A Patient’s Guide to TBI Physical Therapy
Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
When people think of concussion symptoms, they often think of the obvious ones: headaches, drowsiness, fogginess. What they don’t expect are gastrointestinal issues.
In the two weeks after a concussion, you might experience changes to your sense of taste or smell, loss of appetite, nausea, or vomiting. And if your concussion develops into post-concussion syndrome, you can have a whole host of stomach problems resulting from that head injury for months or years afterward, such as:
|
|
|
|
|
|
|
|
|
Unfortunately, many family healthcare providers, sports medicine professionals, and even neurologists don’t make the connection between mild traumatic brain injury (mTBI, or concussion) and stomach troubles. Worse, some dismiss the possibility outright.
While a head injury is far from the most common cause of stomach woes, it could be the cause of your stomach problems if you developed them after that injury.
So why do concussions sometimes cause stomach problems? And what can be done about them? In this post, we answer these and other common questions we get at our post-concussion treatment clinic:
We also discuss how gastrointestinal changes can affect how you metabolize your medications, and what getting treatment for the head injury and resulting symptoms involves.
We specialize in treating lingering symptoms of a concussion and other head injuries. 95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. To learn if we can help you, book a consultation with our team.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
A concussion or other head injury can cause stomach problems. These symptoms may resolve during your initial recovery (two weeks to three months after the injury) or may persist for months or years. They might not appear until some time after the concussion. To understand why this happens, you need to know how a healthy gastrointestinal system functions. Then, it’s easier to understand what sometimes goes wrong after a mild or severe TBI.
The purpose of the gastrointestinal tract (GI tract) is two-fold:
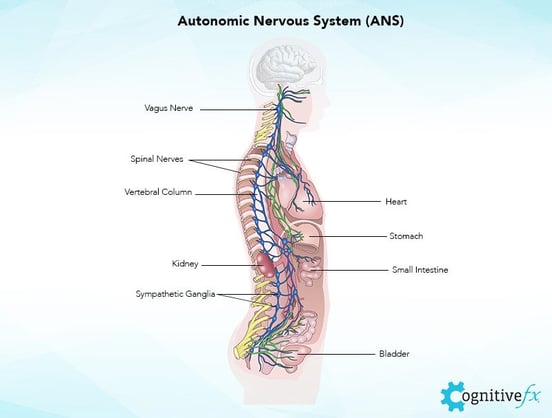
Most of what happens in your GI is controlled locally. The stomach is governed by the enteric nervous system (ENS, sometimes called your “second brain”). But it also responds to stimuli from the brain and the autonomic nervous system (ANS), especially through the vagus nerve.
The autonomic nervous system reaches into almost every organ system in your body to control, or at least influence, automatic processes — think heart rate, blood pressure, breathing, speed of digestion. It’s the invisible hand behind your “fight or flight” (SNS, the sympathetic branch of the ANS) and “rest and digest” response (PNS, the parasympathetic branch of the ANS).
This influence is critical for normal functioning. If you were happily enjoying a meal around the campfire and were suddenly attacked by a bear, your ANS would divert the blood from around your stomach to your muscles so you could flee. This would temporarily slow down digestion, which could resume at a normal pace when the threat was averted.
But the ANS also responds to signals from the gut. Your GI tract has sensory cells that detect nutrients, gut hormones, and distension (expansion of your stomach or intestines). Information from the gut goes to the ANS, and information from the ANS goes to the gut. You can’t have a healthy, functioning system without this two-way communication.
But there’s another system present in your GI tract: the immune system. Your immune system monitors everything that passes through your GI tract to the rest of the body and targets any threats for elimination. That could mean everything from sequestering bacteria in mucus to an immune cell response that kills dangerous cells.
Your sense of taste, your sense of smell, your brain’s ability to interpret signals (“This tastes good” or “I’m hungry”), and even the composition of your “good” gut bacteria also play a role in GI health.
A change in any one of those many variables can lead to stomach issues.
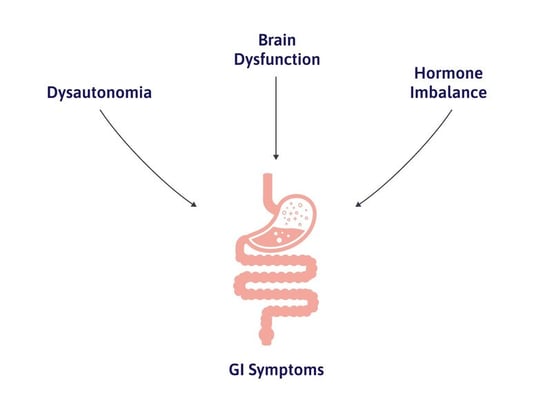
A head injury, damage to the brain stem, or an injury to the vagus nerve can spark dysfunction in the autonomic nervous system (a condition known as dysautonomia).
Dysautonomia may be severe or mild, and the exact mix of symptoms changes from patient to patient. (You can read more about the connection between head injury and dysautonomia here.)
Remember how the ANS plays a large role in gut function? When you have dysautonomia, one of the systems that can be negatively impacted is digestion. Dysautonomia can change your speed of digestion and may secondarily result in your immune system overreacting or in small intestine bacterial overgrowth (SIBO).
Besides dysautonomia, changes in the brain after injury can also cause stomach problems. After a concussion, the relationship between neurons and the blood vessels that supply them with oxygen may be disrupted (neurovascular coupling [NVC] dysfunction, which you can read more about here).
The result can be brain regions that are hypoactive (not doing their jobs) or hyperactive (doing too much, or using too many resources for what they’re doing).
Here are a few examples of how brain dysfunction can lead to stomach issues:
All this to say, there are many ways that a head injury can cause stomach problems. And there are many stomach problems it can cause.

Here is a brief discussion of the symptoms you might have from post-concussion stomach issues, along with possible causes of each specific symptom. GI dysfunction resulting from head injury can cause nausea, loss of appetite, diarrhea and constipation, vomiting, development of food sensitivities and allergies, bloating and gas, heartburn and acid reflux, vitamin deficiency, abnormal weight loss or weight gain, and mental health issues.
Nausea is one of the more complex post-concussion symptoms. It is not necessarily caused by issues with the stomach. It’s often triggered by certain situations (rather than being omnipresent) and does not have to be accompanied by vomiting.
Nausea could be caused by dysregulated breathing that results in an imbalance of oxygen and carbon dioxide in your bloodstream, blood pressure changes (especially with exercise), SIBO, digestion speed, vestibular dysfunction, and more.
You can read more about post-concussion nausea here.

There are many possible causes for loss of appetite after a concussion:
It can take some experimentation to determine the cause. If your orbitofrontal cortex is to blame, eating colorful food might help.
Food manufacturers use this trick all the time to attract buyers (think about how appetizing a red bag of chips looks, for example).
If the cause is depression, treating the depression should also help with your appetite.
If you haven’t been exercising, adding safe levels of exercise into your daily routine will help tremendously (and will often help with other symptoms, too).
A knowledgeable concussion doctor can help you discern the cause and appropriate treatment options.
Note: While loss of appetite is most common, some patients experience the reverse: gain of appetite. Some of our patients have described feeling the need to either eat more or eat more often; others have insatiable cravings for certain foods. This phenomenon could be related to the brain wanting more glucose to aid with overuse and fatigue. It could also be related to hormonal issues, like hyperthyroidism.
Dysautonomia is one of the biggest drivers of both diarrhea and constipation. You may have mostly diarrhea, mostly constipation, or wild swings between the two.
Most post head injury dysautonomia is characterized by too much sympathetic nervous system influence (remember, this is the “fight or flight” part of your ANS). As a result, patients with dysautonomia often suffer from constipation, neck pain and tension, longer recovery times after being startled, and other symptoms.
But the ANS may sometimes swing toward the parasympathetic nervous system (“rest and digest”) in an attempt to rebalance, leading to bouts of diarrhea. Diarrhea could also be a result of exercise intolerance.
You can help combat both conditions with diet and supplement choices. Magnesium will help control constipation but worsen diarrhea (note that magnesium comes in many forms — please consult with your doctor on what type is best for you). An increase in dietary fiber should help with both: soluble fiber for diarrhea (think bananas, beans, and oats) and insoluble fiber for constipation (think nuts, seeds, seeded fruit, and most whole grains).
Sufficient water intake is key, however, and several concurrent strategies will likely be needed for improvement.
Vomiting after a concussion could be an acute symptom or be situationally triggered in the months following the injury.
In the first few weeks after your head injury, vomiting could be a response to brain inflammation immediately after injury. It might also be related to migraines, if you have them.
Note: If you experience loss of consciousness, vomiting, and other signs of serious injury, seek medical attention at the nearest emergency room or medical clinic. Your doctor may order a CT scan or MRI to check for structural brain damage.
In the months following, it could be from dysfunction in the brain regions that influence vomiting, especially the medulla. It could also be from vestibular dysfunction: If your body can’t determine its position in space, the result is vertigo or dizziness, nausea, and sometimes vomiting.
Faulty signals from the vagus nerve could be the culprit, or it might be induced by exercise.
Finally, it may be from a newly developed food sensitivity or immune system overreaction, which we’ll discuss in the next section.

The connection between brain injury, dysautonomia, and development of food sensitivities is still under investigation. It’s a very new and complex field of study, so our knowledge about how and why brain injury could cause food sensitivities is still limited.
We do know that your genetic makeup and environment can influence how you respond to food after a head injury. It may be that you develop something like "leaky gut", in which foods that shouldn’t be found outside your intestines are getting out, triggering an immune response and being labeled as threats by your system. Small intestine bacterial overgrowth may also play a role in food sensitivities.
The most common allergens are the “big eight”: gluten, milk, eggs, peanuts, shellfish, soy, fish, and tree nuts. You might also develop oral allergy syndrome to raw foods that contain proteins similar to pollen allergens (for example, a ragweed allergy could result in swollen, itchy lips after you eat a melon).
These foods have proteins that look similar to proteins in other parts of the body or in common environmental allergens, so the immune system is more likely to flag them as a threat. If they are flagged, then you develop an allergy and experience an immune reaction to that food.
When your gut reacts to a food, it may be an allergy (mediated by an immune response against that food) or a food sensitivity. A food sensitivity is not an allergy but will still come with unpleasant symptoms. We don’t know why food sensitivities develop, and they may or may not go away with time.
If you’re young (not through puberty), you may grow out of your food allergy or sensitivity. But once the immune system decides a food is “dangerous,” it is unlikely to reverse the decision (barring the development of new pharmaceutical interventions in the future).
Bloating and gas could come from a bacterial overgrowth (SIBO), from the way your body reacts to certain foods, from slow GI motility, or some combination of the above. It could also be related to dysregulated breathing in which you swallow air without realizing it.
Certain yoga poses and dietary changes (especially eliminating any food you may be sensitive to) may help.
If your GI system is inflamed or moving too quickly, you might not absorb all the vitamins and minerals you need. It’s very common for our patients to have one or more vitamin deficiencies.
Ask your doctor to test your vitamin levels if they haven’t been checked recently. Even if you have normal results, it may help to take some supplemental vitamin C, vitamin B, vitamin D, and perhaps a low dose of iron.
Please consult with a physician or nutritionist before changing what supplements you take.

Many post-concussion patients are surprised to learn that dysautonomia could lead to heartburn and acid reflux, even hours after mealtime.
Some causes can be:
Two steps you can take to moderate symptoms are to use antacids like TUMS and avoid the most acidic foods (lemon, tomatoes, spicy peppers, etc.). Here’s a short article on what helps and hurts when you have acid reflux.

So often, patients tell us their doctors are laser-focused on their weight changes, blaming their symptoms on their weight. But sometimes, those weight changes are the symptom.
The ANS plays a major role in the regulation of food intake, involving fullness or hunger signals and how much energy is used or needed. Thus, ANS dysregulation might change body composition.
You know what is normal for you. Lower physical activity after your injury can contribute to weight gain, but it’s not enough for large swings in weight. If your habits don’t significantly change but you suddenly find yourself gaining or losing weight uncontrollably, that is a clear sign that something is wrong and needs medical attention.
Bacterial overgrowth (SIBO) could cause malnutrition and weight loss. Hormone changes (mainly ghrelin, leptin, thyroid hormones, and cortisol) could also be the culprits.
If you haven’t done so yet, get your hormone levels checked by a doctor who has some familiarity with post-traumatic hypopituitarism and other injury-related changes.
Here is a guide to finding and working with a doctor about possible hormone imbalance.
Your stomach and your brain have a profound influence on each other. Your brain can change your stomach function, but your stomach can also change your brain function.
For example, most of your body’s serotonin is produced in the gut. Low serotonin levels can influence your mood and might play a role in depression.
Vitamin deficiency is also associated with mental health struggles. Vitamin C deficiency, for example, is associated with mood challenges and cognitive difficulties. Vitamin B and vitamin D deficiency may also play a role in your emotional struggles.
You can learn more about emotional changes after a brain injury and their treatment options here.

The moment you put something in your mouth, it’s in your GI system. Your GI stretches from your mouth, down your esophagus into the stomach, and throughout your intestines.
That means any problem affecting your digestion could affect how you tolerate medication, too. For example, if your medicine moves very slowly through your intestines but your absorption is good, you could get a higher dose than intended during a certain time period. On the other hand, if you have a lot of gut inflammation or diarrhea, you might not absorb as much as intended.
If it moves slowly through your esophagus, the protective coating on medication could wear away before it reaches your stomach, subjecting you to a painful burning sensation.
On top of that, anything that can cross the blood-brain barrier may interact with an injured brain differently than it does in neurotypical humans.
Whether you’ve had a mild traumatic brain injury or a severe traumatic brain injury, you are more at risk for adverse reactions to medication.
Additional causes may include issues with metabolism, either from the GI or the liver, and immune-mediated hypersensitivity.
Does this mean you should never pop an ibuprofen or ignore your doctor’s recommendations? Not at all. But it does mean that you need to be attentive.
Make a note of any side effects you experience. You may need to troubleshoot dosage or try different brands of a medication until you find what’s right for you.
That said, if you have a nonpharmacological solution to a problem you’re facing, try that first.
These strategies are not a substitute for good, post-concussion treatment, but they should help with whichever GI symptoms you’re experiencing. In no particular order:

How much the treatment for your brain injury helps your stomach problems will depend on which issues you have and what’s causing them.
Treatment at our clinic can help with many other common symptoms of post-concussion syndrome, such as headaches, brain fog, difficulty sleeping, emotional changes, difficulties with attention, memory problems, vision changes, and more.
All patients at Cognitive FX receive a functional neurocognitive imaging scan (fNCI scan) before and after treatment.
This shows us exactly which of 60 brain regions are dysfunctional after your injury so we can tailor a treatment plan to your specific needs.
Treatment at Cognitive FX involves multidisciplinary, intense therapy, including neuromuscular therapy, occupational therapy, cognitive therapy, sensorimotor therapy, psychotherapy, and more.
You can read more about patient recovery journeys and what treatment is like here:
95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. If you’d like to discuss your situation and what we can do to help, book a consultation.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect...

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...

“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:


There is no exact time frame for recovering from a mild traumatic brain injury (mTBI), otherwise known as a concussion. The majority of people who sustain an acute concussion recover within a few...

Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY