How to Tackle Post Traumatic Brain Injury Syndrome
“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Loss of taste and smell featured heavily in the news during the COVID-19 pandemic as one of the first signs of infection. But this is not the only condition that may lead to loss of smell. You could also experience this symptom after a traumatic brain injury (TBI), whether it was a mild TBI (concussion) or a severe head injury.
Unfortunately, many patients with changes in smell or taste after a head injury struggle to (a) obtain a diagnosis and (b) receive meaningful treatment. Part of the issue is that treatment providers may have to focus their attention on other symptoms; in the wake of a life-threatening TBI, changes in smell and taste are seen as relatively mild symptoms compared to issues such as dizziness, post-traumatic headaches and migraines, or serious digestive issues.
On the other hand, concussion patients often fail to receive a diagnosis because many doctors are not aware that a mild head injury can cause changes in smell and taste.
And in both cases, finding treatment is difficult. There aren’t many options available, and whether or not they will help depends on what part of your olfactory system is damaged. But pursuing treatment when possible is still important. Loss of smell and taste may not appear serious on paper, but these changes make a big difference in your enjoyment of everyday activities. Changes in smell and taste can lead to excessive weight loss, withdrawal from social activities, and depression.
At Cognitive FX, we offer a multidisciplinary approach designed to look at brain injury recovery as a whole instead of treating each symptom as its own issue unrelated to the others. Over 90% of our patients experience improvement in a wide range of symptoms such as brain fog, dizziness, headaches, fatigue, poor sleep quality, emotional changes, and more.
We can’t promise you a cure for loss of taste and smell after a concussion, but we can promise that we’ll offer appropriate therapies when possible. Certain causes of these symptoms are irreversible with current medical technology, while others are treatable. Of the patients we’ve treated who did suffer from changes in smell and taste, some recovered partially, some recovered completely, and others experienced no change.
In this article, we’ll explain what may be causing your loss of smell and taste and when treatment may help. We’ll answer questions, such as:
Over 90% of our patients experience symptom improvement after just one week at our clinic. We target injured brain regions as identified on the fNCI, a brain imaging scan that looks at 56 brain regions and their communication patterns. To see if you are eligible for treatment, sign up for a consultation.
Yes, a concussion or more severe head injury can affect your sense of smell and taste. Loss of smell and taste are less-common symptoms that can be quite demoralizing. After all, your senses — smell, vision, hearing, taste, and touch — allow you to connect to the world around you. If you remove two of the five senses, 40% of your sensory input is gone.
Post-concussion smell disorders can include:
People who lose their sense of smell often lose their sense of taste as well. This is because the olfactory area in your nose is involved with both senses. When you eat, odor molecules from the food reach the back of your nose. Your taste buds can tell you if a food is sweet, sour, bitter, salty, or savory (umami), but it's your nose that figures out the specifics. For example, your mouth may recognize a sweet taste, but it’s your nose that will help you identify that you’re eating a sweet orange. If you plug your nose when you’re eating, food will not taste the same.
Taste disorders include:
Studies show that up to half of patients with a mild brain injury will lose their sense of smell and taste in the first few days after the injury. This is often unreported as most patients are not even aware of it unless they’re tested explicitly regarding their sense of smell and taste. Olfactory dysfunction after a concussion is not associated with symptom severity, but it is associated with a higher risk of anxiety and longer-term post-concussion symptoms.
Many of these patients regain their sense of smell and taste within six months of the injury. But for some patients, loss of smell and taste lingers for months or even years, often accompanied by a variety of other symptoms, such as headaches, brain fog, and difficulty concentrating. If your symptoms last longer than three months and cannot be explained by any other condition, then you may have post-concussion syndrome (PCS).
If you’re in this situation, our advice is to seek treatment for post-concussion syndrome. At Cognitive FX, we offer state-of-the-art diagnosis and treatment for PCS patients. Although we do not target loss of smell and taste in particular, many of our patients experience significant improvements after a week with us, which we’ll discuss later in the article.
Further reading: Recovering from post-concussion syndrome

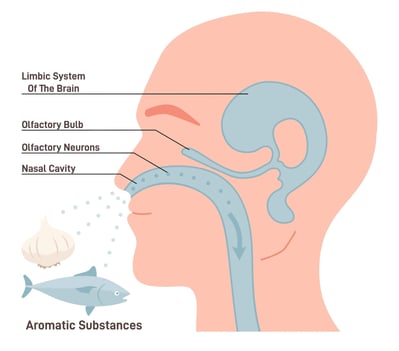
Under normal circumstances, as you breathe in, air enters your nasal cavity and reaches millions of nerve endings capable of detecting different chemicals. These olfactoryneurons then carry information to the brain via the olfactory nerve for processing. Taste works in a similar way — when you eat, different foods touch the taste receptors located on your tongue. These receptors then send that information to your brain. This process relies heavily on areas of the brain dealing with memory, learning, and emotion, and allows you to recognize different tastes and smells.
Diagnosing the cause of changes in olfactory function after a TBI is very difficult. Not everyone will receive a clear diagnosis, even with the best technology in play. Loss of or changes in smell and taste can stem from one or more of the following possible causes:
Head trauma — especially direct hits to the face — can cause serious damage to the nasal passages and pull or twist the olfactory nerve. For example, if the cribriform plate (a bone located directly behind the nose) is shattered during a severe brain injury, this could damage or even cut the olfactory nerves and result in loss of sense of smell.
Luckily, the olfactory nerve is one of the few sensory organs that can regenerate new cells through a process called neurogenesis. This means that, in time, the olfactory nerve may heal. If this happens, patients can recover their sense of smell. However, olfactory nerve healing can be a prolonged process. One patient had to wait nine years to recover his sense of smell after a concussion suffered during a car crash.
If the damage is too severe, and the olfactory nerve is completely severed, or if scar tissue begins to form around it, it may be impossible for patients to recover their sense of smell.
In addition to physical damage to the olfactory system, patients may also lose their sense of smell and taste due to problems with sensory processing. In this case, the olfactory nerve is not damaged, but the brain is struggling to process the information it receives from this nerve.
In a healthy brain, neurons receive the resources they need via a network of blood vessels in the brain. As each area in the brain “requests” what it needs, the blood vessels deliver resources to the right brain cells at the right time. This dynamic relationship is called neurovascular coupling (NVC).
However, brain injuries trigger swelling and inflammation that disrupt this mechanism. As a result, affected areas can no longer get the right amount of resources — oxygen and other nutrients — at the right time for them to perform their task normally. If NVC dysfunction affects any of the brain areas involved in processing information from the olfactory or gustatory systems, patients may experience changes in smell and taste.
Dysfunction of the autonomic nervous system (ANS) may also be a cause of loss of taste and smell.
The ANS controls vital bodily functions that run in the background, such as blood pressure, breathing rates, and heart rate. Most of these processes are governed by the two main branches of the ANS: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS prepares the body for stressful or emergency situations, whereas the PNS calms everything down.
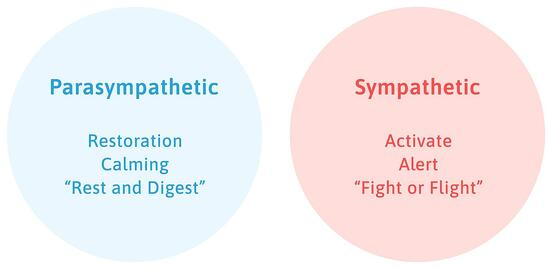
In concussion and TBI patients, this balance between PNS and SNS can be disrupted. The result is often SNS dominance, which means the SNS is overactive, while the PNS is underactive relative to normal function. This imbalance can have devastating consequences throughout the body, including in the olfactory system.
There’s very limited research in this field, but one theory suggests that being in a constant state of stress — triggered by the SNS dominance — can change the way the brain processes smells by reducing sensitivity to some odors and enhancing the recognition of specific, threat-related smells, such as burning or unpleasant odors. This may explain why some patients tell us that “everything smells like cigarettes.”
Further reading: Guide to autonomic dysfunction
Finally, loss of smell and taste can be explained by a hormonal imbalance caused by the brain injury. If the pituitary gland is affected, for example, it could cause hypothyroidism, resulting in a deficit of a hormone called thyroxine.
Thyroxine is needed to ensure smell receptors and taste receptors are fully operational and able to communicate with different parts of the brain. Insufficient thyroxine could lead to reduced or even total loss of the sense of smell and taste.
Further reading: Hormone imbalance after a head injury

Doctors commonly tell patients that if they don’t get better within 6-12 months after the injury, then their sense of smell isn’t going to come back, and there is nothing that can be done. This assessment is not always accurate. While the prognosis of recovery from olfactory loss is admittedly poor, with the right treatment, it is possible for some patients.
Studies show that smell training (also called olfactory training) can help about one-third of patients. Smell training involves smelling strong scents to retrain the olfactory system and help it heal. The most commonly used fragrances are rose (floral), lemon (fruity), cloves (spicy), and eucalyptus (resinous). It’s believed this helps because it encourages cells in the olfactory nerve to regrow and reconnect to different areas of the brain.
But smell training may only be one aspect of recovery. For patients whose smell and taste disruption stems from neurovascular coupling dysfunction or autonomic nervous system dysfunction, treatment at Cognitive FX may help.

For many PCS patients, the loss of smell and taste is not the only symptom they’re experiencing. They usually experience a wide range of cognitive, physical, and emotional issues, including but not limited to the following:
Instead of only getting treatment for individual symptoms, patients need a treatment that addresses PCS as a whole. That's the approach we take at Cognitive FX. Our multidisciplinary therapy program holistically treats interconnected, long-lasting brain injury symptoms.
Before treatment starts, patients undergo a detailed examination. Our therapists review their medical history, ask about past and current symptoms, and test physical, cognitive, and emotional health.
During this initial evaluation, patients complete a functional Neurocognitive Imaging (fNCI) scan. This scan assesses how blood flows in 56 regions of the brain and how these regions communicate with each other while the patient performs a series of cognitive activities. In practical terms, the scan shows us how much and where in the brain a concussion has affected neurovascular coupling (NVC).
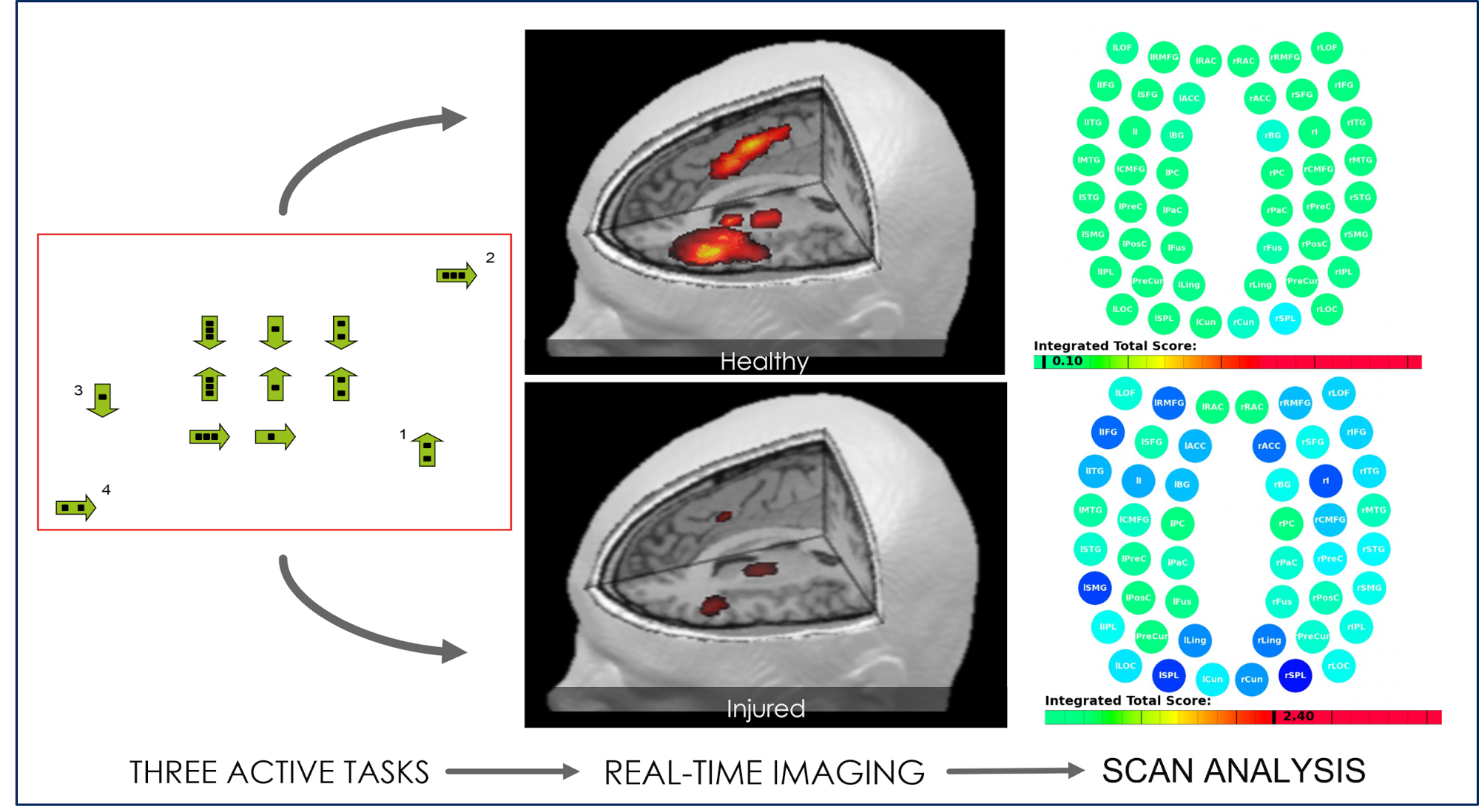
Just seeing the scan results is often an emotional moment for patients. “It was a great moment to have someone validate everything I’d been struggling with,” shared patient Sam Gray, who received treatment for a brain bleed he’d had 30 years prior.
With the results of the medical assessment and the scan, our team designs your treatment plan, which is carried out during our program: EPIC treatment, short for Enhanced Performance in Cognition.
This process involves a three-step cycle that repeats multiple times a day: Prepare, Activate, and Recover. The aim is to restore neurovascular coupling, improve ANS function, and reduce the incidence and severity of PCS symptoms.

Prepare: Patients complete short sessions of aerobic exercise followed by breathing exercises. This improves blood flow in the brain and promotes the release of neurochemicals that prepare the brain for the activities that follow. Exercise is a key component of brain injury recovery.

Activate: Aerobic sessions are followed by a series of different therapies, including occupational therapy, neuromuscular therapy, neurointegration therapy, cognitive therapy, sensorimotor therapy, vision therapy, vestibular therapy, and others. These exercises aim to help restore healthy neurovascular communication throughout the brain.
Recover: The last step involves periods of rest throughout the day to help the brain recover before the subsequent therapy. This may include neuromuscular massage of the neck and shoulders, mindfulness exercises, breathing training, and listening to Brainwaves (which benefits your brain in a way similar to meditation). Read more on the do’s and don’ts of brain rest in concussion recovery.
One patient who made a full concussion recovery, Quirien Willemsen, described treatment this way:
We don’t target loss of smell and taste specifically, but if patients feel that their sense of smell and taste is improving during their treatment with us, our therapists can suggest exercises similar to smell training to support further improvements.
To see if you are eligible for treatment, sign up for a consultation.
Improvements in sense of smell may be associated with improvements in other symptoms. For example, we had one patient who experienced improvements in both balance and sense of smell at the same time after therapy. This happens because as exercises and therapy improve blood flow within a particular area in the brain, it can affect neighboring areas as well. In the case of this patient, exercises that were designed to help with balance also helped the sense of smell because treatment improved NVC within both areas.
We often take advantage of this mechanism — called cranial nerve stacking — when working with our patients. For example, as the olfactory nerve is close to areas involved with vision, our patients perform smell tests and vision therapy simultaneously to stimulate those areas in the brain. Used this way, smell training works the same way as an exercise that stimulates blood flow in the region and prepares the brain for therapy.

At the end of treatment, patients go through a second scan to monitor how their brains are recovering. Patients also meet one last time with our team to assess progress and to receive a list of recommendations for exercises at home. Typically, the at-home regimen includes aerobic exercises, cognitive activities, and rest.
Most patients spend around an hour for five days a week on these exercises, then slowly reduce their time spent as they recover more fully. Following these recommendations is an excellent way to ensure long-term recovery. Most patients continue to improve at home in the weeks and months that follow treatment.
Further reading: How this lawyer recovered after a car accident caused persistent symptoms

Impairment of smell and taste can have a severe impact on the patient’s quality of life and may put them at risk of accidents at home. Some complications of losing your sense of smell include:
To avoid these complications, patients must learn ways to live with only half their senses. This can be challenging, so here are a few tips to help patients cope with the loss of taste and smell after a head injury:
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in therapy for persistent brain injury symptoms. To see if you are eligible for treatment, sign up for a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:

Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...

If you notice symptoms after a concussion, it’s best not to wait to seek treatment. If you’re the type to “wait it out” and see if things get better, then we recommend waiting no longer than three...
.png?height=175&name=childhood%20head%20injuries%20(11).png)
After a concussion or other type of traumatic brain injury (TBI), some patients experience persistent symptoms for months, or even years. This condition is known aspost-concussion syndrome (PCS),...
If you’re searching for answers and think you might have post-concussion syndrome (PCS), the path to diagnosis can be challenging. Few medical professionals are experts on the condition, and many...

There is no exact time frame for recovering from a mild traumatic brain injury (mTBI), otherwise known as a concussion. The majority of people who sustain an acute concussion recover within a few...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY