Low energy, difficulty concentrating, brain fog, anxiety, depression, memory problems...
This laundry list of symptoms is common in people who suffer from post-concussion syndrome (PCS), which is when symptoms of a mild traumatic brain injury (mTBI) persist long after they should have gone away.
These are also common symptoms of hormonal dysfunction, such as hypothyroidism, growth hormone deficiency, or adrenal insufficiency.
You might wonder: Can you have both post-concussion syndrome and hormone dysregulation? And if you have both, is it just an unhappy coincidence, or can a brain injury cause both conditions? The quick answer is that yes, you can have both, and yes, a brain injury can cause both conditions.
Over the past few years, research has shown a connection between traumatic brain injury (TBI) and neuroendocrine disorders. The authors of 2018 review article Post-Traumatic Hypopituitarism—Who Should Be Screened, When, and How? assert that post-traumatic hypopituitarism (PTHP) is a common and under-diagnosed consequence of TBI. They believe that screening for PTHP should be part of standard post-injury care because the last fifteen years of research shows such a high rate of pituitary dysfunction after moderate and severe TBI.
Another study focused on veterans who sustained blast-related mTBIs found evidence of PTHP in 42% of the study participants. The authors of this study also recommended routine screening for hypopituitarism (insufficient hormones produced by the pituitary gland) of anyone who has sustained a brain injury, regardless of its severity.
Hormones are an important but often-overlooked piece of the puzzle when it comes to brain injury symptoms. The brain affects hormone production, and hormones affect the body and the brain. They don’t work in isolation.
In this article, we provide a comprehensive patient guide to hormonal dysregulation caused by brain injury. We cover:
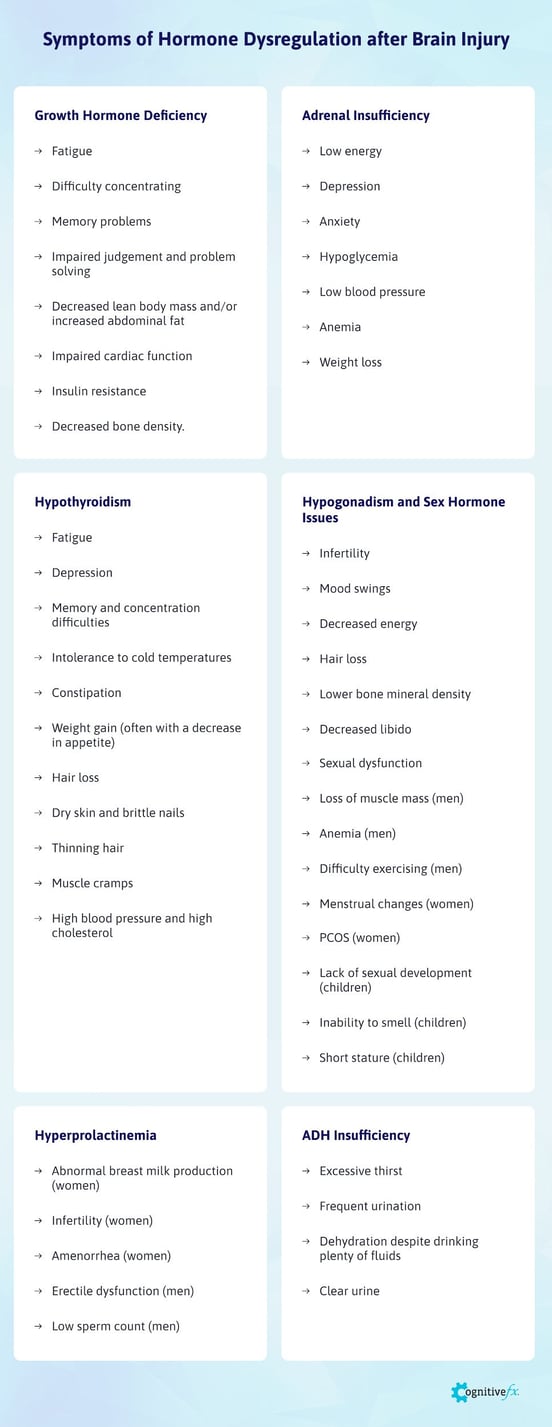
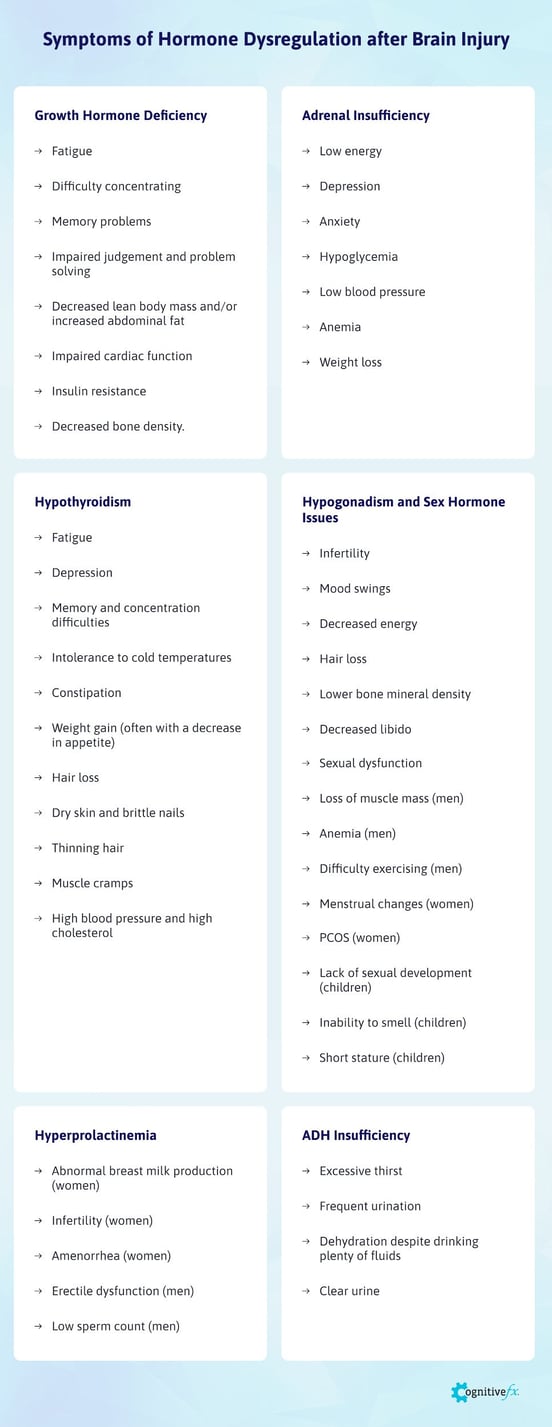
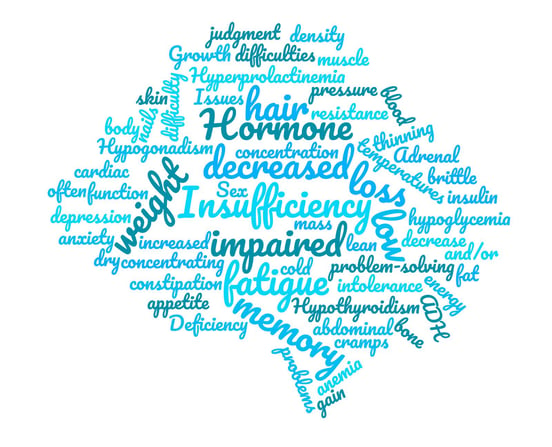
We’ll dig into specifics on symptoms later in the post, but here’s a quick glance at what patients experience:
If you’ve been suffering from symptoms connected to a possible brain injury, we may be able to help. 95% of our patients show statistically verified restoration of brain function. Schedule a consultation to discuss your symptoms with a member of our team.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
How Does a Brain Injury Cause Hormone Dysregulation?
A brain injury results from trauma to the brain. This could be from an external force or impact, such as when someone falls and hits their head on concrete, or when they’re hit by an object like a soccer ball. It could happen from whiplash, such as when your head snaps forward and backward quickly during a car accident. It could even happen as a result of a seemingly harmless jarring motion, such as when you trip and fall but don’t hit your head on anything at all.
You can also injure your brain from internal causes. Infections such as meningitis and COVID-19, events like stroke, and exposure to chemicals or toxins such as carbon-monoxide or chemotherapy drugs can also cause brain injury.
Traumatic brain injuries are usually classified as severe, moderate, or mild. Mild traumatic brain injuries, known as concussions, are the most common. However, even a “mild” TBI can cause significant, long-lasting symptoms and spur hormone dysregulation.
What Happens Inside the Brain During a Brain Injury
The brain is an intricate system of blood vessels and neurons which govern thought, movement, emotions, senses, balance, and memory. This soft, vulnerable tissue is surrounded by a protective fluid and the skull.
When something hits the head, the force causes the brain to crash against the skull. Affected parts of the brain compress, stretch or twist. (Think of the brain as a big gelatin mold. It’s one solid piece, but when you touch it, the whole thing shakes.)

This forceful impact causes bruising and inflammation. It can damage neurons and disrupt neurovascular coupling (NVC), the communication system between neurons and blood vessels in the brain. To function properly, neurons need oxygen. They call for precise amounts of oxygen-rich blood when they need it. When NVC is dysfunctional, injured areas of the brain might not get the resources they need in the right amounts or at the right time. Other areas of the brain might then try to step in and help, but they can’t do an efficient job because they have their own tasks to accomplish.
Neurovascular coupling dysfunction is the cause of many post-concussion symptoms. Unfortunately, this type of damage won’t show up on a standard magnetic resonance imaging (MRI), so if your doctor is trying to connect your symptoms to a brain injury, standard imaging won’t show anything wrong. At Cognitive FX, we use functional Neurocognitive Imaging (fNCI), a special type of MRI to detect neurovascular coupling dysfunction (we’ll explain more about it later in this post).
How Are Hormones Affected by Brain Injury?
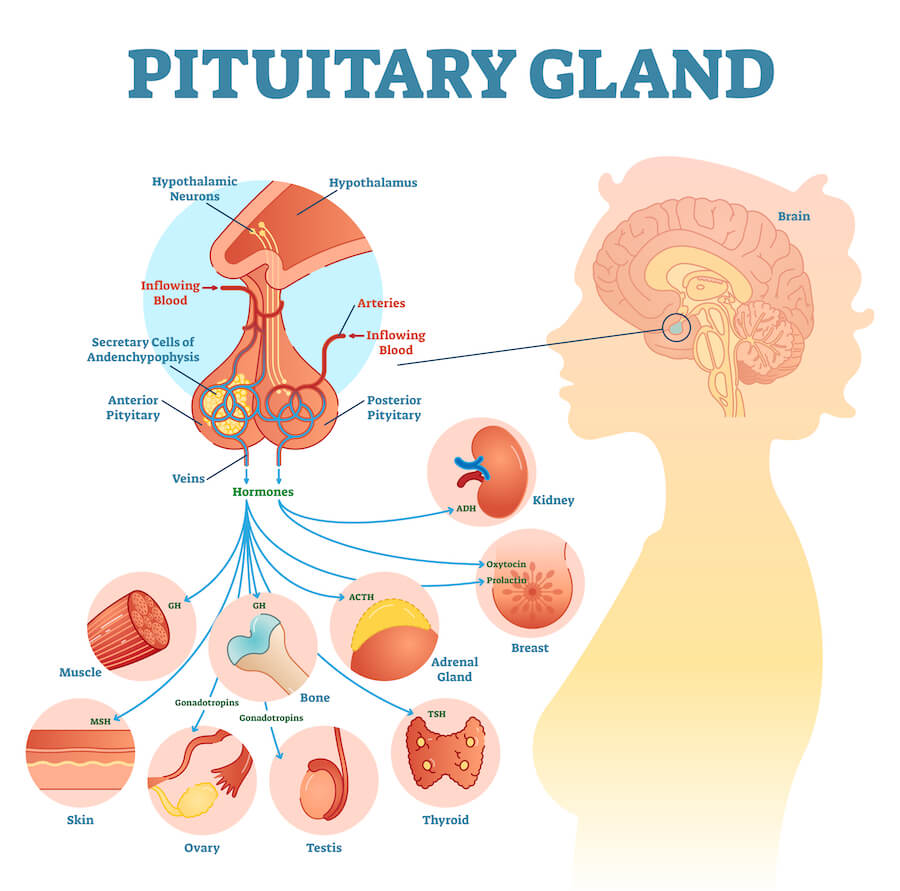
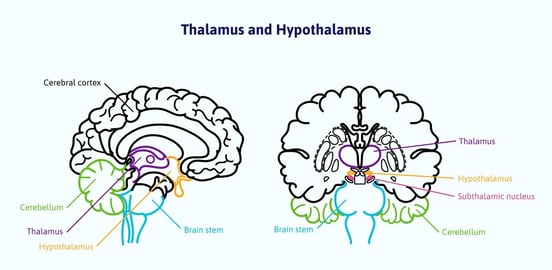
Key brain regions that affect hormone production and regulation are the pituitary gland and the hypothalamus. Because of their location in or next to the brain, they are easily impacted by brain injury. Damage to any one of them leads to the overproduction or underproduction of hormones, which affects the entire body.
The Pituitary Gland
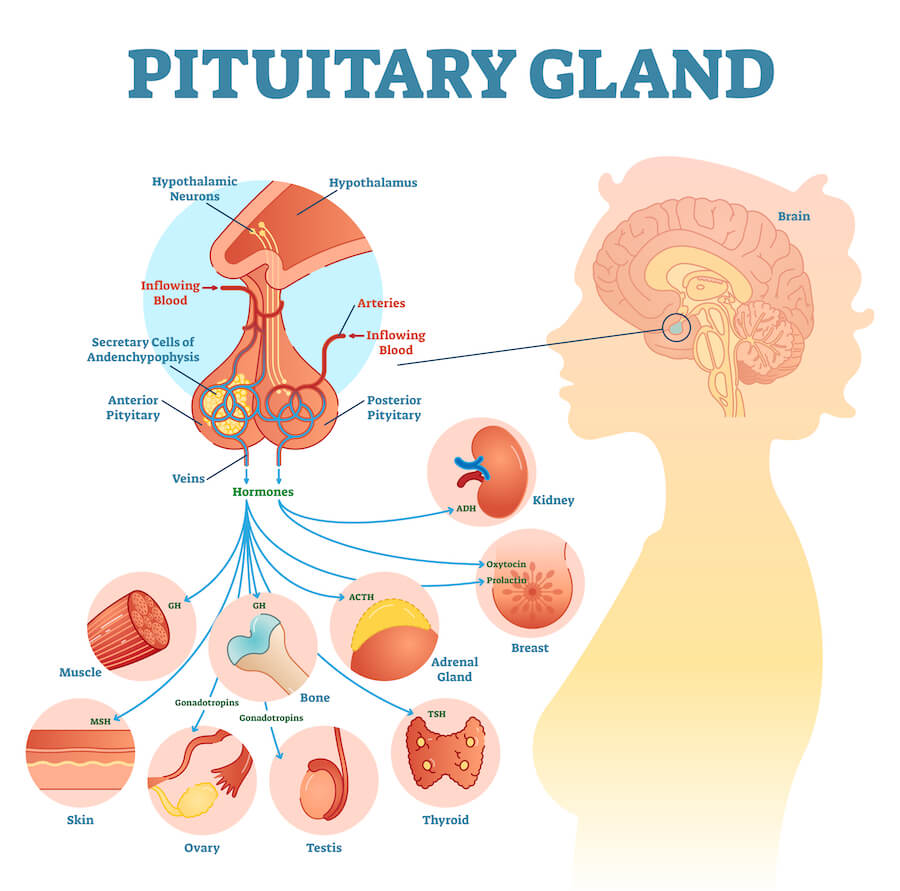
The pituitary gland is known as the “master gland” because it is central to the endocrine system. It is located at the base of the brain and consists of two parts. The anterior pituitary is connected to the brain by blood vessels. The posterior pituitary is the part that actually secretes hormones into the blood system. The pituitary stalk, which contains many blood vessels, connects the pituitary to the hypothalamus. A brain injury to this area rarely leads to visible damage to the pituitary, but it can affect pituitary function by damaging the neurons and blood vessels that are important parts of neurovascular coupling in that region.
The pituitary produces these hormones:
Creating too much or not enough of any of these pituitary hormones causes problems. Problems with the pituitary gland can also lead to issues with hormone production in the thyroid and adrenal gland.
When the pituitary gland doesn’t make enough of the hormones it’s responsible for producing, we use the umbrella term, “hypopituitarism.” It’s also sometimes called pituitary insufficiency. Causes of hypopituitarism other than head injury are benign tumors, bleeding, medication, radiation treatment, and infections.
Hypothalamus
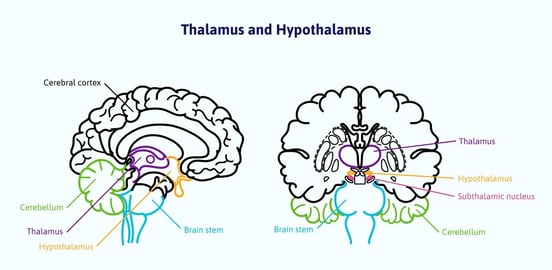
The hypothalamus is located between the pituitary gland and the thalamus in the inner brain. It connects the nervous system with the endocrine system.
The hypothalamus communicates with the pituitary gland and signals it to release or stop releasing certain hormones, especially those that affect the thyroid, gonads, and adrenal glands. It affects the production of growth hormones by telling the pituitary to increase or decrease their production.
The hypothalamus produces hormones that tell the pituitary to make or to communicate the need for other hormones, including:
It also controls the autonomic nervous system (ANS), which is responsible for maintaining homeostasis and involuntary processes in the body. It gathers and processes information sensed by the brain, such as stress, temperature, and hunger, and then tells the body to respond appropriately.
ANS dysfunction is another major contributor to PCS symptoms such as inappropriate blood pressure and heart rate responses, headaches, feeling too hot or too cold, and sexual dysfunction. Some of the symptoms of ANS dysfunction and hormonal dysregulation overlap. Either or both could be causing your symptoms.
How to Identify Hormone Dysregulation
There are generally two ways to identify hormonal problems: symptoms, and blood testing.
Evaluating symptoms isn’t easy. Hormonal changes can happen slowly over time. They’re also attributable to other factors such as stress, genetics, or aging. Hair loss, unexplained weight gain, and decreasing energy levels can be mistakenly chalked up to, “I guess I’m just getting old.” Hormone deficiency is a risk factor for cardiovascular disease in addition to the unpleasant symptoms it causes, so it’s important to have it diagnosed and treated.
The other way to identify hormone dysregulation is from blood testing. Testing isn’t always clear-cut either. We’ll tell you about some problems you need to be aware of when it comes to trying to get medical validation for your symptoms.
Common Symptoms of Hormone Dysregulation
Here is a general list of hormone dysregulation symptoms. (We’ll go into more detail about specific hormones and their associated symptoms in the next section.)
- Energy levels: Decreased energy and increased fatigue are symptoms of several types of hormone dysregulation.
- Growth problems: A child, teenager, or young adult who seems to stop growing and appears younger than others their age could have a growth hormone deficiency. Occasionally, the opposite happens: The patient doesn’t stop growing and goes far beyond their expected height and bone size.
- Unexplained weight change: Unexplained weight gain or weight loss despite eating a healthy diet is something to pay attention to. We’ve had patients who tell us they eat 4000 calories a day and are still extremely thin. Others eat nothing but vegetables and have inexplicably gained 40 pounds.
- Hair changes: Hair loss, thinning hair, or other texture changes are typical of some hormone problems. This can happen slowly over time. You might have small bald spots. Sometimes hair starts growing in the wrong places!
- Skin and nail changes: Skin might become dry, thin, scaly or itchy. Nails sometimes become brittle.
- Changes in body temperature: Feeling too hot or too cold, especially when no one else in the same area experiences the same feeling, is typical of a hormonal imbalance. Some people have a low tolerance for cold.
- Mental health: A new occurrence of depression or anxiety that can’t be explained by a situational event, such as a death in the family, could be hormone related. Feeling apathetic and losing interest in things that normally interest you also falls into this category.
- Women’s health issues: Common issues women face include changes in menstruation frequency and/or flow, amenorrhea, early-onset menopause, Polycystic Ovary Syndrome (PCOS), fertility problems, and vaginal dryness.
- Body physique: Hormone imbalance might be behind increased abdominal fat or decreased muscle mass.
- Memory and concentration problems: Difficulty concentrating and remembering things are possible with hormone imbalance. Impaired problem solving could also be present.
- Sex drive: Decreased libido in men or women, as well as erectile dysfunction in men, can be caused by hormonal imbalance.
- Bone mineral density: Reduced bone mineral density can be caused by several hormone deficiencies. You might only become aware of this one if you easily fracture bones, though bone mineral density testing is common if you’re taking certain medications or are of a certain age.
- Excessive thirst and increased urine production: These are common symptoms of ADH insufficiency.
Some of these symptoms can be caused by conditions other than hormone dysregulation. However, if you are experiencing any of these symptoms, and they persist more than 3 months, we encourage you to get your hormone levels tested.
Blood Tests For Hormone Dysregulation

Getting a blood test to determine if you have hormone dysregulation seems like it should be a simple, straightforward process. Sometimes it is. Often it’s not. In fact, it can be fairly complicated.
Resistance From Your Doctor
The first obstacle you might encounter is resistance from your physician to test at all. This seems to defy logic, but it happens. Despite describing your symptoms and wondering if they could be related to a hormone problem, some doctors push back. Maybe they believe your symptoms are completely unrelated to hormones and they won’t consider it. (“Just exercise more and lose some weight, and you’ll feel so much better!”) Maybe they did one type of test, and that came back normal, so they’ve completely discounted the issue. Maybe they think you just like to complain and are seeking attention.
If you continue to have symptoms and your doctor doesn’t seem to be listening to you, it might be time to find another doctor. Or at least find another way to get the tests done.
Getting the Right Tests Done
The next issue might be getting the correct tests done. For example, your doctor might be ordering only one test when several are needed. Doctors tend to test only the final hormone level itself, but you might also need to test the levels of other signaling molecules involved in the process.
Let’s look at the adrenal glands, for instance. They produce cortisol and aldosterone. Cortisol helps your body respond to stress, and aldosterone helps your body maintain the right balance of water, salt, and potassium.
The process of cortisol production actually starts in the hypothalamus. It senses that your body needs more cortisol, so it sends some corticotropin-releasing hormone (CRH) to the pituitary gland. CRH tells the pituitary to make adrenocorticotropic hormone (ACTH). ACTH is what induces the adrenal glands to make and release cortisol. The hypothalamus and the pituitary continue to monitor the amount of cortisol in your blood and make adjustments when necessary. If something goes wrong during any part of this process, you are going to feel bad.
It’s likely that your doctor will order a blood test to measure your cortisol levels. Cortisol levels vary throughout the day, however, so it’s important to measure them at the right time. Also, cortisol is the end product. It could be that your lab test result on that day measured some amount of cortisol — just within the “normal” zone — which means your adrenals are technically working. In this case, your doctor is probably going to tell you that’s not the problem.
However, maybe this wasn’t a complete picture of your adrenal function. Other tests might shed more light. The cortisol urine test might give a more accurate indication of your cortisol production over a longer period of time. The ACTH stimulation test will show whether or not your adrenal glands are responding appropriately to ACTH produced by the pituitary gland. The Insulin-Induced Hypoglycemia test will help determine if the hypothalamus and the pituitary gland are giving the appropriate orders to the adrenal glands in response to stress to begin with.
One test in isolation may not be enough to understand if your adrenal system is functioning as it should. We’ll make a few recommendations for which tests to get in the next section.
What Is “Normal?”

Another big problem with hormone tests is in reading the results. The “normal” range on lab test results is often very wide. It is found by testing a number of people who are assumed to be healthy and using their results to determine the range of what’s average or normal. This range isn’t foolproof, however.
Just because your results fall within the “normal” range doesn’t necessarily mean you are fine. Your abnormal might fall within the typical normal range. It’s possible that your post-injury blood test numbers — even if they’re in the “normal” range — are significantly changed from your pre-injury numbers (data which most patients do not have). Unfortunately, many doctors do not take this information into account.
Many of our patients have described their debilitating symptoms to doctors, only to have those doctors reply, “But your tests are normal. There’s nothing wrong with you.”
If you recognize that you had a brain injury and are experiencing symptoms of hormone dysregulation, keep pressing. Your struggles are real. Sometimes it takes a few tries to find a doctor that will take you seriously and look deeper. The best doctors diagnose based on test results and symptoms.
What If Hormones Aren’t the Main Problem?
When hormone dysregulation begins after a concussion, we have to consider that the problem might not be with the glands themselves. Rather, neurovascular coupling dysfunction could be the root cause of the problem — or at least a huge contributing factor.
If communication to or from the pituitary gland is dysfunctional or inefficient, the correct orders for hormone production might not be going out as they should. For example, the pituitary gland might not receive the message from the hypothalamus that the body needs more cortisol, so the adrenal glands might not be notified to make more. Or the pituitary might send an order for the wrong amount, or send it too late. As a result, the adrenals produce an insufficient amount for the body’s needs. A simple blood test won’t show this kind of problem.
When in Doubt, Get Tested
All this is not to say that blood tests are unreliable or useless. Many patients are helped by blood tests under the right medical supervision. We strongly recommend them to our patients. But it is to say that which tests you take and how your doctor interprets them matters.
Note: If you’ve been suffering from symptoms connected to a possible brain injury, we may be able to help. 95% of our patients show statistically verified restoration of brain function. Schedule a consultation to discuss your symptoms with a member of our team.
Common Hormonal Problems After a Brain Injury
Until recently, hormone dysregulation after brain injury was thought mainly to affectTBI patients who sustained a moderate or severe injury. Now, more researchers are studying changes from mTBIs. A 2014 article in The Journal of Family Practice noted that in one study, the incidence of neuroendocrine dysfunction (NED) after an mTBI was 16.8%, and in another, it was as high as 42%.
A review of fourteen studies on hypopituitarism following traumatic brain injury showed that growth-hormone deficiency was the most commonly reported endocrine dysfunction after a TBI. They noted that this deficiency was linked to “impaired quality of life, depression and poor rehabilitation outcome.” They found hypogonadotropic hypogonadism (low sex hormones) to be the next most common endocrine dysfunction associated with head trauma. Patients also often had altered production of ACTH and thyroid hormones.
These hormonal dysfunctions sometimes happen only during the acute phase of injury and are of short-term duration. Others develop over time, sometimes two to three years after injury.
Below, we cover six common hormonal issues that brain injury patients face: growth hormone deficiency, adrenal insufficiency, hypothyroidism, hypogonadism, hyperprolactinemia, and ADH insufficiency.
Growth Hormone Deficiency

Symptoms of growth hormone deficiency (GHD) include:
- fatigue.
- difficulty concentrating.
- memory problems.
- impaired judgment and problem solving.
- decreased lean body mass and/or increased abdominal fat.
- impaired cardiac function.
- insulin resistance.
- decreased bone density.
Many of these symptoms are similar to those of thyroid dysfunction and other conditions, so it’s easy to overlook.
Children with GHD usually appear younger than others their age. Puberty is often delayed. As young adults, they sometimes look significantly younger than they are.
Growth hormones naturally decline as we age. In adults, GH is used for energy regulation instead of growth.
Since GHD is so common after a concussion, we like to test growth hormones in our patients who are under 30 years of age. We specifically recommend the GH stimulation test. Often, doctors are reluctant to test growth hormones. They tend to take a wait-and-see approach.
Children are usually treated with replacement GH by injection. Adults are not typically treated with replacement GH.
Sometimes, the pituitary creates too much growth hormone. This condition is called acromegaly. Common symptoms are enlarged hands and feet and facial structure changes. It usually affects adults. It’s most often caused by a tumor in the pituitary gland, so it’s something to get checked out if you have symptoms.
Adrenal Insufficiency

Adrenal insufficiency is also known as corticosteroid deficiency. It has three subcategories:
- Primary adrenal insufficiency, also known as Addison’s disease, in which the adrenal glands don’t make enough cortisol and aldosterone because the glands themselves are damaged. This condition is usually permanent.
- Secondary adrenal insufficiency, which happens when the pituitary gland doesn’t make enough ACTH. This means the adrenal glands won’t make enough cortisol.
- Tertiary adrenal insufficiency, in which the hypothalamus doesn’t create enough corticotropin-releasing hormone. This is the hormone that instructs the pituitary to make ACTH. Without ACTH, the adrenal glands won’t make enough cortisol.
Some of the symptoms of adrenal insufficiency are:
- low energy.
- depression.
- anxiety.
- hypoglycemia.
- low blood pressure.
- anemia.
- weight loss.
Symptoms usually increase when the body is under stress. An adrenal crisis is life threatening. Its symptoms include nausea and vomiting, abdominal pain, confusion, and extreme weakness.
To test for adrenal insufficiency, we recommend testing morning (fasting) serum cortisol levels. If that test is indicative of adrenal insufficiency, it might warrant testing of ACTH and a corticotropin stimulation test.
Treatment depends on which condition you have and its severity. Patients who need medication take replacement doses of medicine such as hydrocortisone. Some also have to take fludrocortisones, which help the body maintain sodium and potassium levels.
Hypothyroidism

Hypothyroidism is a common endocrine disorder in which the thyroid doesn’t produce enough thyroid hormone. The hypothalamus and the pituitary gland are involved in this process.
When the hypothalamus senses thyroid hormone levels are low, it secretes thyrotropin-releasing hormone (TRH), which tells the pituitary gland to release thyroid-stimulating hormone (TSH). The release of TSH tells the thyroid gland to produce the right amounts of triiodothyronine (T3) and thyroxine (T4), then send them out to whatever part of the body needs them.
Symptoms of hypothyroidism include:
- fatigue.
- depression.
- memory and concentration difficulties.
- intolerance to cold temperatures.
- constipation.
- weight gain (often with a decrease in appetite).
- hair loss.
- dry skin and brittle nails.
- thinning hair.
- muscle cramps.
- high blood pressure and high cholesterol.
To test for hypothyroidism, we recommend measuring serum free T4 (fT4) and TSH.
Thyroid hormone replacement therapy is the standard treatment, most commonly with levothyroxine (L-T4). However, some trial-and-error with medication and dosage is often necessary. Sometimes, dietary changes are sufficient to see improvement even without medication.
Note: Another less common thyroid disorder is hyperthyroidism. In this case, the thyroid makes too much T-3 and T-4. Blood tests also usually indicate low levels of TSH. Hyperthyroidism is not usually associated with brain injury. It’s usually a result of an autoimmune disorder or the growth of nodules on the thyroid that affect thyroid hormone production.
Hypogonadism and Sex Hormone Issues

Hypogonadism is the condition in which the male testes or the female ovaries don’t produce enough (or any) sex hormones. When this condition is caused by a problem with the pituitary gland or the hypothalamus, it is called hypogonadotropic hypogonadism (HH).
The production of sex hormones again involves a chain of communication. The hypothalamus releases gonadotropin-releasing hormone (GnRH). This tells the pituitary gland to release follicle stimulating hormone (FSH) and luteinizing hormone (LH). These then tell the testes to produce testosterone and the ovaries to produce estrogen and progesterone. If anything goes wrong in this chain of command, hormone production is impaired.
Symptoms of hypogonadism vary by sex and age:
- Children with hypogonadism experience a lack of sexual development. They sometimes are also unable to smell and might be short in stature.
- Both women and men often experience infertility, mood swings, decreased energy, hair loss, and decreased bone mineral density.
- Men commonly experience a decrease in sex drive and function, low testosterone, loss of muscle mass, anemia, and decreased exercise tolerance.
- Women might experience menstrual cycle changes such as amenorrhea, infrequent or light menstruation. They might also have some sexual dysfunction. We’ve noticed that quite a few of our female patients also developed Polycystic Ovary Syndrome (PCOS) after a concussion.
If we suspect hypogonadism, we recommend that men be tested for total thyroid and free thyroid, FSH, LH, and prolactin. Estrogen levels in women should be tested in the form of serum estradiol (E2). We also recommend testing FSH, and LH levels.
This condition is usually treated with replacement hormones.
Hyperprolactinemia
Another hormone to be aware of in this category is prolactin. This hormone is produced by the pituitary gland and is influenced by the hypothalamus. It has many functions, but it is most commonly known to be involved in breast milk production.
Both men and women can suffer from too much prolactin (hyperprolactinemia) or too little prolactin (hypoprolactinemia), which is very rare.
Common symptoms of hyperprolactinemia in women are the production of breast milk when there shouldn’t be any, infertility, and amenorrhea. Men often experience breast enlargement, erectile dysfunction, and low sperm count.
We recommend a blood test of prolactin levels if you are experiencing any of these symptoms. It’s a good idea to check testosterone levels in men as well. If your prolactin level is high, you’ll probably need to get an MRI of the brain and pituitary gland done because this condition is often caused by a benign tumor on the pituitary gland. The tumor can also press on the optical nerves, which can affect your vision. It’s usually treated easily with medication, though sometimes radiation or surgery is recommended.
ADH Insufficiency

Antidiuretic hormone (ADH) insufficiency is also known as diabetes insipidus. ADH, also called vasopressin, helps the kidneys maintain the proper balance of water in the body. It’s an important factor in blood-pressure regulation.
ADH production begins in the hypothalamus. It travels to the pituitary gland, which releases it into the bloodstream.
Symptoms of ADH insufficiency include excessive thirst, frequent urination, and dehydration despite the consumption of large quantities of fluid. Urine is often very clear in color.
For testing, we recommend a urinalysis, simultaneously measuring serum and urine osmolarity.
This condition is treated with a medication that is similar to ADH.
Some Final Thoughts About Common Post-TBI Hormone Problems
Because these conditions are so common after a brain injury, we talk to our patients about hormones when they come to us for post-concussion syndrome treatment.
We aren’t medical doctors (we’re a group of PhDs, neuropsychologists, and therapists), but we can get blood tests done inexpensively at our clinic when we suspect hormone dysregulation. Our nurse can draw blood between your therapy appointments, and we can get the results during your time at Cognitive FX. This is a completely optional service that is helpful for patients who never thought about a hormonal issue before or whose doctors were reluctant to test. We can forward test results to your chosen physician. We can also collaborate with your physician if you were being treated prior to coming to our clinic. Treatment for PCS might repair some of the hormone dysfunction, which makes follow-up testing advisable.
As we noted, treatment in the form of hormone replacement or medication is available for most of these conditions.
Sometimes working with a nutritionist to modify your diet is sufficient. Ask if there are any changes you can make to help with hormone production or to reduce the amount of medication you need to take.
Treatment at CFX: How Can It Help with Hormones?

To be clear, we don’t directly treat hormone dysregulation at CognitiveFX. You should see an endocrinologist to treat and manage those conditions.
We also can’t promise that being treated for post-concussion syndrome will end your hormone dysfunction. However, if the problem behind the hormone dysregulation is neurovascular coupling dysfunction, then restoring that can improve hormone production.
Remember that a large part of hormone production depends on accurate and timely communication between the thalamus, hypothalamus, pituitary gland, and the rest of the body. Some of our patients have been able to reduce or completely go off their hormone medications after treatment at our clinic because this communication system was repaired.
Here’s a surprising example: We’ve seen a number of patients get pregnant (after struggling with infertility) shortly after treatment at our clinic. Some of them were in fertility treatment for years without success. It could just be a coincidence, but it’s happened enough for us to call them “Cognitive FX babies.”
EPIC Treatment for Post-Concussion Syndrome
While our treatment program may or may not restore your hormone balance, it will rehabilitate your brain’s neurovascular coupling and reduce or eliminate symptoms from post-concussion syndrome.
Enhanced Performance in Cognition Treatment (EPIC treatment) is unique, active rehabilitation that targets each patient’s dysfunctional brain regions.
Prior to treatment, each patient goes through a series of imaging scans, one of which is the fNCI. As patients work through specific cognitive activities, we can see and track blood flow in the brain, revealing hyperactive and hypoactive regions as compared to non-injured brains.
The thalamus is one of the sixty regions of the brain that we look at with the fNCI. It is a critical component of the hormonal communication system in the brain. Detecting thalamus dysfunction in patients with hormone dysregulation means there is a chance that symptoms will improve after treatment.
Our team of experienced professionals creates an individualized treatment plan for each patient based on fNCI results and symptoms. Therapies include neuromuscular therapy, balance and cognitive exercises, vision therapy, occupational therapy, and sensorimotor therapy. This combination of therapies and exercises is designed to force the brain to use efficient, pre-injury communication pathways. Patients also meet with a psychologist for help with mood issues and help coping with their recovery journey.
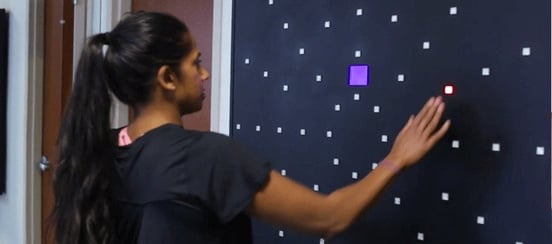
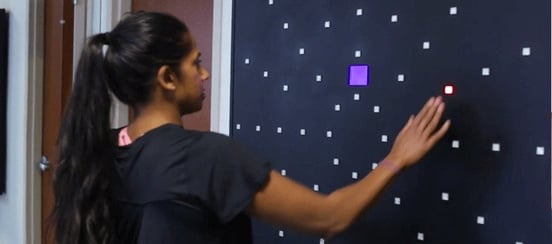 A patient during Dynavision therapy, which works on multitasking, reflexes, and more.
A patient during Dynavision therapy, which works on multitasking, reflexes, and more.
EPIC treatment is not easy, but we are there to help and support patients every step of the way. (Read about the experience of seven of our patients who found help for PCS through treatment at our clinic.)
At the end of treatment, each patient repeats the fNCI. We compare before and after treatment results to measure the change in blood flow to each area of the brain. We typically see a 75% improvement in brain function during treatment, and patients report a 60% improvement in their symptoms in just one week.
Most patients continue to improve after EPIC treatment. It’s a process that takes time and effort. We give each patient a post-care plan to continue exercises at home. We periodically check in to monitor progress, answer questions, and make recommendations when necessary.
For patients who do have hormone imbalance in addition to PCS, we can assist in finding specialists to work with near their home and are happy to coordinate with their physicians in whatever way we can.
Conclusion

We know how difficult it can be to get help for PCS and hormone dysregulation, especially since so many of the symptoms are attributable to other common conditions. Many doctors just aren’t familiar with how a concussion can cause them. It can be easy to lose hope, especially if doctor after doctor tells you they can’t find anything wrong with you.
Don’t give up. You know your body better than anyone. If you know something’s not right, trust your instincts, and keep searching for answers.
We can’t promise that our treatment will repair your hormone dysregulation. But we can help considerably with post-concussion syndrome, and we can get you on the path to treatment for endocrine dysfunction. It isn’t an easy journey — it takes hard work in therapy and finding the right dose of medications — but you can get better.
Our patients, on average, report 60% improvement in their symptoms after just one week of treatment. And 95% show statistically verified restoration of brain function. If you’ve been suffering from symptoms connected to a possible brain injury, we may be able to help. Schedule a consultation to discuss your symptoms with a member of our team.