Can Post-Concussion Syndrome Cause Stuttering?
Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
“It never used to be like this.” This may be something you’ve said many times about your menstrual cycle. Given that there's a high risk that women will develop irregular periods after they suffer a mild to moderate traumatic brain injury (TBI), this is not surprising at all.
Women experience post-concussion symptoms differently than men. Once women hit puberty, they sustain a higher incidence of concussion, go through different and more severe symptoms, and take longer to recover than men.
Brain injuries can cause changes in your menstrual cycle, including missed periods and painful cramps. Interestingly, the phase of your menstrual cycle can be a predictor of outcomes after a traumatic brain injury. Women injured during the last week of their cycle — when progesterone and estrogen levels are high but decreasing — have worse health outcomes than women injured during the first few weeks when these hormones are naturally low but stable.
For females suffering severe changes in their menstrual cycles, the question they want to answer is, “When will my cycle revert to normal?” In this case, the severity of the injury is a good indicator: Less severe brain injuries usually result in a quicker return to normal, while more serious injuries (or ongoing post-concussion syndrome) may take longer to resolve.
Note: While in this article we often refer to women, we are aware that some transgender men, non-binary and gender fluid people, and intersex people may also experience menstruation. Everything in this article applies to people with a uterus who experience periods. If you’re concerned about any changes in your menstrual cycle, it’s best to follow up with your doctor.
In this article, we cover everything you need to know about the impact of a brain injury on your menstrual cycle, including topics such as:
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. To discuss your specific injury and symptoms, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
The brain is the most complex organ in the human body. It’s responsible for every thought, action, memory, and feeling we experience throughout our lives. To achieve this phenomenal task, the brain contains a staggering one hundred billion neurons, which are surrounded by blood vessels, which deliver the oxygen and glucose the brain needs for energy.
When something hits the head — or even during whiplash or a similarly jarring motion — the force of that event causes the brain to collide with the skull. There’s actually very little space between the brain and the skull, but in the split second after the impact, the head decelerates rapidly, and the force of impact travels deep inside the brain.
A brain injury disrupts the communication between these nerve cells and the blood vessels in the brain. This link between neurons and blood vessels is known as neurovascular coupling. If this is disrupted, injured areas in the brain may not receive the resources they need in the way they need them. While other areas try to compensate, it’s often not an efficient swap.
Because of their location at the back of the head, some of the areas that are easily twisted or damaged by brain injuries in women include the pituitary gland, the hypothalamus, and the fragile pituitary stalk, which connects both sections.
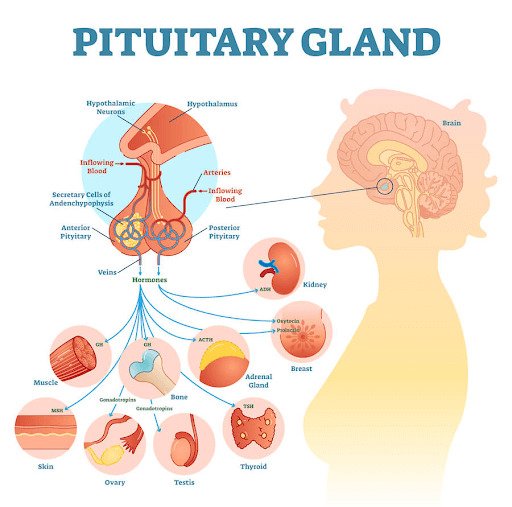
As this is a crucial part of the endocrine system, this kind of damage can result in over- or underproduction of some hormones, which can have serious effects in the body. Studies have shown that up to 80% of patients with a brain injury have some type of hormonal impairment immediately after the injury, and up to 25% of long-term survivors continue to have issues resulting in ongoing problems — which may explain some of the symptoms associated with post-concussion syndrome (PCS).
You can read more about the most common hormone changes after a brain injury here.
Brain injuries can have serious effects on the menstrual cycle, mostly through the action of hormones secreted by the hypothalamus and the pituitary.
The most important hormone from the hypothalamus is called gonadotropin releasing hormone, better known as GnRH. In turn, GnRH stimulates the pituitary to secrete a hormone called follicle stimulating hormone (FSH), which is responsible for stimulating follicle development and causing estrogen levels to rise in the follicular phase. The other hormone from the pituitary is called luteinizing hormone (LH), which is involved in promoting ovulation and the release of eggs from the ovary.
The first day of menstruation is typically identified as the first day of the cycle. The pituitary releases FSH to stimulate the growth of several follicles in the ovary. As the follicles grow, levels of estrogen increase steadily until it triggers a sudden release of LH around day 13 of the cycle. This LH peak triggers a series of events within the follicles, which ultimately result in ovulation of one egg.
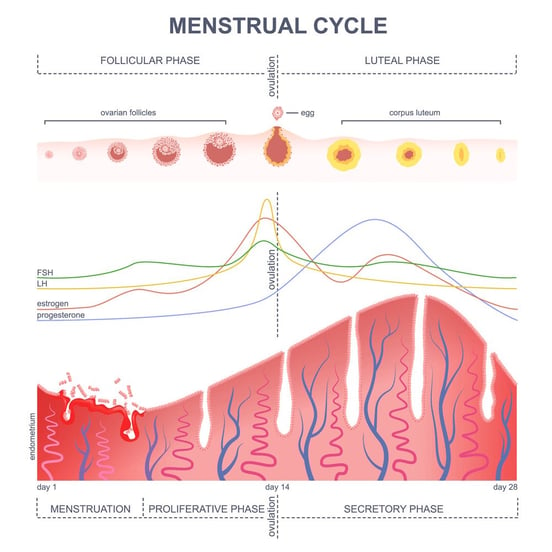
During the luteal phase, the follicular cells left behind in the ovary after ovulation transform into a yellow body called the corpus luteum, which starts secreting high amounts of progesterone to prepare the uterus for implantation in case of pregnancy.
If a pregnancy occurs, the corpus luteum continues to produce progesterone until about 10 weeks of gestation. If no embryo implants, the corpus luteum eventually degenerates and progesterone levels drop. This is the sign for the lining of the uterus to start shedding, leading to menstruation and a new cycle.
After a mild traumatic brain injury, however, these communication channels between the hypothalamus, the pituitary, and the ovary can be severely affected. If anything goes wrong in this chain of command, hormone production is impaired. Studies show that most patients experience a drop in the circulating levels of LH, FSH, progesterone, and estradiol during the first few days after the injury. Thyroid hormones are also affected, with both hypothyroidism (lower levels than normal) and hyperthyroidism (higher levels than normal) causing menstrual disturbances.
Checking reproductive hormone levels may not be at the top of the priority list after a serious and potentially fatal injury, but all these hormones play a vital role in the healthy brain, and their suppression after a concussion can have long-term consequences for women.
Some of these long-term consequences include missed and irregular periods, heavy bleeding and painful cramps, and mood dysregulation. These symptoms may last for months or years after the injury occurred. A study showed that 46% of women with moderate or severe brain injury experienced amenorrhea, and 68% reported irregular cycles up to 60 months post injury.
Menstrual cycles that are continually irregular can have a serious impact on both short- and long-term health. Not only can these changes be distressing for women, but they also can lead to a wide range of more serious conditions, including cardiovascular problems, sleep issues, and poor fertility, to name just a few. This is why it's important to have any potential issues diagnosed as early as possible and managed with the help of a healthcare provider.

The time of injury in relation to the menstrual cycle phase may also influence the outcome. It is particularly dangerous for women to sustain a brain injury after ovulation, when the levels of progesterone are high, compared to immediately after menstruation when levels are low.
Initially, this seems counterintuitive, because progesterone is known to have a neuroprotective effect. However, it seems that it’s not the actual level of progesterone or estrogen that matters, but the fact that there’s a sudden drop a few days after ovulation (dubbed the “withdrawal hypothesis”). This withdrawal of progesterone is more risky for women than the stable levels during the rest of the cycle. For the same reason, time of injury doesn’t affect women taking oral contraceptives, because they have constant hormone levels.
This means a simple question about the date of last menstruation could help to identify who is at increased risk of a poor prognosis when women seek medical assistance after an injury. Women taking synthetic progestins as contraceptives are expected to have a better outcome, as long as they continue to take their birth control pill to prevent any sudden drops in progesterone.
Traditionally, sex hormones have been associated with the reproductive system. However, recent evidence shows that even short-term fluctuations of progesterone and estrogen during the menstrual cycle can have an impact on the brain. Across different parts of the cycle, women go through emotional and cognitive ups and downs. They’re better at spatial awareness after their period, but they turn into expert communicators by the end of the cycle. Most women also experience better moods right after menstruation compared to the period after ovulation.
This influence, however, is not the same for patients dealing with the lingering effects of a brain injury. Instead of mild changes in cognitive skills — which most women probably don’t even notice during the cycle — the impact of a sudden drop in progesterone and estrogen after a brain injury can have much more serious consequences in the brain of PCS patients. Psychological changes can include emotional changes (such as irritability, mood swings, or depressed mood) as well as cognitive symptoms (such as difficulty concentrating and a constant sense of being overwhelmed).
If you’re on medication to treat other symptoms caused by your brain injury, you may find that these can also affect the menstrual cycle. Examples include:
If you’re concerned about changes in your menstrual cycle and think it may be related to medication, call your doctor to determine whether this is an expected side effect of this medicine. If you are taking a medicine not prescribed by a doctor, stop taking it and call your doctor if you need help to control symptoms.

It is possible for menstrual cycles to return to normal spontaneously, even many years after the original concussion, but patients have a much better chance with appropriate treatment. The best course of action varies from patient to patient, but in general terms, treatment involves an attempt to return progesterone and estrogen values to pre-concussion levels.
To measure the level of hormones in your system, your doctor will likely order a multitude of blood tests, including LH, FSH, progesterone, testosterone and estrogen, as well as thyroid hormones. These tests are useful to find the underlying cause responsible for your menstrual changes.
Because they vary so much during the menstrual cycle, some blood tests must be done at specific times. For example, LH, FSH, and estrogen are often done on the second or third day of the cycle, while progesterone is done towards the end of the cycle. You may have to get a series of blood tests that establish how your hormone levels fluctuate across your cycle. You should also tell your doctor about any medications you take, especially birth control pills or hormone therapy, which can affect the results.
Once you get the results, your doctor can then diagnose and manage potential changes to your menstrual cycle caused by a brain injury. A common way to treat a hormone imbalance is with hormone replacement therapy (bioidentical replacement doses of hormones your body should have been producing enough of, but isn’t).
If the problem lies with progesterone and estrogen, starting on birth control is another common approach to control irregular periods. By releasing the right amount of hormones throughout the cycle, birth control pills create a predictable cycle for post-concussion syndrome patients, eliminating unpleasant symptoms like heavy and painful periods. However, it’s important to note that symptoms may return when you stop taking the pill.
A word of warning: Be prepared to try a few products until you find one that suits you. Doctors typically start with a product with a low level of progesterone, but don’t be afraid to try another one, especially if it causes side effects such as mood swings, acne, or painful cramps. Be patient; this process may take a while.
There are also some studies suggesting that short-term estrogen or progesterone injections can be a potential therapy strategy to quickly resume hormone levels. Results seem incredibly promising, with lower mortality rates after severe brain injury and a better outcome for patients with mild cases.
For patients with heavy bleeding, doctors may prescribe tranexamic acid, which can only be used for a few days at a time. This may not be appropriate if patients are also on the pill, as it increases the risk of deep vein thrombosis.
Unfortunately, it could take months or even years for the menstrual cycle to return to normal. Even with the right treatment, how long it takes to go back to a regular period depends on several factors, such as age, history of concussions, treatment approach, and the severity of the injury, among others.
Treatment at Cognitive FX is designed to address a variety of post-concussion symptoms, including headaches, brain fog, fatigue, sleep problems, memory issues, and vision problems, to name just a few. Post-concussion syndrome may become permanent without treatment, but there’s a good chance it will improve with the right therapy.
However, when it comes to menstrual changes, our treatments at Cognitive FX are not directly aimed at treating hormone dysregulation. We advise you to see an endocrinologist or a gynecologist to treat and manage your condition. Having said that, many symptoms of a concussion can exacerbate menstrual cycle symptoms (and vice versa). The overall improvement in wellbeing you experience after going through Enhanced Performance in Cognition Treatment (EPIC treatment) may improve your cycle as well.
EPIC is an intense period of rehabilitation targeting dysfunctional areas in the brain. Before treatment starts, each patient goes through a series of imaging scans to reveal hyperactive and hypoactive regions compared to healthy, non-injured brains.
One of the scans we use is functional Neurocognitive Imaging (fNCI) to see which parts of the brain are working properly and which parts need rehabilitation. With this scan, we can measure neurovascular coupling while the patient performs six different cognitive tests. fNCI produces over 7,000 images of the brain, which are then compared with a healthy control database, allowing us to analyze the impact of the injury in each region of the brain.
While an fNCl scan can’t look directly at the hypothalamus and pituitary, it can analyze the thalamus, which is located directly above these regions. If we detect thalamus dysfunction in patients with hormone dysregulation, this area can be targeted during treatment and — although we cannot guarantee it — there is a chance that neurovascular coupling in the hypothalamus and pituitary gland will also improve.
Based on the results from the fNCl scan, our team of experts create a customized treatment plan for each patient. Therapies used during our EPIC treatment are designed to coax the brain to reestablish communication pathways lost due to the brain injury.
The therapies we use during treatment include but are not limited to:
For patients who come to us with a hormone imbalance, we are happy to work with their physician or, if needed, we can help find specialists near their residence.
At the end of treatment, each patient undergoes another fNCl, including a second look at the thalamus. Comparing before and after, we usually see a 75% improvement in brain function, and patients report a 60% improvement in their symptoms in just one week. However, don’t expect a full return to normal for your menstrual cycle in this period. Even if the fNCl shows an improvement in the thalamus area, it may take months for these changes to trickle down to your ovaries.

If you’re concerned about changes in your menstrual cycle, it’s a good idea to start keeping a record on a calendar or an app. Take a note of your start date every month for several months to identify the regularity of your periods. You will have a better picture of what’s going on during your cycle and can correlate with other symptoms. Even if you haven’t detected any changes, track your cycle anyway. It may uncover some relevant information which may be connected with other symptoms.
You can also use fertility awareness-based methods (FABMs) to help your doctor diagnose your condition. These methods involve examining physical signs, such as cervical secretions and body temperature, to assess hormone fluctuations throughout a woman's menstrual cycle. They can produce robust data about your cycle, which may lead to better treatment. It’s important to note that you cannot be on the pill if you want to use an FABM, as the pill will mask your natural changes in hormones.
If you're worried about your periods, then take note of the following:
Changes in the menstrual cycle may also lead to changes in your sleep patterns. For example, you may feel that it is harder to get to sleep and stay asleep just before your period.
It may be helpful to keep a diary of symptoms for a few months. It will be a good starting point if you need to discuss it with your doctor. Take a note when your period starts and stops, and then you can identify whether these sleeping problems are linked with any particular symptoms you’re experiencing, like strong PMS or irregular periods.
It’s common for head trauma to affect sleep quality, regardless of whether you have menstrual changes. Read this post to learn more about sleep changes and how you can rest better after a concussion.
Exercise has many health benefits that can help your periods, and it has been shown that it can effectively alleviate painful and irregular periods. It can also relieve emotional symptoms associated with menstruation (such as depression and anxiety) and improve quality of life.
It’s important to use common sense when exercising after a brain injury. Choose mild exercises that increase your heart rate but that don’t aggravate your symptoms or put you at risk of another injury. The important thing is to keep exercising even if it’s only for five minutes at the beginning. Continue increasing gradually until you feel comfortable exercising for longer periods.

Eating a balanced diet may not be enough by itself, but it can help your cycles return to normal.
Make sure you include fresh fruit and vegetables, fish, meat, and dairy products, and avoid skipping meals, high sugar consumption, strict weight-loss diets, and heavy drinking. Your doctor may also suggest vitamin and mineral supplementation to alleviate painful periods, and probiotics to ensure a healthy microbiome. This approach is proven to reduce pain during your period and keep PMS symptoms under control.
You can read more here about the best nutrition for post-concussion syndrome recovery.
There are many misconceptions around the potential effects of an mTBI on the menstrual cycle. Some of these are even perpetuated by doctors who do not have experience testing for or treating hormone imbalance and menstrual irregularities after a head injury.
Here are two misconceptions your doctor or friends may have said to you:
Yes, they can.
As described earlier, many scientific studies have confirmed that a brain injury can have a severe impact on a woman’s reproductive system, causing symptoms such as irregular and painful periods as well as heavier or lighter bleeding than normal.
At Cognitive FX, we also have first-hand experience with women going through our EPIC treatment program who complain of changes during their menstrual cycle. We’ve seen a number of patients on hormone replacement therapy who were eventually able to stop taking their medications after their menstrual cycles returned to normal. As we’ve said before, our treatment is not guaranteed for irregular cycles, but it can go a long way to help.

If you have a prepubescent daughter who experienced a brain injury, you’re probably not worried about changes to her menstrual cycle. Your doctor may have also said that it’s not important at the moment to look at hormones like progesterone or estrogen. They expect them to sort themselves out eventually.
But what if they don’t? Your daughter’s brain is growing at an astounding rate, and this process needs hormones such as progesterone and estrogen to shape structure and function. If the concussion caused a drop in these hormones, how is the brain going to adapt? More importantly, will it be able to recover in the long term?
Estrogen in particular is vital in young women to stimulate the development of secondary sexual characteristics and build bone mass. Peak bone density is achieved in late adolescence, and it may never be recoverable if the process is hindered by a brain injury. Even in prepubescent girls, early identification of hormonal issues caused by a brain injury is essential to avoid further health problems in adulthood.

It’s important to note that it’s not uncommon for women to experience irregular periods. These changes are not necessarily an indication that there is something wrong, even after a brain injury. For example, periods are often irregular for the first few years after puberty, or if you recently experienced extreme weight loss or weight gain, increased the amount of exercise you do, or are under severe stress.
The best advice we can give you if you’re worried is to track your cycle as best you can, coordinate with your doctor, and focus on rehabilitation from your brain injury. Menstrual changes are often unpleasant, but they may not be permanent. And if they are, there are a number of therapeutic options available to you. Stay focused on recovery, and you will continue to improve.
We specialize in helping post-concussion patients recover from lingering symptoms caused by a brain injury. 95% of our patients show statistically significant improvements by the end of their first week. To discuss your specific injury and symptoms, schedule a consultation with our team of experts.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
.png?height=175&name=image2%20(5).png)
Have you ever caught yourself holding your breath while doing something challenging? Or feeling lightheaded and breathing faster when you stand up after sitting for a long time? Maybe you often have...

What should you do when your concussion symptoms don’t go away?

Severe traumatic brain injury (TBI), concussion (mild traumatic brain injury or mTBI), and other head trauma can cause high blood pressure, low blood pressure, and other circulatory system changes....

Concussions may be the hardest form of traumatic brain injury to treat due to the convoluted nature of long-term symptoms and how those symptoms can be misdiagnosed or even undiagnosed.

If you’ve been struggling with lingering symptoms after a brain injury and even a mild jog is enough to trigger misery, then you might flinch at the idea of high-intensity interval training as a...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY