After a concussion or other brain injury, your loved one may start exhibiting some behaviors that are considered inappropriate and childlike. They may be prone to crying (emotional lability), angry outbursts, impulsive behaviors, and more. It may seem like their words and behaviors are out of character or that they’re failing to understand and respect the feelings of others.
You might feel frustrated with how they’re behaving and wonder why they’re acting so selfishly when it’s been weeks (or months, or even years) after their head injury. But most post-concussion patients are not acting out on purpose. Although it may seem like they have a different personality after the head injury, their personality is likely the same as before. It’s just that their normal pre-injury personality is being hidden by brain changes and symptoms.
Persistent symptoms following a concussion are known as post-concussion syndrome. If your loved one experienced symptoms after a head injury or other source of brain trauma (like transient ischemic attack, acquired brain injury, severe traumatic brain injury (severe TBI), long COVID, carbon monoxide poisoning, etc.), and it’s been at least three months since the injury, then there’s a high chance they have post-concussion syndrome.
The good news is that it’s possible to treat childlike behaviors after a head injury (along with other persistent symptoms). Many PCS patients return to their pre-concussion selves with the right care. However, choosing the proper treatment is not always straightforward. It’s easy to assume psychotherapy/counseling sessions are the best approach to address these behaviors. While talk therapy can help in the short term, it often isn’t enough to achieve full, long-term brain injury rehabilitation.
Most of these emotional symptoms and personality changes are rooted in functional brain changes, autonomic nervous dysfunction, and other long-term effects of concussion. At Cognitive FX, we target these primary, underlying issues directly with a multidisciplinary therapy program designed to treat post-concussion syndrome. Our therapy holistically addresses the cognitive, emotional, and physical effects of brain injury that our patients experience. What we see is that when the physical/functional symptoms improve, behavioral symptoms either improve soon after or are much easier to resolve with talk therapy.
In this article, we’ll cover:
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.
Childlike Behavior Symptoms After a Brain Injury

Numerous PCS symptoms can be described as childlike behaviors. Even patients who seemingly make a “good” physical recovery after a mild head injury may experience some of these behavioral changes. In most cases, patients don’t behave this way on purpose and they aren’t intentionally trying to hurt or upset their loved ones. The reality is that they struggle to regulate their behavior after their brain injury; some may suffer from post-traumatic stress disorder (PTSD). Some are even unaware that their behaviors are inappropriate, which makes it challenging for patients to seek treatment for them.
Common symptoms of childlike behavior after a mild traumatic brain injury include:
- Irritability and aggression
- Impulsivity
- Disinhibition
- Withdrawal and/or self-protective behavior
- Obsessive behavior
- Emotional lability
- Self-centered attitude
- Lack of affection
Irritability and aggression
One of the most common behavioral changes after a head injury is increased irritability and aggression. Patients may become impatient, intolerant, have poor impulse control, and be easily irritated by disruptions to their concentration. This may result in outbursts of verbal or physical aggression.
Impulsivity
Patients with a head injury may speak or act impulsively, without thinking about the possible consequences of their behavior. This may include inappropriate comments about other people, which may lead to embarrassment in social situations and upset the person they are speaking about. Patients may also agree to tasks that they cannot complete or spend money they don’t have.
Disinhibition
PCS patients may also experience excessive disinhibition, which can result in socially inappropriate behavior. This may include, for example, talking too freely about sensitive information, being overly familiar with acquaintances, using crude language, and experiencing outbursts of uncontrolled rage.
Withdrawal/self-protective behavior
Patients are often so overwhelmed by PCS symptoms that they only have the bandwidth to consider their own needs and care for themselves. This may make them oblivious to others' feelings or perspectives, and their behavior can easily be mistaken as egocentric by someone who doesn't understand the real burden of PCS symptoms. Unfortunately, PCS is an "invisible" illness, and it's easy for people to misunderstand self-protective behaviors as callous or self-centered.
Obsessive behavior
PCS patients may become obsessive or fixated on certain behaviors after a brain injury. For example, they may want to follow a particular routine or do specific things in a certain way and feel scared and angry if it doesn’t happen that way. These issues are due to a reduced cognitive flexibility caused by the concussion. Under normal circumstances, cognitive flexibility allows people to change between different tasks and apply what they’ve learned in one field to solve problems in another field. With low cognitive flexibility, PCS patients get “stuck” on certain thoughts and behaviors. They are likely unaware of the change and unable to control it.
Emotional lability
In some cases, brain damage may cause emotional lability, where patients exhibit intense mood swings or extreme reactions to everyday situations. This may include sudden tears, angry outbursts, or exaggerated laughter, which may not actually express how the patient is feeling or may be much stronger than they would otherwise exhibit.
Lack of affection
Family members of PCS patients often report that their loved one seems less interested in what the rest of the family is doing or the activities they once liked. Patients may prefer not to engage with family members and appear apathetic or indifferent to what’s happening around them. They may not show emotion through facial expressions. This behavior could have several causes. It may be that their brain injury greatly diminished their ability to feel or register emotions. It also may be a sign of depression.
What Causes Childlike Behavior After a Brain Injury?

Childlike behavior after a brain injury can be the consequence of different factors, including:
- Structural damage to the frontal lobe
- Neurovascular coupling dysfunction
- Autonomic nervous system (ANS) dysfunction
- Overstimulation
- Cognitive changes
Structural Damage to the Frontal Lobe
Patients can develop behavioral changes — including childlike behaviors — if an area in the brain called the frontal lobe is affected. This area controls reasoning, problem-solving, executive function, empathy, impulsivity, and other neuropsychological traits.
If damaged by the concussion, patients lose self-control, which may result in the type of behaviors described above, including poor decision-making and reckless behavior. This area is one of the last areas of the brain to fully develop, not reaching fully mature status until age 25. This explains why children and adolescents think and act differently compared to adults: Their frontal lobes are not mature yet. If adults sustain a concussion that directly affects their frontal lobe, childlike behaviors may return because the frontal lobe is no longer fully operational.
Neurovascular Coupling (NVC) Disruption
The frontal lobe can also be affected indirectly if a mechanism in the brain called neurovascular coupling (NVC) is disrupted. Under normal circumstances, brain cells receive the resources they need from a network of blood vessels in the brain. After a concussion, this connection can be disrupted such that the brain struggles to complete normal functions. If this happens in the frontal lobe, it may trigger behavioral changes, including disinhibition and irritability.
Dysfunction of the Autonomic Nervous System (ANS)
The autonomic nervous system regulates a variety of (mostly) involuntary processes throughout your body, such as heart rate, blood flow, breathing, digestion, and physiological threat response.
Two major subsections of the ANS are the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS represents the “fight or flight” part of the nervous system and prepares your body to react to a threat, while the PNS is the “rest and digest” part of the nervous system, and it helps your body to calm down. Under normal circumstances, these two sections work in harmony and change dominance as needed.
After a concussion, this balance is disrupted, and the SNS remains activated even when it’s not needed. In addition to physical symptoms, such as fatigue, headaches, digestive issues, and problems sleeping, ANS dysfunction can trigger behavioral changes.
Under normal circumstances, the PNS helps patients cope with frustrating situations. When faced with a challenge, the PNS helps the brain engage and adapt to the situation calmly. For example, when playing a computer game, if a person can’t complete a level, they will increase focus in the hopes that this increased attention will help them succeed.
PCS patients, however, have limited PNS activity. As a result, they cannot regulate their emotions so easily and struggle to focus when presented with a challenging or frustrating situation. Inevitably, they feel overwhelmed and overstimulated, and activities that wouldn’t normally be a problem become a problem. For example, they may feel like losing their temper was an acceptable response to being called for dinner two or three times when they were trying to read. In reality, this was not normal behavior, but the effort needed to shift attention away from the reading to going for a meal was too overwhelming, most likely because the brain was under a lot of stress already.
Overstimulation (and Frustration)
PCS patients often experience dramatic changes in their daily lives and may no longer be able to get involved in activities they once enjoyed, like playing sports or going out with friends. Emotional outbursts can come out because the brain is not screening and processing information in the normal way.
Here’s an illustration of how that might happen…
Let's say you are a parent and you want to take your child to the playground. Initially, it’s a cloudy day and no one else is at the playground, so it’s quiet and tolerable. Then the sun comes out (so bright!) and a few more families show up (more kids yelling and screaming). You start to develop a headache and anxiety. Two of the parents nearby strike up a conversation and it’s more than you can take. You feel the need to retreat to a quieter place ASAP because the bright light and multiple auditory stimuli are not being filtered correctly by your brain.
You call for your kid and they don't come right away. But your feelings of desperation are mounting. Why can’t they just come when they’re called? Instead of being patient, you yell at them and get angry in front of everyone instead. (Alternatively, you might burst into tears out of frustration for how you feel and not even understand why you're crying.) Now you feel crummy, your kid feels crummy, and the incident adds an emotional layer of frustration and feeling guilty on top of your poor brain just needing to rest.
For anyone who has experienced overstimulation, these feelings and scenarios will sound painfully familiar. Common triggers for emotional outbursts include:
- Too much sensory input
- Pain
- Fatigue
- Low glucose (sugar) levels
- Hunger
- Unrealistic goals and expectations
- Lack of independence or control
Cognitive Impairments
Cognitive issues, such as problems with focusing, thinking, or communicating, are very common after a concussion or other brain injury. These memory problems and other cognitive issues can make it hard for patients to follow a conversation or understand a particular situation. As a result, PCS patients may appear disinterested, uncooperative, and “out of sync” with what is happening around them. If this is pointed out to them, they may overreact with aggression, withdraw even further, and/or avoid social interactions because they feel uncomfortable or embarrassed.
Treatment at Cognitive FX
![EPIC Treatment exercise with headphones [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg?width=2265&height=1425&name=EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg)
At Cognitive FX, we offer a combination of exercise and multidisciplinary therapies to address underlying PCS symptoms caused by brain injury, including ANS dysfunction and neurovascular coupling disruption.
Before treatment starts, patients must complete an extensive medical evaluation, including:
- A review of their medical history,
- An inventory of past and current symptoms
- Physical, cognitive, and emotional assessments
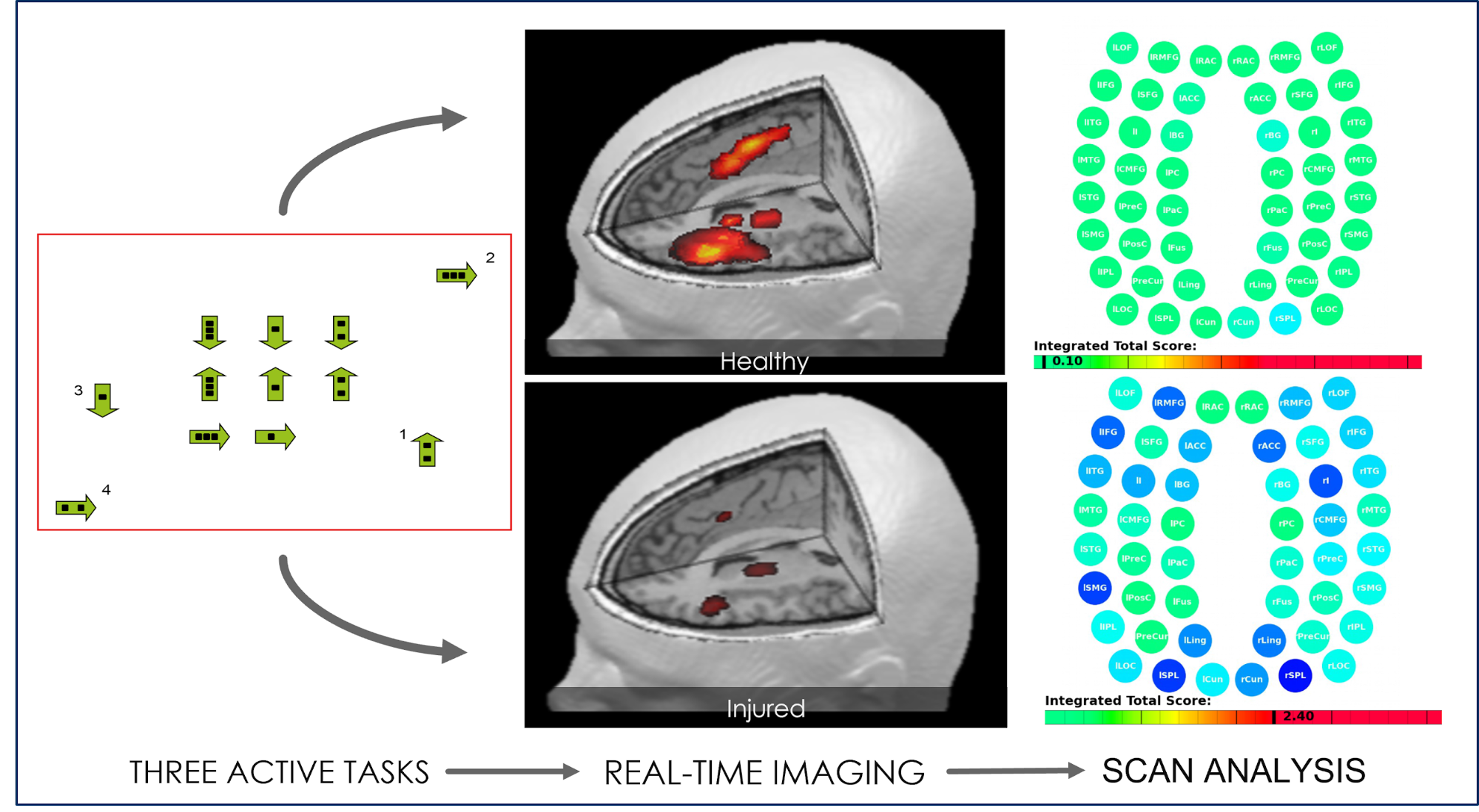
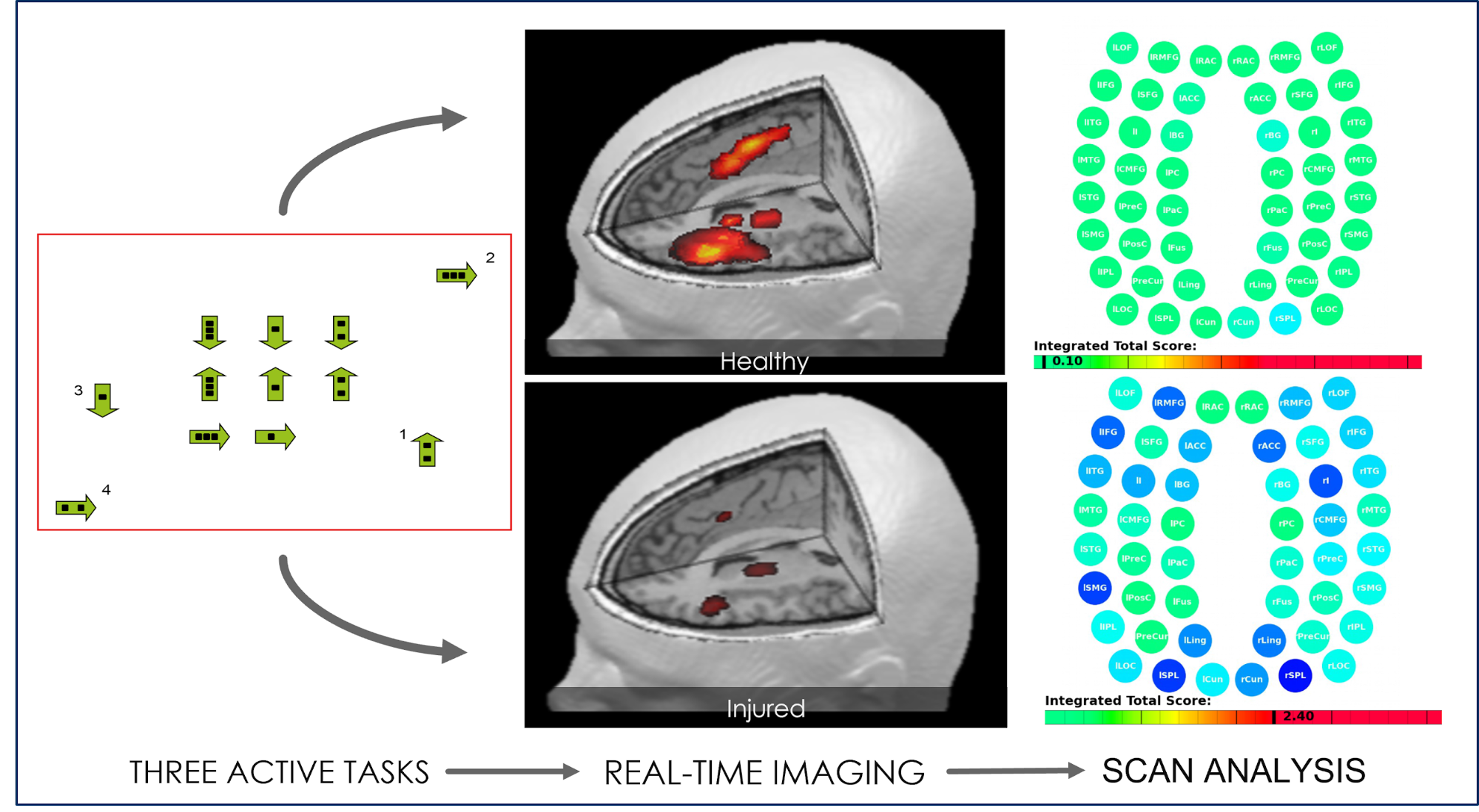
Patients also undergo a brain imaging scan. This scan — called a functional Neurocognitive Imaging (fNCI) scan — investigates how the patient’s brain is working in 100 regions of the brain (including the frontal lobe) and checks how effectively these regions are communicating with each other.
During the scan, patients complete a series of standardized cognitive tasks to trigger activity in different areas of the brain. This scan is a crucial part of our treatment. It tells us exactly where (and in what way) the patient’s brain was affected by the brain injury and allows us to design a personalized treatment plan for each patient.
Treatment involves a repeated three-step cycle:
The first step, Prepare, involves short sessions of aerobic exercise intervals, usually on a stationary bike or treadmill, to promote healthier blood flow in the brain. Physical activity triggers the release of different neurochemicals, including a compound called brain-derived neurotrophic factor (BDNF). BDNF enhances the impact of subsequent therapies and helps the brain learn and adapt to changes.

During the second step, Activate, patients engage in a series of therapies to treat their physical, cognitive, emotional, and behavioral symptoms. Therapies include occupational therapy, neuromuscular therapy, neurointegration therapy, cognitive therapy, sensorimotor therapy, vision therapy, vestibular therapy, and others.

While the overall list of therapies offered to each patient is similar, specific exercises and how they’re combined can vary considerably from patient to patient. These combinations are closely tailored to each person’s brain injury and evaluation results.

Using this approach, we have seen many success stories over the years. We acknowledge that most patients do not recover 100% at the end of their treatment (one to two weeks) with us, but they experience significant and life-changing improvements and continue improving at home.
If, at the end of treatment, our team feels patients need further therapy, we can make appropriate recommendations for follow-up with the appropriate specialists.

Finally, patients need the third step, Recover, to relax and rest in between therapy sessions. This may include breathing exercises to promote relaxation, neuromuscular massage of the neck and shoulders, and mindfulness exercises.
At the end of the treatment, patients complete a second scan to check how their brains are recovering. In addition, patients meet with a member of our team to discuss progress and receive a series of “homework” exercises. These typically include aerobic exercises, cognitive activities, and relaxation techniques.

We recommend that patients spend about one hour five days per week on exercises at home. As their symptoms improve and their stamina grows, they can slowly reduce the time spent on these exercises. This at-home continuation of your treatment provides the best chance of a fast and complete recovery after your time with us.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in the long-term symptoms of head injury. To see if you are eligible for treatment, sign up for a consultation.
Additional Ways to Treat Childlike Behavior

Addressing the root of the problem — like the treatment we offer at Cognitive FX — is the most effective approach for patients. However, some patients may benefit from further treatments, like psychotherapy and medication.
It’s important to note that although cognitive behavioral therapy and anger management sessions, for example, can help patients manage their behavioral and emotional problems, these treatments don’t address the underlying brain dysfunction driving PCS symptoms, such as vision problems, headaches, and dizziness.
Talk Therapies
Talk therapies involve talking to a trained mental health professional, such as a counselor, neuropsychologist, or psychotherapist. These medical providers can help you explore the causes of behavioral changes and find ways to manage them. Two helpful forms of talk therapy are cognitive behavioral therapy and counseling:
- Cognitive behavioral therapy (CBT) is a structured therapy where therapists help you understand how your thoughts and feelings trigger certain behavior problems. The aim is for patients to develop strategies to control the way they react to triggers and to develop healthier thought patterns. This can be especially effective for patients exhibiting childlike behaviors related to difficulties in adjusting to life after a brain injury.
- Counseling is a treatment where you can talk to a therapist about a specific issue to find ways to deal with it. For example, it may help patients who have outbursts of anger with family members at home or inappropriate behavior in the workplace.
Anger Management Therapy
Anger management therapy may suit PCS patients with aggressive symptoms and outbursts. This type of therapy aims to help patients develop healthier alternatives to angry outbursts and learn to control their behavior.
Anger management sessions help patients find what triggers their emotional responses and learn effective coping techniques for situations where anger may be a problem. Typically, therapists role-play different scenarios, such as dealing with colleagues at work or challenges living with a partner and family at home, and help patients find ways to deal with anger issues that may arise in these situations.
Medication
Patients should always exercise caution with medication for post-concussion symptom management. PCS patients are more likely to have negative experiences with medication than their non-brain-injured peers. We recommend that you read about the pros and cons of medication with PCS before continuing.
That said, patients with behavioral and emotional symptoms have some options. This is particularly true if talk therapy alone is not helpful. If you decide to try meds, work closely with your doctor and reassess your diagnoses and prescription on a regular basis, as doses may need to be adjusted over time.
Meds should never be seen as a stand-alone treatment; they need to be part of a more comprehensive treatment plan. They should only be used as a last resort for patients as they’re usually associated with multiple side effects and can make some symptoms worse.
How Patients Can Cope with Emotional and Behavioral Symptoms

As the brain heals, patients start to regain the ability to control their behavior. However, recovery may take some time. Here are some strategies PCS patients can use to cope with childlike behavior during this time:
- Take a break: When you feel that you are beginning to get agitated or frustrated, walk away from the situation and go to a safe space where you can relax. This will help your brain destimulate, making it easier for you to regain control over your emotions.
- Acknowledge the loss: Brain injuries can change how you feel and behave. You may have had to stop working or quit your sport, at least while you recover. Acknowledging what you’ve lost is a vital step in your recovery.
- Reach out to others: Never be ashamed or afraid to ask for help and support when you need it. Talk to friends and family about your difficulties controlling your behavior. They may be able to help you recognize what triggers challenging behavior and help you learn how to avoid those triggers.
- Apologize: Even though you know your behavior was not intentional, it goes a long way with friends and family if you apologize to them. This also gives you an opportunity to share how you feel and why you are behaving this way.
- Seek professional help: The best way to cope with this type of behavior is to seek professional medical care. As we’ve described before, this may include receiving treatment at Cognitive FX, as well as counseling and psychotherapy.
- Rest: Take frequent breaks during the day. If you decide to take a nap, keep it to about 20–30 minutes shortly after lunch to make sure it doesn’t interfere with your nighttime sleep.
- Diet and exercise: Engaging in regular exercise and eating a healthy and balanced diet can help your brain heal faster. In addition, it also reduces aggressive behavior and improves mood.
- Practice mindfulness: Take time each day to engage in self-care and mindfulness activities. This could be going for a short walk, doing yoga, or meditating. Even just a few minutes every day doing an activity you enjoy can help you feel more controlled throughout your day.
- Journal: Journaling can help you process emotions on your own and gives you a way to look at your progress over time.
- Join a support group: You may have supportive family and friends, but it may still be helpful to connect with other PCS patients. Meeting other patients in similar circumstances in a support group can be encouraging and uplifting during your recovery.
- Be patient: Finally, be patient with yourself while you recover. While there will be bad days, that does not make you a bad person, and recovery is possible.
Patient recovery story: Read how lawyer Anthony Loubet overcame emotional symptoms, cognitive difficulties, and more after a car accident concussion left him with lingering symptoms.
How Families Can Help Patients with Emotional and Behavioral Symptoms

Behavioral and emotional changes can be difficult for PCS patients to deal with alone, especially when they find it challenging to implement effective coping mechanisms by themselves. It is so important for caregivers and loved ones to help and support patients during this stage.
Here are some helpful tips to assist with challenging behaviors:
- Create a peaceful environment at home: A peaceful and quiet environment at home is ideal to lessen exposure to potential triggers for PCS patients. This also gives family members a better chance to diffuse a situation before it escalates.
- Walk away: Family members should avoid arguing with the patient during an outburst. If possible, they can try to negotiate an alternative solution or redirect the patient’s attention to another activity. If this strategy doesn’t work, the best option may be to walk away and give the patient time alone. This allows the patient to release their emotions and process the situation.
- Use various techniques to help the patient calm down: In some cases, the best way to deal with childlike behavior is to help the patient calm down. Family members can use many different techniques, including breathing techniques (which our therapists teach during treatment at Cognitive FX), listening to soft music, meditation, or simply asking the patient to sit down and close their eyes to destimulate.
- Don’t criticize: Don’t criticize or make fun of the patient’s deficits. Respect is key. Patients may be acting out but most likely cannot control their behavior and feel bad about the situation.
- Acknowledge the patient’s feelings: Once the situation has de-escalated and the patient has calmed down, it’s important that family members acknowledge their feelings. This is the best way to avoid frustration, anger, and embarrassment.
- Plan for future situations: Family members and patients should discuss how to deal with future outbursts. For example, instead of yelling at each other, family members can suggest that the patient use a punching bag to release energy or a journal to write their frustrations.
- Join a support group or seek personal counseling: If family members struggle to cope with the patient’s behavior, joining a support group or even seeking counseling can be very helpful.
- Teach the rest of the family: The whole family needs to establish consistent and non-confrontational ways to deal with the patient. Even the younger members need to learn some “dos” and “don’ts” when interacting with their loved ones with PCS.
- Set strict rules at home: It is very important to establish rules at home, including behaviors that are not acceptable at home, such as cursing or being aggressive to other family members. Patients may need to be reminded about these rules on a regular basis. In this case, consistent, positive reinforcement is key to reestablishing boundaries.
- Monitor triggers: Patients may not be aware of what triggers their symptoms, but family members can help. For example, if noise and overstimulation trigger childlike behaviors, family members can advise shopping during quieter hours and avoiding busy roads.
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.



![EPIC Treatment exercise with headphones [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg?width=2265&height=1425&name=EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg)