brain called glutamate. The problem is that glutamate is also essential for many cognitive functions and inhibiting it may lead patients to experience cognitive impairments. Patients need to decide if the benefits outweigh these risks before starting a ketamine treatment. (TMS, in contrast, does not have this downside. Brain stimulation can improve the function of glutamate and other neurotransmitters and promote better brain function.)
Side effects of ketamine can be severe and include dissociation, intoxication, sedation, high blood pressure, dizziness, headache, blurred vision, anxiety, nausea, and vomiting.
On the plus side, ketamine has proven very effective in offering rapid relief from depression symptoms. Multiple clinical trials showed that ketamine is extremely fast-acting compared with traditional antidepressants and can relieve depressive symptoms, including suicidal ideation, for a period that can last days or weeks. Around 60% of patients experienced the benefits of ketamine up to 3 days after a single treatment and about 40% still maintained their response one month later. However, after six months and multiple ketamine treatments, only 26% of patients were still responding and 15% were symptom-free and in remission.
Psychotherapy (Talk Therapy)
While psychotherapy is commonly prescribed in combination with antidepressant medications, it can also be used on its own as an alternative to medication. It involves meeting with a mental health professional, such as a psychology or psychiatry specialist, to discuss and find ways to cope with their symptoms, process difficult experiences, change thinking patterns, and gain a better understanding of their depression.
Three well-studied types of psychotherapy have been developed specifically for the treatment of depression.
Cognitive Behavioral Therapy (CBT) for Depression
Cognitive Behavioral Therapy (CBT) is the most well-researched type of psychotherapy for depressed patients, with far more scientific and empirical support compared to other psychotherapies, and a significantly greater number of randomized controlled trials.
CBT teaches patients how to identify and evaluate negative thoughts, feelings, and behaviors associated with their depression. It provides different strategies to cope with symptoms, such as helping patients identify and re-engage in activities they have enjoyed in the past. The goal is to help patients develop healthier thinking patterns, change cognitive processing, and engage in goal-directed behaviors, leading to improved mood, emotional regulation, and overall functioning.
CBT is often cited as the most effective form of psychotherapy for depression. Overall, research shows that CBT is superior to other psychotherapies and medication for depression in both short- and long-term outcomes, with a notable advantage in the long term. The response rate to CBT across studies ranges from 61%–87% with large effect sizes.
Behavioral Therapy (BT) for Depression
Behavioral therapy (BT) for depression, also known as “behavioral activation,” is considered a subset of cognitive behavioral therapy (CBT). As the name suggests, behavioral therapy focuses solely on the behavioral aspect of CBT, leaving the cognitive part out.
BT has the advantage of being more simplified, emphasizing getting patients moving and active, which can have significant short-term benefits in helping people feel better. However, BT misses out on the cognitive aspects that are important for overall outcomes.
The cognitive components of CBT, which address thinking patterns and cognitive processing, are most linked to the sustained effects of therapy. Without these, BT is less likely to provide the lasting change and long-term improvement that CBT offers.
Interpersonal Therapy (IPT)
It’s common for patients with depression to experience problems with their relationships and social roles. Interpersonal Therapy (IPT) helps patients recognize how life events, such as arguments with family members or grief, can affect their mood and emotional well-being. The goal is to help these patients learn to communicate better with others, address relationship issues that contribute to their depression, and improve social role transitions.
While results are not immediate and patients may feel uncomfortable addressing difficult issues during their sessions, studies show that IPT can be effective in treating depression, particularly when used in combination with antidepressant medication.
Non-Medical Alternatives to Consider
In addition to alternative first-line treatments such as those we’ve discussed so far, patients may benefit from various wellness products, services, and lifestyle changes. However, these should not be seen as a stand-alone treatment for your depression. They’re complementary aspects that can contribute to relieving depression alongside primary treatments.
Engage in Regular Physical Exercise
It’s not uncommon for patients with depression to feel constantly tired and low on energy. For these patients, engaging in regular exercise may be the last thing on their minds, but it can be helpful.
Beyond its numerous physical health benefits, such as lowering blood pressure, regular exercise also positively impacts emotional and psychological well-being. It can elevate mood, reduce anxiety, and help maintain improvements in depression and anxiety symptoms over time.
From a physiological perspective, regular physical activity enhances blood flow and stimulates the release of endorphins in the brain. Exercise also triggers the release of important neurochemicals including one called brain-derived neurotrophic factor (BDNF), which helps nerve cells communicate with each other and improves brain function.
Any type of exercise can be beneficial, from organized sports to gardening and walking. It can be hard to start, especially if patients haven’t exercised in a while, but they can start with short sessions and gradually increase difficulty.
It’s important to understand that although exercise can help patients with depression, the benefits are not instant. Patients should start to feel better a few weeks after starting to exercise regularly, but it’s a long-term solution, not a one-time fix. For this reason, it’s important to pick an activity you can sustain over time.
Practice Mindfulness
Mindfulness is known to help with stress, anxiety and depression. These exercises help patients with depression focus on the present instead of ruminating about the past or worrying about the future. This way, patients can control their mood better and experience fewer symptoms of depression. Crucially, patients learn to experience sadness and worry without letting these feelings consume all their thoughts.
As described earlier, some types of psychotherapy rely on mindfulness to help patients with depression. But it’s not just MBCT with the help of a therapist that can help. Practicing mindful exercises at home can be beneficial too, reducing anxiety and depressive symptoms. Crucially, these exercises also lower the risk of falling back into depression once patients achieve remission. Patients experience this wide range of benefits because mindfulness practice improves blood circulation and triggers changes in the brain in areas involved in regulating mood.
Follow a Healthy Diet
Bad dietary habits are known to contribute to depression. A dietary pattern characterized by a high consumption of red or processed meat, refined grains, sweets, high-fat dairy products, potatoes, and high-fat gravy, and a low intake of fruits and vegetables is associated with an increased risk of depression.
While there is no magic diet that can relieve depression, following a healthy diet can help patients as part of their overall treatment. For example, a study found that the symptoms of patients with moderate-to-severe depression improved when they received nutritional counseling sessions and ate a healthier diet for 12 weeks. Some patients experienced significant improvements and even achieved remission.
Several healthy options can be used as a guide for patients with depression, including the Mediterranean diet. Healthy diets include fruits and vegetables, unprocessed whole grains, seeds, and nuts, as well as some lean proteins like fish and yogurt. Items to avoid include foods high in salt and sugar, as well as highly processed fatty foods.
Choose Dietary Supplements Carefully
It is common for people to turn to dietary supplements to address health problems and support their overall health. However, it is important to understand that these products are not regulated by the FDA, so manufacturers are not required to prove their supplements' effectiveness or disclose their exact ingredients. Additionally, there is a lack of substantial scientific evidence supporting their use. Most studies involve a small number of participants and often fail to report side effects or long-term effects.
With that said, some of the most commonly used supplements for depression include:
- Omega-3 fatty acids: These can be taken as pills or by eating foods rich in these fatty acids, such as oily fish like salmon and sardines. Omega-3 fatty acids are essential for a healthy nervous system function and, at least in theory, should help patients regulate their mood. However, studies show conflicting evidence regarding the effectiveness of these supplements. In most cases, patients experienced some short-term benefits, but they didn't improve long-term remission rates.
- S-adenosylmethionine (SAMe): This compound is produced naturally in the body and is involved in the synthesis of neurotransmitters in the brain. However, similar to omega-3 fatty acids, results regarding its efficacy are contradictory. One study found a significant short-term effect similar to antidepressant medication, but others detected no effects.
- St. John's wort: This herb comes from a flower (Hypericum perforatum) and has been used to treat depression for centuries. St. John's wort is believed to regulate serotonin levels in the brain. Studies show that St. John’s wort can be as effective as SSRIs (selective serotonin reuptake inhibitors) for treating mild to moderate depression, but it can also have a series of side effects and must not be taken with several commonly prescribed drugs.
- Vitamin D: The brain has receptors for vitamin D in areas involved in regulating mood and this vitamin is also involved in the production of neurotransmitters. Studies suggested that vitamin D may benefit patients with depression, but only if they have low levels of this vitamin.
- Iron: The link between anemia and depression is well-known, and low levels of iron may aggravate depressive symptoms. Low iron changes dopamine metabolism and affects serotonin levels, both of which can result in mood changes. For patients with low levels of iron, supplementation may be beneficial to help with depressive symptoms.
- Prebiotics and probiotics: Some studies show that pre- and probiotics can help patients with depression. Even in patients who did not respond to antidepressant meds, there was a clear improvement in symptoms in those taking these products for 8 weeks. As these products are usually well tolerated and with no serious adverse effects, they could be a useful option for patients with depression.
Before taking dietary or herbal supplements, be sure to discuss them with your doctor. It’s also helpful to review the National Institute of Health website — specifically the section on complementary and alternative medicine. There you will find rigorous and unbiased research on everything from acupuncture, to specific herbal remedies, to yoga, and more.
Follow Healthy Sleep Patterns
Poor sleep and depression are closely connected. It’s common for patients with depression to start experiencing sleep disturbances. Poor sleep also makes it harder for patients to regulate their emotions which, in turn, leaves them vulnerable to depression.
Approximately 40% of people with insomnia have clinical depression and up to 90% of patients with depression experience bouts of insomnia. Sleep issues commonly associated with depression include difficulties falling asleep, frequently waking up during the night, and sleeping too much.
Implementing healthy sleep habits can help patients sleep better, boost their mood, and decrease some of their challenging depressive symptoms. Consider the following tips:
- Follow a consistent routine: Waking up and going to sleep at the same time every day (including holidays and weekends) consistently “teaches” the mind and body when it’s time to sleep.
- Nap carefully: If you’re not sleeping well at night, it may be tempting to nap during the day. Ideally, naps should be early in the afternoon and no longer than 20-30 minutes. These “power naps” can regulate emotions, reduce sleepiness, and increase performance. However, anything longer is likely to interfere with your ability to fall asleep at night.
- Avoid alcohol: Excessive drinking before bed makes it harder to fall asleep, and even moderate drinking is enough to disrupt the sleep cycle and shorten REM sleep.
- Get outside: Exposure to natural light — particularly first thing in the morning — regulates the body’s internal clock and gives powerful cues for when it’s time to be alert and when it’s time to sleep.
- Exercise regularly: As described earlier, engaging in regular exercises not only improves sleep quality but also decreases symptoms of depression.
Engage in Light Therapy
Another option to treat depression involves light therapy. This involves sitting close to a special light source every morning for at least 30 minutes. To use a light box, patients sit in front of the light or slightly off to the side. Patients shouldn’t look directly but need to keep their eyes open. As long as they’re near the light, patients are free to eat, read, watch television, or work on a computer.
This type of therapy is more suitable for patients with mild depression. Patients with severe cases should not try light therapy without seeking medical advice first. In addition, patients with bipolar disorder should consult a psychiatrist before trying light therapy. In rare cases, the light can trigger a manic episode.
Studies suggest that light therapy can help patients with depression by:
- Balancing the levels of serotonin in the brain (this chemical is believed to influence mood)
- Regulating sleep patterns and increasing sleep quality
- Increasing alertness and creativity
The effectiveness of light therapy is about the same as antidepressant medications or psychotherapy. For example, studies suggest that light therapy improves symptoms in about 50% to 60% of patients, which may increase considerably when combined with other treatments.
Key Takeaways
- While traditional antidepressant medications are often the first line of treatment for major depressive disorder, they’ve been found to only work for about one-third of patients.
- There is a great need for evidence-based treatment alternatives, especially for patients who do not respond to initial medications.
- TMS, ECT, and Ketamine are all FDA-approved alternatives for treating depression. However, ECT and ketamine are associated with more severe side effects than TMS and lower response rates than TMS.
- TMS — and particularly fMRI-guided theta burst stimulation — is one of the safest, fastest, and most effective treatments available for patients with treatment-resistant depression.
- While psychotherapy is commonly prescribed in combination with antidepressant medications, it can also be used on its own as an alternative to medication. Overall, research shows that CBT is superior to other psychotherapies and medication for depression in both short- and long-term outcomes, with a notable advantage in the long term.
- Additionally, various non-medical approaches, such as exercise, mindfulness, healthy diet, and sleep hygiene, can offer substantial benefits.
If you are interested in receiving accelerated fMRI TMS therapy at Cognitive FX, click here to learn more.
Cited Research