Is TMS Safe? Answers for Patients Considering TMS Therapy
If you’re considering transcranial magnetic stimulation (TMS) therapy, one of the first and most important questions you’re likely to ask is: “Is TMS safe?”

If you’re considering transcranial magnetic stimulation (TMS) therapy, you may be concerned about its side effects and whether the benefits outweigh any risks.
The short answer is yes — the potential benefits do outweigh the risks for many people. TMS for depression, for example, is associated with fewer and milder side effects than antidepressant medications, while being equally or more effective in reducing depression symptoms.
This article provides a comprehensive overview of potential side effects and risk factors for TMS. We cover:
Cognitive FX offers the most advanced, safe, and precise method of accelerated TMS for people with treatment-resistant depression. Click here to learn more and see if you’re a good fit for treatment.
In general, with TMS, patients either don’t experience any side effects or experience only mild ones, such as temporary scalp discomfort or headaches. This treatment option can boast this excellent side effect profile because — unlike medication, which can affect the entire body — TMS works by targeting a specific part of the brain responsible for regulating mood. It uses magnetic pulses to induce neural plasticity and aims to stimulate nerve cells in what’s called the dorsolateral prefrontal cortex (DLPFC).
In addition to mild side effects, TMS also has an impressive success rate. For example, when combined with psychotherapy, studies have shown the standard form of TMS (rTMS) has response and remission rates of ~66% and ~55%, respectively.
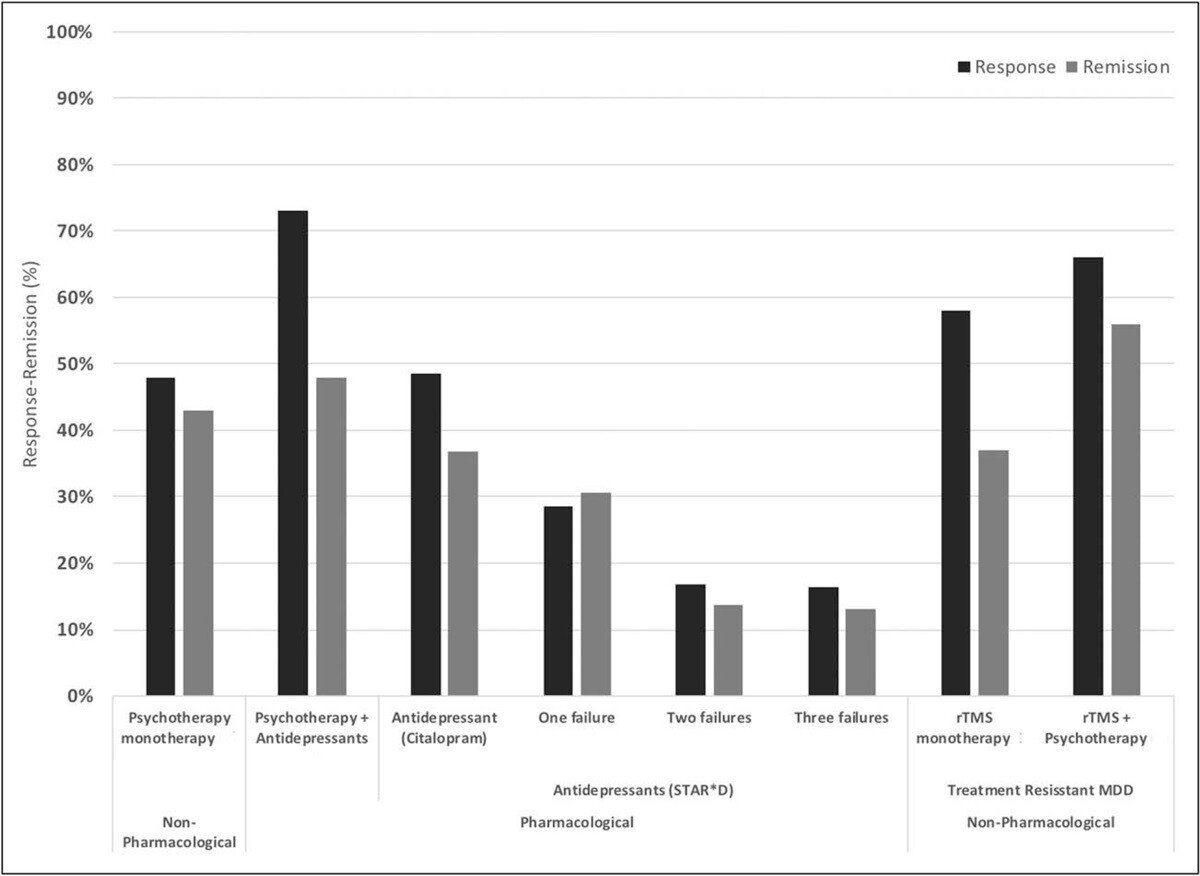
Response and remission rates of various monotherapeutic and combinatory antidepressant treatments based on the largest studies and datasets available. [Source]
New forms of accelerated TMS, such as the SAINT™ protocol (now approved by the US Food and Drug Administration), are producing even better outcomes. In a double-blind randomized controlled trial, about 85.7% of patients responded to the treatment (meaning they met prespecified criteria for reduced depressive symptoms) and around 78.6% met the remission criterion.
All of the individuals in the study had treatment-resistant depression and had failed at least two other depression treatments. At the one-month mark, 60% were still in remission.

A comparison of remission rates for rTMS/iTBS, electroconvulsive therapy (ECT), and SAINT-iTBS.
Based on these results, the potential benefits of TMS far outweigh the risks, particularly when medication and traditional therapy have fallen short.
Generally, TMS therapy doesn’t trigger significant patient discomfort and causes only mild side effects. In addition, patients don’t need anesthesia or sedation and can resume their normal activities immediately after each session. This ease of treatment and non-invasiveness are significant benefits for many patients.
The most common side effects of TMS include:
Mild headaches and localized pain are the most common side effects after a TMS session, affecting about one-third of patients during treatment. Occasionally patients may also experience toothache, earache, twitching facial muscles, and jaw pain, but these are less common. It’s unclear how TMS causes headaches, but the most likely explanation involves a trigeminal nerve reaction that can cause muscle in the head to contract. There is no indication that TMS can trigger migraines, even in patients with a history of this condition.
Advice for patients: Typically, these headaches are mild and rarely cause patients to stop their treatment. If you experience any headaches after your treatment, you can use over-the-counter painkillers such as ibuprofen or paracetamol to manage these side effects. In most cases, patients get used to the procedure and stop having headaches after a few sessions.
Another common side effect of TMS is scalp pain and discomfort (usually with a sensation of warmth) during the TMS procedure. Like headaches, this happens due to muscle contractions in the scalp and usually dissipates shortly after the session. In addition, patients get acclimatized as their body adapts to the procedure and this eventually stops happening.
Advice for patients: Again, you can use painkillers to manage the symptoms, if needed. In extreme cases, some of the treatment parameters can be adjusted to minimize discomfort during the initial sessions, such as placing the coil further away from the brain or changing the angle to ensure it doesn’t hit the trigeminal nerve or the scalp muscles that are causing the pain.
An uncommon side effect of TMS is an increased sensitivity to sound, likely triggered when TMS stimulates brain areas involved in auditory processing. Some patients become more aware of ambient noises or hear sounds more intensely than before treatment. This is only temporary and normal hearing returns soon after treatment. In rare cases, TMS can trigger tinnitus and hearing loss if patients undergo TMS sessions without ear plugs.
Advice for patients: Make sure you always wear ear protection during treatment. In case you experience any significant changes for a prolonged period, seek medical help to assess for hearing loss and tinnitus.
TMS can cause severe side effects, but it is extremely rare. However, it’s important to note that even these are usually short-lived and the patient recovers fully without any long-term consequences.
Some of these include:
The most serious possible side effect during TMS treatment is seizures, but it’s important to note that the risk is minimal for most patients. Estimates suggest that less than 3 patients experience a seizure per 100,000 sessions. Seizures are more likely in the initial sessions but can occur later in the treatment, particularly if there are clinical or medication changes.
Seizures can occur in any patient, but they’re more likely in patients with a previous history of seizures or suffering from neuropsychiatric diseases, including epilepsy, multiple sclerosis, traumatic brain injury, and Alzheimer’s disease, to name just a few. In addition, lack of sleep, excessive alcohol consumption, some prescription drugs, and high stress levels are also associated with a higher risk of seizures during TMS sessions.
Typically, patients experience a single isolated seizure that has no serious long-term consequences. There is no evidence that patients experience multiple seizures during TMS sessions.
Advice for patients: The best way to minimize the risk of experiencing a seizure is to look at all factors that may increase your risk of seizures, such as prescription medication and history of seizures. In conjunction with your healthcare provider, you can weigh the pros and cons and decide whether TMS is suitable for you.
Patients sometimes feel lightheadedness and faint during a TMS session due to anxiety and discomfort. This is a common reaction to some medical treatments and isn’t caused by the TMS procedure itself. Occasionally, symptoms may exhibit some behaviors that also occur during seizures, such as convulsions and rapid head movements.
Patients typically recover faster after a syncope than after a seizure.
Advice for patients: It’s impossible to determine when you’re going to faint during a treatment. If you start showing signs of distress which may cause fainting, you need to rely on your healthcare provider to terminate the TMS session and allow you to recover.
Some patients undergoing TMS therapy report unexpected emotional responses, including exaggerated mood swings and manic episodes. Studies show these mental health changes are extremely rare (less than 1% of cases) and occur especially in patients with bipolar disorder and taking antidepressant medication for major depressive disorder. In all cases, these psychiatric changes subsided shortly after the treatment and patients returned to normal.
It’s generally difficult to determine whether symptoms such as anxiety, sleep disturbances, and low mood are caused by the treatment or the major depression itself.
Advice for patients: If needed, you should seek medical care, where a psychiatry or psychology specialist can assess your mental health conditions.
While TMS is generally safe, certain situations can pose additional risks for patients, including:
One of the main contraindications for TMS is the presence of metallic implants (or other objects) in the brain close to where the coil needs to be placed. This includes, for example, cochlear implants, Internal Pulse Generators, medication pumps, aneurysm clips or coils, stents, or even bullet fragments. Patients with these cannot undergo TMS because the magnetic fields could malfunction the implanted devices. Braces and dental fillings are acceptable for treatment.
Under normal circumstances, the heating produced during a TMS session is negligible and poses no risk to the patient. However, TMS can overheat metal objects and cause irreversible damage to the brain. Low-conductivity plastic and titanium implants are less prone to heating up.
Eye makeup containing ferromagnetic particles may potentially cause facial pain during TMS due to local heating. While there are no studies that assess permanent makeup (e.g. for alopecia) or scalp tattoos, if they may contain ferromagnetic particles, that can interact with TMS’s magnetic field.
Certain medications are known to increase a patient's risk of seizures, and it was previously assumed that using these medications in combination with TMS would significantly elevate this risk. However, over the years, thousands of patients have undergone TMS sessions, many of whom were also taking prescription medications, and there is no evidence to suggest an increased risk of seizures beyond the risk already associated with TMS.
Nevertheless, if you’re currently on medication, it’s important to discuss this with your healthcare professional before starting TMS.
For patients taking drugs associated with a high risk of seizures, TMS should be performed with caution.
At our clinic, Cognitive FX, we offer a close alternative to the newly FDA-approved SAINT™ protocol which uses intermittent theta-burst brain stimulation (iTBS) in coordination with functional MRI and neuronavigation for precision coil placement over the exact section of the brain that TMS targets. Of all the types of TMS available, this is the most targeted, safe, and effective protocol for patients with treatment-resistant depression.
The only difference between our treatment and SAINT™ (a trademark licensed to Stanford Medical) is our targeting method. Our target locations are determined by fMRI and our prescribing neuroscientist and physician, rather than their proprietary software.
| Accelerated fMRI - TMS | Magnus SAINT™ TMS | |
|---|---|---|
| FDA-Approved iTBS | ✔ | ✔ |
| FDA-Approved Neuronavigators | ✔ | ✔ |
| FDA-Approved Figure 8 Coils | ✔ | ✔ |
| Number of Treatment Days | 5 | 5 |
| Treatments per Day | 10 | 10 |
| Total Treatments | 50 | 50 |
| Number of TMS Pulses | Approx. 90,000 | 90,000 |
| Resting motor threshold pulse intensity | 90–120% | 90–120% |
| FDA-Approved Personalized DLPFC Targeting | ✘ | ✔ |
| Personalized DLPFC Targeting Assists Doctor in Target Location | ✔ | ✘ |
| Personalized E Field Coil orientation | ✔ | ✘ |
| Cost | $9,000 to $12,000 | $30,000+ |
This accelerated protocol of TMS is:
To improve patient outcomes, we also include cognitive behavioral therapy (CBT) as a part of our treatment. When combined with the traditional method of TMS (rTMS), CBT improved response and remission rates by ~8% and ~19%, respectively. Additionally, CBT is likely to produce sustained improvement over time once treatment has concluded.
Our brain stimulation treatment is ideal for most patients with treatment-resistant depression. However, we do not treat patients under the age of 18 or over 65. Additionally, as a safety measure, we do not treat patients who have a history of seizures or who are currently actively suicidal and in need of crisis care.
Click here to learn more about receiving accelerated fMRI TMS therapy at Cognitive FX.
Although TMS has been available for a few years, it remains a relatively lesser-known treatment for depression, and misconceptions about it are common. Some of the main misconceptions include:
As we’ve discussed in this article, the risk of experiencing serious side effects during or after TMS sessions is very low throughout the weeks of treatment. Most side effects are mild and dissipate shortly after the session. No long-term negative side effects have been reported and TMS is considered a safe procedure. This applies to the various types of TMS, ranging from repetitive transcranial magnetic stimulation (rTMS) to deep TMS.
According to a study conducted by the team at Stanford University, 60% of patients were still in remission more than 4 weeks after completing the treatment. In addition, some studies suggest that patients who can stay symptom-free for a few months are unlikely to relapse again.
TMS therapy has long passed the experimental phase. This procedure is FDA-approved and recognized as a legitimate treatment for depression in many countries. This procedure has undergone extensive research, clinical trials, and regulatory scrutiny. It is a viable option for patients seeking alternatives to traditional treatments for depression.
Sometimes, patients feel worse before they start to feel better. This is known as a TMS dip and it’s usually short-lived.
As we’ve seen, TMS uses magnetic waves to stimulate healthier levels of a special kind of electrical activity that neurons use in areas of the brain that are either underactive or inactive. This triggers nerve cells to release important chemicals in the brain (called neurotransmitters) and form new neural pathways. New neural pathways allow the brain to start using new communication patterns that positively influence the patient’s thinking and behavior.
However, this process takes time and sometimes the brain gets “stuck” in the old ways, causing patients to feel worse for a while. If you’re currently undergoing TMS therapy and are experiencing a dip, you must talk to your therapist. It’s very important to persevere with the treatment, even if you aren’t feeling better yet.
Studies show that TMS doesn’t cause serious cognitive issues. In fact, some patients may experience temporary enhanced cognitive skills. Why this happens isn’t well understood, but it’s likely triggered if the magnetic waves during TMS sessions are targeting areas involved in specific cognitive skills.
TMS in young patients poses some challenges. A child’s brain is still developing and there is a chance that TMS may disrupt the nervous system and cause long-term impairments. Despite these concerns, multiple studies detected no serious or long-term side effects worse than what’s observed in adults. However, the number of children exposed to TMS is still significantly lower compared to the adult population.
It’s important to note that children are more prone to seizures and hear TMS sounds more intensely than adults, which means they need to be more closely followed.
There is still limited research in this field, but results seem to suggest that TMS is safe and effective for pregnant women. This is likely because magnetic fields attenuate rapidly with distance, and are unlikely to reach the fetus. Encouragingly, babies born to mothers treated with TMS for depression during pregnancy didn’t experience perinatal complications and were within normal limits in both cognitive and motor development.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

If you’re considering transcranial magnetic stimulation (TMS) therapy, one of the first and most important questions you’re likely to ask is: “Is TMS safe?”

Transcranial magnetic stimulation (TMS) and neurofeedback are gaining popularity as non-invasive, medication-free options for treating depression—especially for people who haven’t found relief from ...

Both Transcranial Magnetic Stimulation (TMS) and Vagus Nerve Stimulation (VNS) are FDA-approved neuromodulation treatments for depression. At first glance, they may seem similar—both use electricity...

Clinics across the U.S. now offer TMS therapy specifically for anxiety. While early research suggests TMS may be an effective treatment, only a handful of studies have focused exclusively on anxiety.
If you’re wondering what to do when transcranial magnetic stimulation (TMS) doesn’t work, you might be:

If you’re considering Transcranial Magnetic Stimulation (TMS) — a procedure that uses electromagnetic pulses to improve depression symptoms — you may be wondering what the treatment actually feels...