What to Know About Combining Antidepressants & TMS Therapy
Patients considering transcranial magnetic stimulation (TMS) often wonder whether or not they can continue taking their antidepressant medication while undergoing TMS treatment.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Perhaps this situation sounds familiar: Months ago, you got a concussion, and you’re still suffering from persistent symptoms, such as headaches, fatigue, and brain fog. To make matters worse, your mood keeps sinking lower, it’s easy to lose patience with friends and family, and it’s hard to concentrate at work (if you’re still able to work at all).
If you’ve been to see a neurologist or a psychiatrist, they may have suggested antidepressants to address some of the symptoms. Perhaps you’ve started taking some already without good results. Many doctors don’t have the resources to fully address post-concussion symptoms, so they prescribe antidepressants and hope for the best. Antidepressants, plus some counseling if you’re fortunate, is a typical treatment of depression, but this approach falls far short of what most patients with a post-concussion syndrome (PCS) diagnosis need.
At Cognitive FX, we believe that patients with PCS need to be treated holistically. This means addressing the root of symptoms caused by the mild traumatic brain injury (mild TBI or mTBI for short) instead of treating individual symptoms as if they were unrelated to the changes in the brain and nervous system that can happen after a head injury.
Our combination of exercise and multidisciplinary therapies works to restore healthy functioning throughout the brain and nervous system. It addresses a multitude of physical and cognitive symptoms and, depending on the cause, may also improve depressive symptoms. Even if you still need further treatment for depression after therapy, symptoms will be easier to treat once the underlying dysfunction in the brain has been addressed.
Even though we believe antidepressants should not be the first option to treat depression, there are some circumstances where these medications are an appropriate choice. However, PCS patients need to be especially careful regarding which medications are chosen because brain injury patients do not always metabolize and respond to meds the way a healthier individual might.
In this article, we’ll discuss aspects to consider when choosing the best antidepressants for PCS patients and look at some alternatives to use instead of (or in combination with) those antidepressants.
We’ll cover:
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.
Studies show that about one-third of patients experience depression in the first year after a head trauma, and this value doubles for patients who continue to experience symptoms and deficits for more than seven years. These symptoms reflect changes in the brain that the patient cannot control.
Under normal circumstances, we have two systems that regulate our motivation to do something: the behavioral activation system (BAS) and the behavioral inhibition system (BIS). They cannot be active at the same time; we’re either “activating” or “inhibiting” motivation. Every time something happens, your brain will use one of these two systems to analyze the situation and act accordingly.
The BAS is activated when you engage in something that you perceive as positive if you achieve it. The BAS is associated with positive emotions, such as excitement, happiness, and hope.
However, a concussion causes the brain to feel less optimistic about life. Patients may have to stop working and avoid social contact with friends and family because of their symptoms. Coping with these changes can be devastating to the patient’s quality of life and mental health. At some point, even simple choices like what to eat for lunch become too overwhelming.
This is a gradual transition, and patients may not realize immediately that they’re experiencing depression. However, at some point after the injury, PCS symptoms can activate BIS. This system focuses on negative emotions, such as anxiety, distress, and pain, which can make patients experience stress disorder and feel like there is nothing good to look forward to. Patients may try to force themselves to carry out their daily activities, but motivation is low and the burden of depression becomes greater.
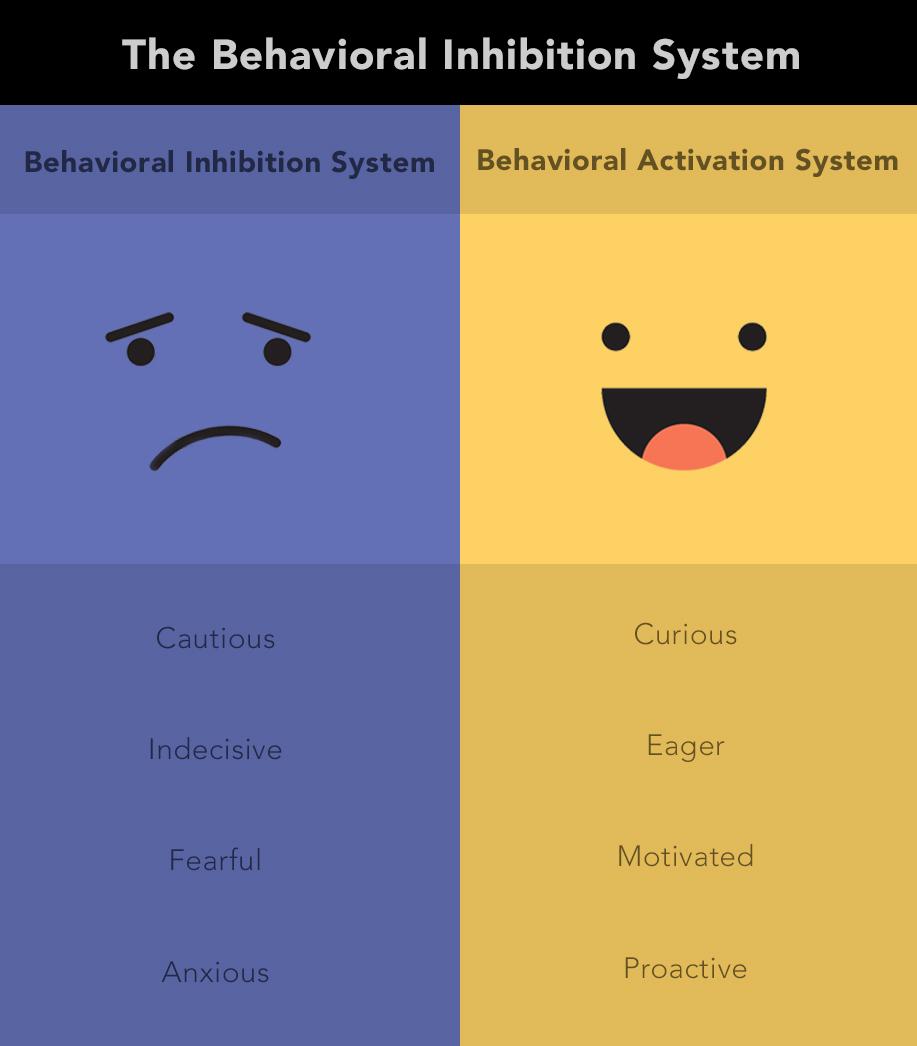
To make matters worse, these patients often get stuck in a vicious circle: Their depression makes them experience more severe PCS symptoms, such as headaches, blurred vision, dizziness, aggression, and cognitive problems, and their PCS symptoms exacerbate their depressive symptoms. This makes it very hard to recover as patients struggle to go to work or attend school, engage in social outings, or even get some exercise.
Recently, a group of researchers suggested that this type of depression combined with PCS symptoms should be considered a distinct condition called TBI affective syndrome. Using brain imaging techniques, these researchers found differences between the brains of depressed patients who suffered a concussion and those of the general population who haven’t had a brain injury. In other words, PCS depression is driven by something different in the brain which may cause different symptoms and need specialized treatment.
Doctors and other healthcare professionals shouldn’t think about depression after a concussion the same way they think about depression in other patients. In practical terms, treatments that work for other patients — such as antidepressants, for example — may not benefit patients with persistent postconcussive symptoms.
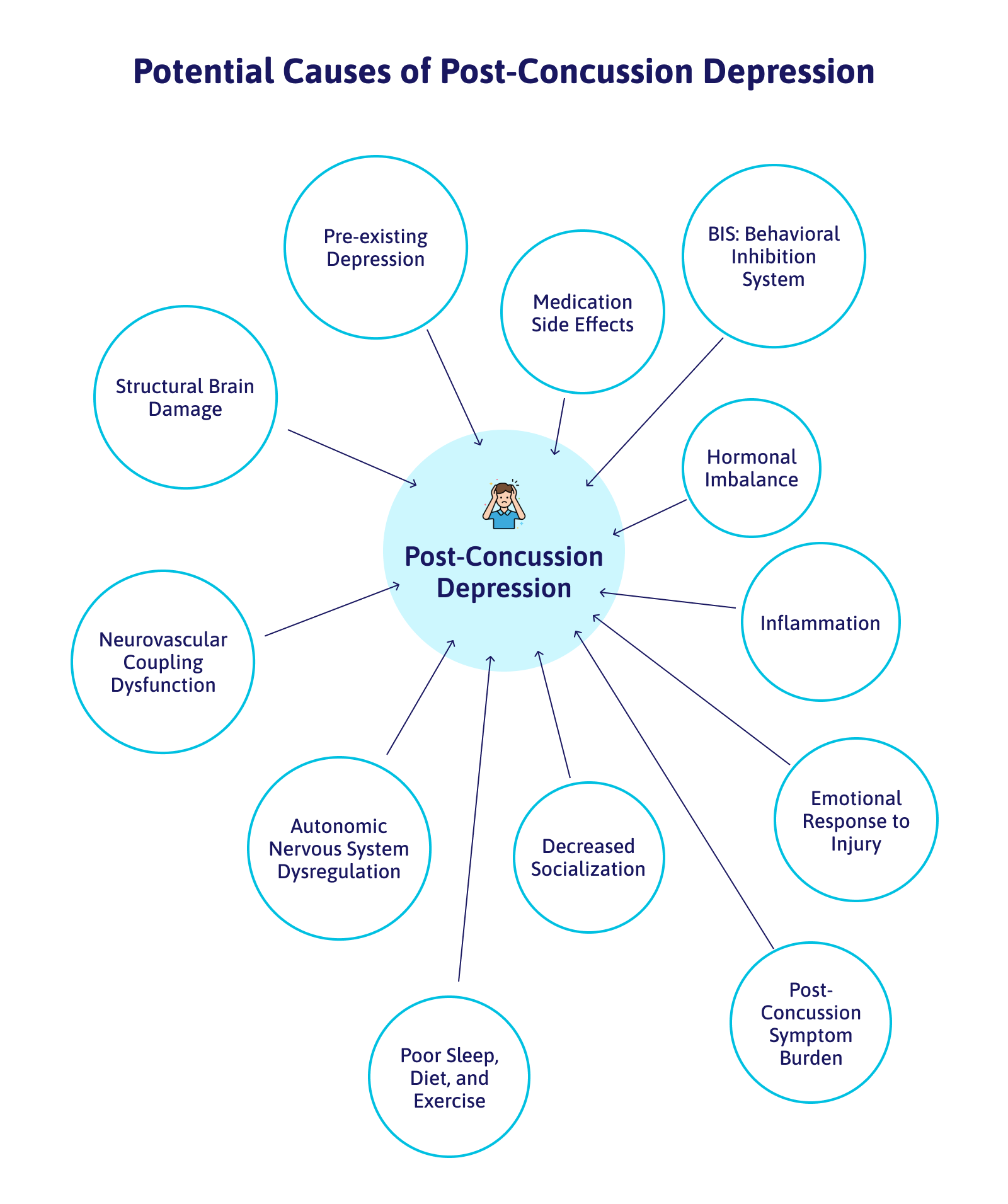
Understanding the underlying causes of symptoms (including depression) is key to an appropriate treatment direction. PCS patients may develop depression due to many different causes, including the following:
If PCS patients started experiencing depression or other mood disorders shortly after their injury, then it’s likely that these symptoms resulted from damage to the areas of the brain that control emotions and mood, including the amygdala, the thalamus, and the hippocampus. For example, researchers found that, in patients with depression, the hippocampus (an area involved in long-term memories) is smaller and less active than normal, whereas the amygdala (an area associated with emotions such as anger, sorrow, and fear) is more active.
Depressive symptoms may also arise due to changes in neurovascular coupling. Under normal circumstances, brain cells need access to a dynamically regulated supply of energy and oxygen. When these cells need to perform a specific task, they can request these resources from surrounding blood vessels, which are then delivered to the right place at the right time. This dynamic connection between the vascular system and the brain is called neurovascular coupling (NVC).
Concussions disrupt this dynamic mechanism, and some areas of the brain don’t receive the right resources (too much or too little) or they get delivered at the wrong time. This disruption can cause symptoms such as headaches, fatigue, poor sleep, irritability, and sensory sensitivity.
Neuroinflammation triggered by the concussion may cause (or at least exacerbate) depression in some PCS patients. Researchers don’t fully understand the mechanism involved in this process, but an exaggerated inflammatory response in the brain may cause changes in areas of the brain involved in behavior. These patients typically respond poorly to antidepressants; targeting the inflammation rather than the depression symptoms may be a better way to provide care.
Depression can develop if patients struggle to adjust to living with their symptoms, especially if they have to stop working or engaging in activities they enjoy. They may be experiencing financial problems or difficulties in their relationships with their loved ones. The problem is that when patients start to experience changes in their mood after the concussion, it’s easy for these symptoms to get worse over time.
Further reading: Depression after a concussion
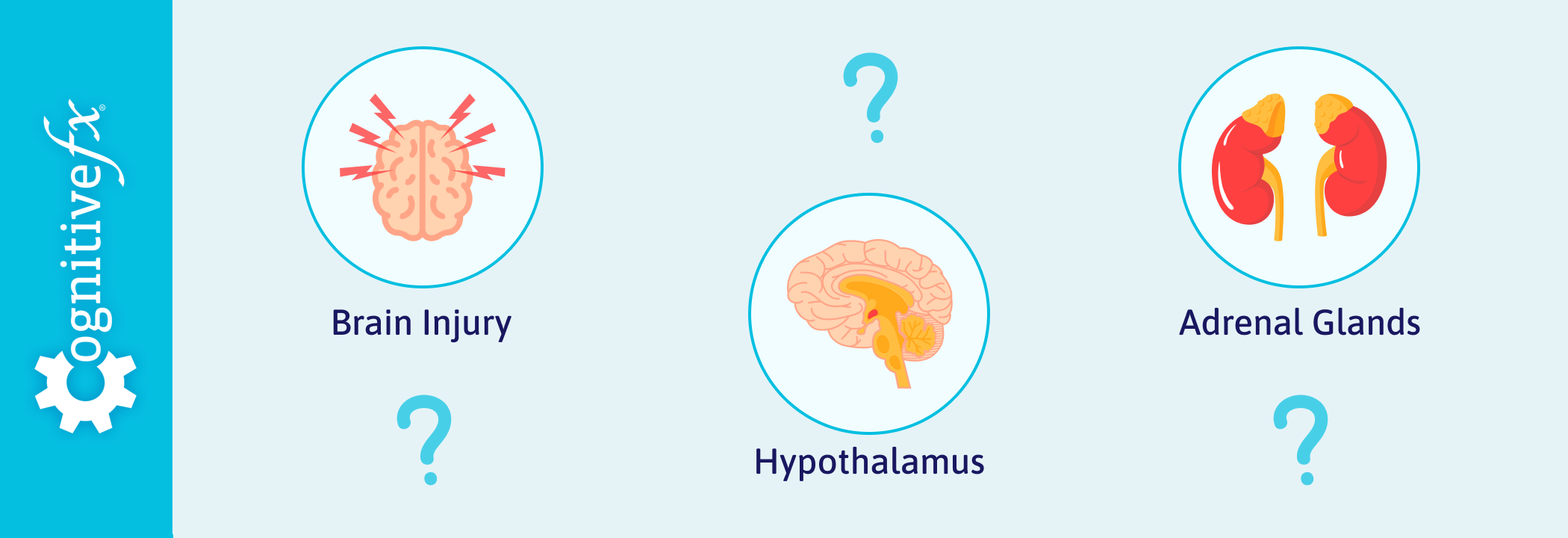
Concussions can also lead to hormonal problems, especially if the hypothalamus and pituitary gland are affected.
These two glands are considered the master regulators in the endocrine system and control major bodily functions, such as the heart rate and blood pressure, body temperature, appetite and body weight, sleep cycle, and function of the gastrointestinal tract. Not surprisingly, if they’re injured by a concussion, they may not function properly. In addition to physical symptoms, hormonal changes can also cause emotional problems. For example, low thyroid levels can cause patients to feel sluggish, tired, less interested in activities, and irritable.
Further reading: Hormone dysfunction after a head injury
A concussion can also create an imbalance between two key parts of the autonomic nervous system (ANS): the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
The SNS and PNS work together to regulate a multitude of bodily functions, such as heart rate, speed of digestion, blood pressure, sleep, vision, and more. Control of the ANS is primarily located in the upper cervical spine, which can easily be affected by whiplash or post-concussion complications such as muscle tension and stress.
As a result, the SNS, which governs the fight-or-flight response and prepares the body to handle stressful situations, often becomes dominant, leading to reduced influence from the PNS, which has a calming effect on the body’s systems. This constant state of tension can feed into emotional regulation and result in an increased incidence of depression, anxiety, and other negative feelings.
Further reading: Dysautonomia after a head injury
Depression and sleep problems are closely linked. Many PCS patients get trapped in a vicious circle where they experience problems sleeping because they feel down and stressed. Sleep deprivation aggravates these symptoms further. Common sleep issues associated with depression include insomnia, hypersomnia, and sleep apnea. Sleep issues may influence the function of the neurotransmitter serotonin (which is involved in regulating mood), disrupt normal circadian rhythms, and heighten the body’s stress responses.
Dysfunctional sleep is a common symptom of PCS that may be rooted in brain dysfunction. Getting treatment for underlying causes of poor sleep can help tremendously if the depression is being exacerbated by low-quality sleep.
Further reading: Post-concussion sleep issues & treatment

Antidepressants should rarely be the first option to treat depression in PCS patients, but there are some situations where these meds can be helpful. In addition to helping with mood, antidepressants may also help with the other symptoms of depression, such as low energy, poor concentration, poor sleep, low appetite, and anxiety.
That said, there is limited evidence to support the use of antidepressants with neurotrauma patients. At best, studies show that antidepressants can help patients when accompanied by psychotherapy, but when used alone, most studies found no improvements in patients receiving antidepressants.
The decision to start taking antidepressants is something you need to discuss with your psychiatry or neurology practitioner. However, below we outline some key considerations for patients with concussion sequelae.
Side effects are common in patients being treated with antidepressants and may include headaches, dizziness, stomach upset, sleep disturbances, fatigue, and difficulties with sexual intimacy. If this happens to you, you need to decide whether the benefits you’re getting from the medication outweigh the distress of the side effects.
Make sure your medical provider knows about your history of head injuries and posttraumatic symptoms, as PCS patients are more sensitive to side effects compared to patients who haven’t suffered a concussion. In most cases, this happens because of metabolism changes after the concussion: blood is often diverted away from the liver and other organs that process medications and pumped into the brain instead. More blood reaches the brain (which can change the concentration of medication delivered), and if the liver becomes less able to metabolize medication, the chances of experiencing side effects increase.
Antidepressants take time to work. Patients may need to take medication for a few weeks before noticing any improvements. Sometimes, your physician will need to change the dose over time or switch to a different medication if one doesn’t work well enough. In some cases, two different antidepressants can be used together if a single medication is not effective.
Finding the best antidepressant for you may take a few attempts. Your doctor may put you on a certain medication, but then you have to wait 6–8 weeks to see if it has any effect. If it doesn’t work, you may have to try different meds and wait a few more weeks. You may have to repeat this process multiple times until a suitable medication is found.
To speed up this process, patients may be asked to undergo a genetic test to help narrow down options. Although these tests can’t determine specifically which antidepressant will work best for you, they offer clues about how your body may respond. The test assesses variations in genes that determine how quickly a drug is metabolized in the body or whether patients may have side effects from a certain drug.
For example, the test may indicate that the patient’s body metabolizes a certain drug very slowly, which means the drug might build up in the body, increasing the risk of side effects. The drug may still be useful, but patients may need lower doses. On the other hand, the test may suggest that a certain drug is metabolized extremely fast, not giving it a chance to work properly. In this case, patients may need higher doses than normal to get an effect.
Stopping antidepressants needs to be done carefully and with the support of your doctor. You should never stop abruptly, as this may cause a variety of uncomfortable symptoms, including fatigue, nausea, headaches, dizziness, anxiety, and even problems sleeping. Your physician will recommend a gradual decrease in the doses, which may take several months.
As we’ve described above, depression in PCS patients can be caused by many different factors, and antidepressants are not designed to help with many of them. For some patients, depressive symptoms won’t ease off until the underlying factors triggered by the concussion — such as neurovascular disruption, for example — are treated.
Antidepressants are not suitable for every patient. For example, antidepressants that increase levels of norepinephrine are not suitable for patients with heart issues, a history of panic attacks, or hyperactivity. High levels of norepinephrine cause feelings of euphoria, but they may also cause panic attacks, high blood pressure, and hyperactive behavior.
Or, consider that adolescents need to exercise extra caution with antidepressants. For example, a systematic review of publications that investigated suicide rates (and suicide attempt rates) in adolescents showed a significant increase in suicide for adolescents taking antidepressants vs. those who did not take them.
At this moment, there are no medications approved by the U.S. Food and Drug Administration specifically for the treatment of post-TBI depression. This means antidepressants prescribed to PCS patients have not been tested on people who sustained a brain injury and may not operate as expected in these patients, or they may produce unexpected side effects.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in the long-term symptoms of head injury. To see if you are eligible for treatment, sign up for a consultation.

The most commonly used antidepressants to treat post-concussion depression are selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs).
SSRIs are one of the most commonly prescribed antidepressants. They work by increasing the levels of serotonin in the brain. Serotonin is a neurotransmitter in the brain that carries messages between nerve cells to regulate mood, emotion, and sleep. After delivering a message, serotonin is reabsorbed by the brain cells (a mechanism called reuptake). SSRIs work by blocking this reuptake, making more serotonin available to pass further messages between nearby brain cells.
Some of the most commonly prescribed SSRIs include:
For many years, doctors believed that depression was caused by an imbalance in the brain and that keeping serotonin within normal levels would help regulate mood. However, recent research and clinical trials are questioning this theory. A growing number of scientists and doctors are starting to recognize the chemical imbalance framing as an oversimplification that doesn’t apply to all patients. This reflects what we know from our experience with PCS patients: Depression can have many causes (as we’ve described earlier), and not all patients respond to antidepressants.
Whereas SSRIs impact levels of serotonin, SNRIs impact the levels of both serotonin and norepinephrine. Similarly to SSRIs, SNRIs work by blocking the reabsorption (or reuptake) of serotonin and norepinephrine, which increases the levels of active neurotransmitters in the brain. While serotonin creates feelings of well-being, norepinephrine promotes feelings of alertness and energy, and this combination can relieve symptoms of depression and anxiety and boost the patient’s mood.
There are several different SNRIs available, including:

When choosing between an SNRI or an SSRI, make sure you discuss the pros and cons with your medical provider. Your doctor will assess your medical history, diagnosis, reaction to other medications, specific symptoms, and your lifestyle to help them decide which medication is best for you.
If a pharmacological approach is warranted, SSRIs are more commonly used to treat patients with depression, but many of these medications are not suitable for PCS patients. There is some evidence to support the use of sertraline, fluoxetine, and citalopram, but studies involve a small number of participants, and researchers advise against using these antidepressants in PCS patients. In addition, many other antidepressants remain untested. There are some clues, however, about their mode of action to suggest that they may not be suitable for PCS patients. For example, paroxetine aggravates cognitive impairments, and fluoxetine takes a long time to be metabolized, increasing the risk of side effects. This means neither of these SSRIs is a good option to treat PCS patients.
That said, SSRIs may improve other PCS symptoms, including headache, fatigue, sleep problems, cognitive function, and memory, as well as reduce patients’ perception of the severity of their symptoms.
The second option, SNRIs, are newer drugs and therefore there is limited evidence regarding their use with PCS patients. However, preliminary studies suggest they’re just as effective in treating both emotional and cognitive problems as SSRIs, with the bonus that they may trigger fewer side effects. To our knowledge, this is the only study assessing the use of SNRIs after a concussion but, from our experience, we find that PCS patients tend to tolerate SNRIs better than SSRIs.
In addition, a controlled study in mice found better results with SNRIs compared to SSRIs, with the authors suggesting that SSRI medications can aggravate some of the symptoms, such as anxiety and memory problems, commonly experienced after TBI.
Overall, our view is that — if you have to try antidepressants — SNRIs may be marginally better than SSRIs, but this may vary significantly from patient to patient.

Some types of antidepressants should be avoided in most cases because they are not suitable for PCS patients. These include:
TCAs, such as amitriptyline, amoxapine, desipramine, and doxepin, are an older type of antidepressant. Most doctors avoid their use to treat PCS patients with depression. Not only do they cause more unpleasant side effects than SSRIs and SNRIs, but they can cause seizures even in patients who have never suffered seizures before.
MAOIs are also an older type of antidepressant that are rarely used nowadays because they cause potentially serious side effects. Using MAOIs requires patients to follow a strict diet to avoid foods that contain tyramine — such as certain cheeses, pickles, and wines — as well as some medicines, including pain medicines, decongestants, and some herbal supplements. In addition, patients should not take MAOIs combined with other antidepressants like SSRIs or SNRIs. Doing so can cause serotonin syndrome, which is potentially fatal.
The efficacy of atypical antidepressants to treat depression in PCS patients has not been established yet. In addition, some of these antidepressants also increase the risk of seizures. If your doctor is suggesting an atypical antidepressant, ask about a slow-release formulation.
Antidepressants are not the only way to deal with depression symptoms. As described earlier, we believe they shouldn’t even be the first type of treatment to try.
Here is a brief look at other treatment options:

All the pharmacological treatments described so far in this article focus on addressing depression symptoms in isolation. However, at Cognitive FX, we believe that post-concussion syndrome should be treated as a whole condition, not as individual symptoms.
Resolving your post-concussive symptoms — issues such as headaches, fatigue, difficulty concentrating, and sleep problems — can have a significant impact on how you feel. If your depression was closely connected with your primary symptoms (the ones caused directly by the concussion), it may resolve quickly after you complete treatment for post-concussion syndrome with us.
Even if your post-injury symptoms are secondary — which means they developed after the injury but were not directly caused by the concussion — treatment for post-concussion syndrome can still help. If that’s the case for you, you may need additional psychological treatments (as described above) to overcome depression, but therapy will be easier at this stage. If you try to do it the other way around — psychotherapy first, then treat other PCS symptoms — it will likely be harder to recover from the depression.
As long as PCS symptoms linger, they will continue to feed your depressed state of mind and lower your mood.
At Cognitive FX, we offer a combination of exercise and multidisciplinary therapies to treat PCS patients. Before treatment starts, patients undergo an extensive neuropsychological evaluation, including:
Patients also complete a functional Neurocognitive Imaging (fNCI) scan to determine exactly what areas of the brain were affected by the concussion. This scan allows our therapists to image 100 different regions of the brain, investigating how blood flows in the brain and how different areas communicate with each other while our patients complete a set of predetermined cognitive tasks.
Once our team has gathered all this information, they can design a treatment plan customized for each patient. Treatment involves a three-step cycle that is repeated throughout time at the clinic: Prepare, Activate, and Recover.
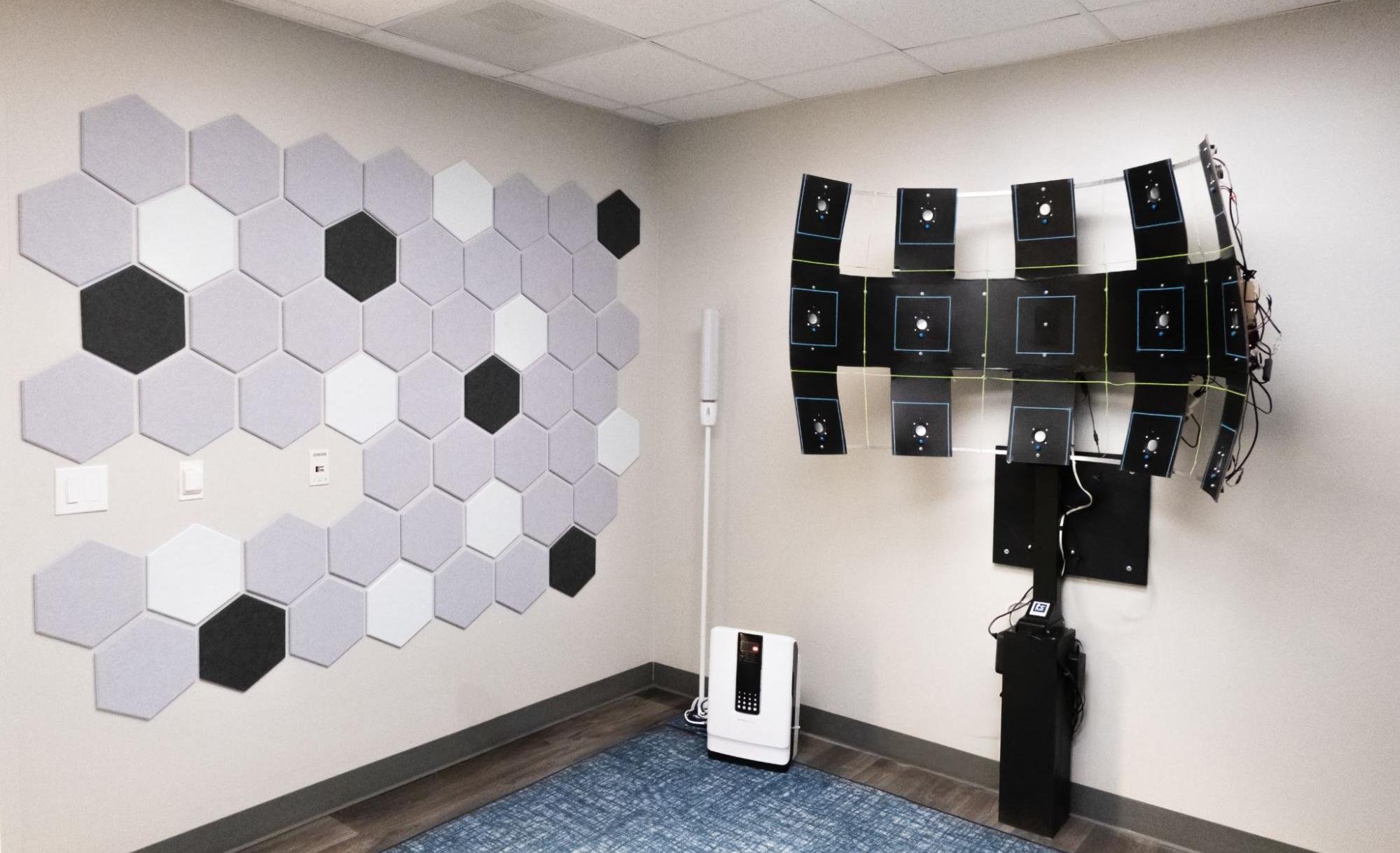
Prepare: Treatment starts with a short session of aerobic exercise, usually on a stationary bike or treadmill. Interval-based exercise helps the sympathetic and parasympathetic branches of the nervous system work together again. It also promotes the release of a chemical in the brain called brain-derived neurotrophic factor (BDNF).
BDNF helps the brain adapt to changes and learn better, thereby boosting the impact of subsequent therapies. Curiously, there is some evidence that low levels of BDNF are associated with depression, which means this step is particularly important for PCS patients suffering from this condition.
![EPIC Treatment Dynavision [V7]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20Dynavision%20%5BV7%5D.jpg?width=1999&height=1333&name=EPIC%20Treatment%20Dynavision%20%5BV7%5D.jpg)
Activate: After exercise, patients engage in a series of therapies, including occupational therapy, neuromuscular therapy, neurointegration therapy (including vision and vestibular therapy), cognitive therapy, sensorimotor therapy, and psychotherapy.
During treatment, all patients meet with a psychologist to be assessed for depression and anxiety. If our therapists feel that you would benefit from further therapy, we will refer you to a psychologist in your area.
In addition, if we think your depression symptoms could be related to hormonal imbalances, we’ll order or refer you for blood tests to detect any problems. If you do have hormone dysfunction, we’ll refer you to an endocrinologist for further treatment, which will also help with your depression symptoms.

Rest: The last step of treatment involves periods of relaxation in between therapy sessions. These periods may include breathing exercises and listening to brainwaves to promote relaxation, neuromuscular massage of the neck and shoulders, and mindfulness exercises.
At the end of treatment, patients undergo a second scan to assess how their brain is changing and meet with one of our therapists to discuss their progress. Patients also receive a set of “homework” exercises, typically including aerobic exercises, cognitive activities, and relaxation techniques. Our recommendation is for patients to start doing these exercises about an hour every day, five days a week, and then slowly reduce the time as they recover. Completing these exercises gives you the best chance of a full recovery.
90% of our patients report reduced symptoms (with an average improvement of 60%) after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.
![EPIC Treatment memory game with cards [V2]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20memory%20game%20with%20cards%20%5BV2%5D.jpg?width=1490&height=1076&name=EPIC%20Treatment%20memory%20game%20with%20cards%20%5BV2%5D.jpg)
Here are a few ways to ease your depression symptoms at home:
Exercise may feel like the last thing you want to do, but it’s a proven method to improve your mood. Find a comfortable routine, like going for a short walk in the morning or doing some gentle flexibility exercises in the evening. If you can, work your way up to 30 minutes of cardio every day for the best results. Just keep in mind that PCS patients sometimes experience symptom spikes during or after exercise because of the brain injury. If that’s you, read our post on how to exercise safely after a concussion.
Diet is an important component of mental health. Studies show that following a diet low in processed foods and rich in fruit, vegetables, whole grains, fish, low-fat dairy, and antioxidants reduces the risk of developing depression and alleviates symptoms.
Further reading: Nutrition for post-concussion syndrome
It’s common for PCS patients with depression to also experience cognitive issues. Engaging in cognitive games and activities is a great way to keep your brain active. It also stimulates brain cells and promotes communication between different areas of the brain. You can try many different activities, from puzzles and crosswords to learning to play a musical instrument.
Further reading: Cognitive exercises for post-concussion syndrome recovery
Patients with depression often also experience problems sleeping, including finding it difficult to fall asleep at night or feeling sleepy during the day. These problems exacerbate depression symptoms, leading to a negative cycle that can be difficult to break. Going to bed at the same time every day, avoiding long daytime naps, and limiting your intake of alcohol and caffeinated drinks in the evening can help you sleep better, boost your mood, and help decrease some of the symptoms of depression. Melatonin supplements may also prove useful.
Talk to your loved ones about how you’re feeling and why you may appear distracted. If you find this difficult, try to find other ways of communicating, such as writing a letter or sending a text message.
Avoid becoming socially isolated. Make sure you spend some time interacting with family and friends. If you struggle with busy and noisy places, meet your friends at home or in a quiet location. If meeting face-to-face is difficult, you can communicate with your friends via text messages or phone calls.
Educate yourself on the effects of brain injury, including common physical, cognitive, and emotional symptoms. Being aware of the possibilities can help you adjust your expectations. In turn, this makes it easier for you to accept where you are and set realistic goals for improvement.
Find a local support group where you can find support from other patients who are experiencing a similar situation.
Further reading: Post-concussion syndrome support groups
Use well-being techniques, such as mindfulness, yoga, meditation, or other relaxation methods. Studies show that these methods are similar in efficacy to cognitive behavioral therapy for depression symptoms in adults.
If you're experiencing symptoms of depression after a concussion, your doctor may recommend a cocktail of drugs, including antidepressants. It’s important to know that many of these meds are not suitable for everyone and may make symptoms worse.
Here are a few things you need to consider if you’re thinking about antidepressants:
Even if you don’t feel like there is hope for the future, there are many steps you can take toward recovery. We would be honored to walk with you on this journey. If you’re ready to seek post-concussion syndrome treatment, please sign up for a consultation with our team.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Patients considering transcranial magnetic stimulation (TMS) often wonder whether or not they can continue taking their antidepressant medication while undergoing TMS treatment.

You've waited weeks. You've followed every instruction. And you still feel the same, or maybe even worse. If your antidepressant isn't working, you're not imagining things, and you're far from alone.

Antidepressant medication is often the first treatment offered to patients with major depressive disorder. However, these medications are not as effective as once thought and frequently trigger...

Many doctors aren’t aware that concussions can cause long-lasting symptoms, a condition commonly called post-concussion syndrome (PCS). As a result, they treat common symptoms rather than the...

Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.

Sustaining a traumatic brain injury can be a challenging experience. You probably felt angry, demoralized, helpless, and even hopeless in the days following your injury. For some people, these...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY