Brain Damage from Carbon Monoxide Poisoning | Cognitive FX
If you speak to him today, you’d never be able to guess that Nathan “Nate” Benson is a brain injury survivor. The Bountiful, Utah native is in his final year of undergraduate school for a...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Still feeling "off" months after carbon monoxide exposure? You're not imagining it.
If you've been told your CO levels are back to normal but you're still battling brain fog, crushing fatigue, memory problems, or mood changes, you're experiencing what happens to up to 46% of CO poisoning survivors. It's called delayed neurological sequelae, and here's the frustrating truth: there is no established treatment protocol in conventional medicine for these long-term symptoms.
Most doctors focus on the acute crisis. They'll give you oxygen therapy, monitor your carboxyhemoglobin levels, and send you home once your bloodwork looks normal. But CO poisoning doesn't just starve your brain of oxygen temporarily. It triggers inflammation, damages the protective coating around nerve fibers, and disrupts how your brain regulates blood flow to different regions. These changes can persist for months or years, long after the gas is gone.
The good news? Your brain can recover. At Cognitive FX, we specialize in treating the persistent neurological symptoms that conventional medicine overlooks. Our approach targets the underlying dysfunction, not just the symptoms, using a combination of aerobic exercise and multidisciplinary therapies that have helped patients like Nate Benson reclaim their lives after years of struggling with CO-related cognitive problems.
In this article, we:
Your blood tests came back normal. So why do you still feel so wrong?
Oxygen therapy addresses the immediate crisis. But what about the brain fog, memory problems, and fatigue that persist for months or years afterward?
Select any symptoms you're currently experiencing:
Select symptoms above to see analysis.
CO binds to hemoglobin 250x more effectively than oxygen, starving your brain of the oxygen it needs to function properly.
The connection between brain activity and blood flow (neurovascular coupling) becomes dysfunctional.
The protective coating around nerve fibers (myelin) is particularly vulnerable to CO toxicity.
CO triggers inflammation and oxidative stress that can continue damaging brain tissue even after exposure ends.
We treat the persistent neurological symptoms that conventional medicine overlooks by targeting the underlying brain dysfunction.
Schedule Free ConsultationIf you’re experiencing persistent symptoms such as brain fog, fatigue, memory problems, vision changes, and more after CO exposure, you’re not crazy. These are real symptoms caused by changes in the brain and autonomic system after exposure, and they can be helped. Over 90% of our patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.
Most of the initial symptoms of CO poisoning are subtle and nonspecific. Mild cases often go unrecognized, as symptoms can be mistaken for many other illnesses. As a general rule, as the level of CO in the blood increases, so does the severity of symptoms.
In this article, we’ll cover symptoms that occur:
Acute CO poisoning refers to cases where patients experience significant symptoms after exposure. This typically occurs after a single, large exposure to the gas.
At low levels, headache is the most common symptom of acute carbon monoxide poisoning; patients often describe it as dull but constant. In addition to headaches, some patients may experience fatigue, nausea, and dizziness. At this stage — if patients are not aware of their exposure to CO — it can be difficult to separate between being exposed to carbon monoxide and other common illnesses.
Increasing CO exposure may lead to cardiac problems, including fast heart rate, low blood pressure, chest pain, and cardiac arrhythmia. Patients may also experience short-term symptoms affecting their central nervous system, such as delirium, hallucinations, drowsiness, dizziness, unsteady gait, confusion, seizures, and central nervous system depression. Ultimately, severe poisoning can cause loss of consciousness, respiratory arrest, and death.
In contrast to acute poisoning, chronic CO poisoning refers to cases where patients are exposed multiple times to CO, usually at low concentrations.
The most common symptoms of chronic CO poisoning include persistent headaches, lightheadedness, fatigue, memory problems, nausea, hearing disorders, sleep disorders, abdominal pain, diarrhea, and vomiting. Each time a patient is exposed to CO, they will develop one or more of these symptoms. However, because most are nonspecific symptoms, CO poisoning is difficult to recognize and is frequently mistaken for a flu-like disease or a stomach bug.
Irrespective of whether patients were exposed to acute or chronic CO poisoning, they can develop persistent symptoms even after the source of CO is removed. These symptoms occur in up to 50% of all patients who sustained toxic levels of CO.
This is what happened to Nate Benson, one of the patients treated at Cognitive FX for CO poisoning. Nate was exposed to low levels of CO in his home for over three years. The leak in the furnace was eventually detected, but Nate continued to experience persistent symptoms for years, including brain fog, difficulty remembering information, headaches, and depression. Eventually, his family found Cognitive FX, where Nate received treatment.
After just one week, Nate was a different person. “When I left the clinic, I was happy! I felt motivated. A lot of that was thanks to the therapists encouraging me. I did feel sharper. I felt way quicker. My reaction time and my ability to process things was faster,” he recalled. Read more about Nate’s recovery story and how his time at Cognitive inspired a career change.
Similarly to what happened to Nate, up to 30% of patients exhibit some degree of cognitive decline after CO poisoning. This ranges from subtle impairments that most patients don’t even notice to a significant reduction in intellectual function or even dementia. It’s common for patients to experience deficits in attention, concentration, memory, executive function, and verbal fluency.
Physical and movement disorders can affect about 13% of patients. Symptoms include balance issues, rigidity, and shuffling gait. Urinary and fecal incontinence is also a common problem in severe cases.
Finally, emotional and behavioral disturbances are less common and can be difficult to distinguish from pre-poisoning disorders, particularly in cases of suicide attempts by CO poisoning. Personality changes may occur, and studies have described patients suffering from depression, anxiety, and irritability several years after CO poisoning.

It’s impossible to determine exactly how CO poisoning causes symptoms in each person, but a mixture of multiple resultant mechanisms affecting the brain can include:
Neuroimaging studies show that CO poisoning can cause lesions throughout the brain, with certain regions — including the hippocampus and hypothalamus — being particularly vulnerable.
Researchers don’t know the exact mechanism behind this damage, but some studies suggest it may be caused by oxidative stress. There is some evidence that CO poisoning increases the production of free radicals in the brain, which in turn affects how brain cells work.
In addition to direct damage, CO poisoning also causes the brain to be starved of oxygen and other resources. Neurons receive oxygen and nutrients via a network of blood vessels. In a healthy brain, when different areas need resources to complete a task, surrounding blood vessels deliver what they need. This dynamic mechanism is called neurovascular coupling (NVC).
However, CO replaces oxygen in red blood cells and reduces the amount of oxygen in the blood flow reaching the brain, disrupting this connection. As a result, affected areas may not receive the right amount of resources at the right time for them to perform their tasks normally. NVC dysfunction is very taxing on the brain, frequently leading to headaches, fatigue, and irritability. In addition, you may experience different symptoms related to the areas of the brain that were affected (such as vision problems when regions associated with visual processing are harmed).
Low levels of oxygen in the brain — caused by CO poisoning — can also affect the autonomic nervous system (ANS). The ANS controls many body functions, including heart rate, blood pressure, and breathing rate via the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
In simple terms, the SNS represents our “fight-or-flight” response when we’re stressed, and the PNS is responsible for our “rest-and-digest” mechanisms by bringing everything back down with a calming influence.
Under normal circumstances, both sides work together in harmony. However, low levels of oxygen often cause the SNS to stay activated most of the time. The constant effort leads to a series of symptoms such as fatigue, headaches, high blood pressure, digestive issues, problems sleeping, and mood changes.
CO poisoning may also lead to hormonal problems, most likely due to damage to the brainstem and hypothalamus.
For example, adrenal glands (located on top of the kidneys) produce multiple hormones, including cortisol, adrenaline, and testosterone. The production of these hormones is regulated by the hypothalamus and pituitary gland in the brain. Anything that affects normal functioning in these areas — including CO poisoning — may cause hormonal problems and symptoms such as fatigue, muscle weakness, nausea, vomiting, dizziness, joint pain, and irritability.

Many patients experience chronic neurocognitive and physical symptoms long after the source of CO is eliminated.
To further complicate matters, these patients often struggle to find the medical care they need. It’s easy for the long-term effects of carbon monoxide poisoning to be mistaken for other conditions, such as psychiatric conditions or stroke, and patients often get lost in the system and never receive the treatment they need.
This is where Cognitive FX comes in. If you believe that you’re experiencing persistent symptoms due to CO poisoning, we offer a combination of aerobic exercise and a variety of therapies — such as cognitive therapy, vestibular and vision therapy, and sensorimotor therapy — as an effective treatment option.
Before treatment, all patients need to complete a detailed medical examination. This includes a review of their medical history, past and current symptoms, as well as exams to assess the patient’s physical, cognitive, and emotional condition.
All patients undergo a functional Neurocognitive Imaging (fNCI) scan. This brain imaging scan assesses neural functioning in about 100 regions of the brain and checks how effectively these regions communicate with each other while the patients perform a series of cognitive tasks.
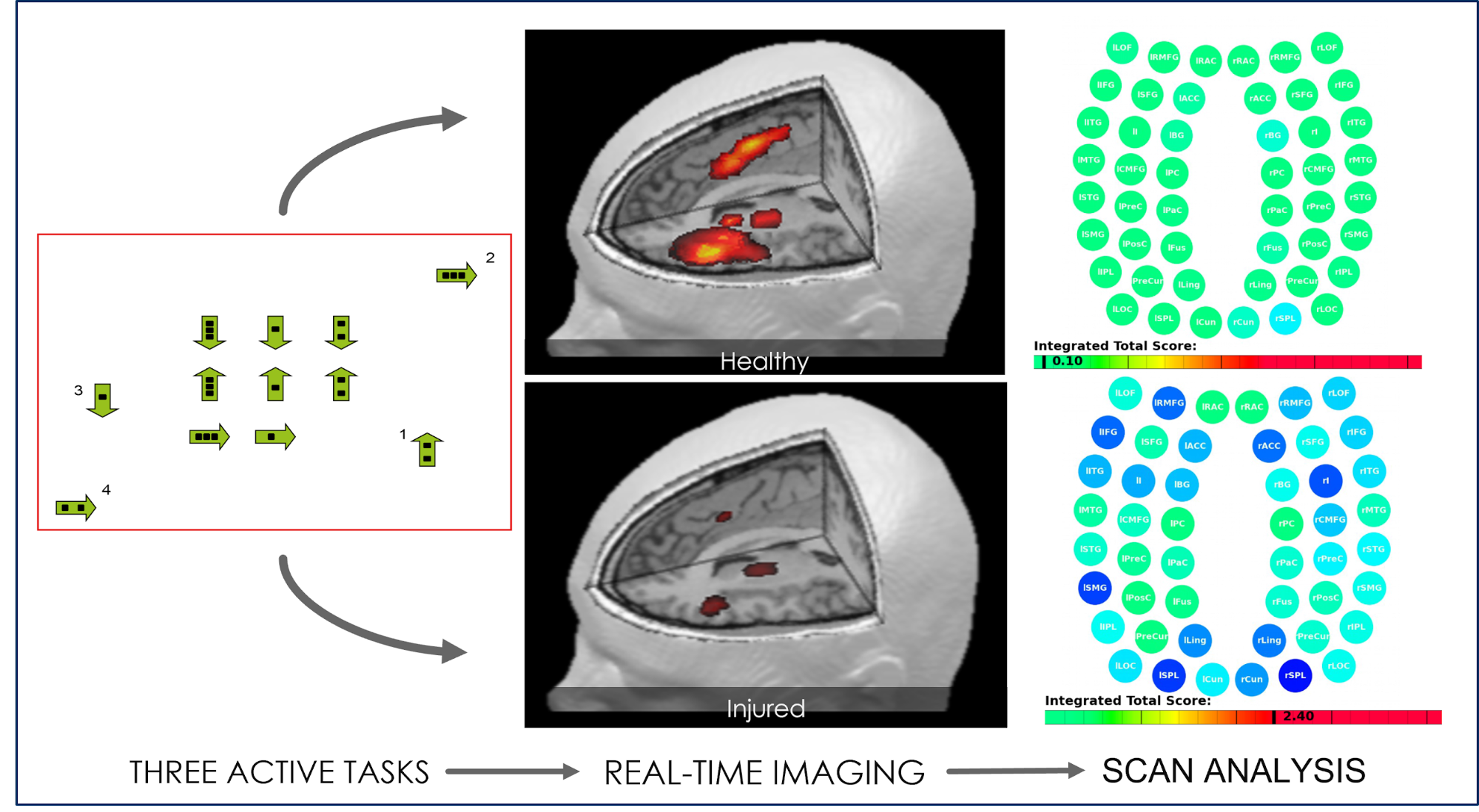
Once these exams are completed, our team will gather all the results and design a treatment plan specific for each patient. For example, we know that CO poisoning affects the cardiac system and that these patients are therefore more likely to experience exercise intolerance. Our therapists are trained to find ways to work around this issue.
Treatment involves a three-step cycle that is repeated multiple times a day: Prepare, Activate, and Recover. The main goal is to restore neurovascular coupling, improve ANS function, and reduce the incidence and severity of symptoms after carbon monoxide exposure.


After treatment, patients go through a second scan to check how their brains are recovering. Patients meet with one of our therapists to discuss progress and receive a series of exercises to complete at home. These typically include aerobic exercises, cognitive activities, and relaxation techniques.
Most patients start with about an hour per day, five days a week on these exercises, then slowly reduce the time spent as they recover. Completing these exercises boosts the chances of a fast and complete recovery. Most patients continue to improve at home in the weeks and months after their treatment.
This was certainly the case with Nate Benson. In the months after his treatment, his energy levels increased, he could focus while studying, and his mental health improved significantly.
Since his treatment, his mom and brother have also undergone treatment at Cognitive FX. In fact, his brother’s initial condition was even worse than Nate’s because he suffered multiple concussions growing up. He too saw significant improvements in his symptoms.
In addition to CO poisoning, we also treat a variety of other conditions that affect the brain. Some of our patients include:
Ready to start your recovery journey at Cognitive FX? Schedule a consultation with our team.

In this section, we address the following common questions:
Carbon monoxide poisoning occurs when carbon monoxide (CO) builds up in the bloodstream. When people inhale too much CO, this gas reaches the bloodstream through the lungs and attaches to the body’s oxygen transporter — called hemoglobin — present in red blood cells. The problem is that CO can bind 200 to 250 times more effectively than oxygen to hemoglobin. After CO exposure, red blood cells start carrying CO, and the body is effectively starved of oxygen.
This colorless and odorless gas is produced during the incomplete burning of organic matter. (Complete combustion would produce carbon dioxide - CO2.) Any burning fuels, including gas, wood, propane, or charcoal, can produce carbon monoxide.
Most accidental exposure to CO happens in the winter. The most common source of CO poisoning is space heaters in the home. If these devices are not installed properly, they can release CO into the room. Placing these heaters in a tightly enclosed space makes the buildup worse.
Other sources of carbon monoxide include the following:
Everyone can be affected by carbon monoxide poisoning, but patients with the highest risk include:
Diagnosis is possible if patients seek medical treatment immediately after exposure. In practical terms, this is done by measuring the amounts of hemoglobin connected to CO (called carboxyhemoglobin) compared to the amount of hemoglobin connected to oxygen in the blood.
In an average person, the ratio between carboxyhemoglobin and hemoglobin molecules is around 5%, although it may be double in heavy smokers. Levels can reach 30% after mild exposure, with fatal cases going as high as 90%.
However, diagnosis is not always this straightforward. The body can eliminate CO within a few hours after exposure, and the patient’s ratio between carboxyhemoglobin and hemoglobin quickly goes back to normal values. This does not mean that the patient is not experiencing symptoms caused by exposure to CO.
To further complicate matters, symptoms may develop immediately after exposure or may be delayed and only develop weeks or even months after the CO poisoning. This period — called the lucid period or lucid interval — makes diagnosis extremely challenging.
Symptoms and potential exposure — not carboxyhemoglobin levels — should guide diagnosis. Medical staff should be particularly aware of CO poisoning in fire victims, patients with unexplained altered mental status, or if more than one person in the household is experiencing similar symptoms.
Anyone exposed to carbon monoxide needs to get fresh air and seek medical care. If you believe you or your loved ones have been exposed to high levels of CO and are experiencing symptoms like headache, dizziness, nausea, shortness of breath, weakness, and confusion, you need to call emergency medical services immediately.
At the hospital, treatment for CO poisoning may involve:
If you suspect that you’ve suffered carbon monoxide poisoning (or actually have been diagnosed), most likely, it happened at home or in a familiar environment. Follow these recommendations to prevent further accidents affecting you or your family in the future:
If you’re experiencing persistent symptoms such as brain fog, fatigue, memory problems, vision changes, and more after CO exposure, you’re not crazy. These are real symptoms caused by changes in the brain and autonomic system after exposure, and they can be helped. Over 90% of our patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

If you speak to him today, you’d never be able to guess that Nathan “Nate” Benson is a brain injury survivor. The Bountiful, Utah native is in his final year of undergraduate school for a...

If you’re experiencing memory issues after a head injury, you are not alone.

Oxygen is good for the brain. A lack of oxygen is bad for the brain. So is getting more than normal levels of oxygen better for the brain?


Loss of taste and smell featured heavily in the news during the COVID-19 pandemic as one of the first signs of infection. But this is not the only condition that may lead to loss of smell. You could...

Severe traumatic brain injury (TBI), concussion (mild traumatic brain injury or mTBI), and other head trauma can cause high blood pressure, low blood pressure, and other circulatory system changes....
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY