Perhaps this sounds familiar: You wake up from a relaxing nap expecting to feel refreshed, but instead, your heart is pounding for no reason. Or you stand up after a few hours on the couch and feel lightheaded and unstable. Maybe your resting heart rate is now 90, even though it used to be 65.
Most people don’t know that a concussion can cause changes in heart behavior, so the symptoms catch them off guard. But it’s true: Your heart responds to stimuli from both your brain and your autonomic nervous system. After a mild traumatic brain injury (concussion) or other source of head trauma, those systems can send misleading signals to your heart.
Any head injury can affect your heart rate, including an overall increase or decrease in heart rate, lower heart rate variability (how flexibly your heart rate adapts to situational changes), palpitations or unexpected rate increases, and more.
We’ve even seen one patient whose post-concussion autonomic dysfunction led to cardiac infarction (heart attack) two weeks after injury, despite previously excellent cardiac health. His doctor couldn’t find any attributable cause except for his recent head injury.
At our clinic, we treat patients whose symptoms linger for months or years after a head injury, a condition known as post-concussion syndrome.
We also see severe TBI patients, victims of carbon monoxide poisoning, and more. Many of them are understandably concerned when their heart behaves in unexpected ways.
This post answers all their commonly asked questions. We cover:
Every week, we help head injury patients recover from persistent symptoms. 95% of our patients show statistically verified restoration of brain function by the end of one week. To discuss your specific injury, symptoms, and treatment options, schedule a consultation with our team.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
How Should Your Heart Rate Behave?

When healthy, the heart adapts rapidly to biological needs, coordinating with the brain through the autonomic nervous system (ANS), pressure receptors, and chemical receptors in the body to increase or decrease beats-per-minute (bpm). If you go for a run, your limbs need more oxygen and nutrients from your blood, so the heart beats faster to accommodate that need. When you rest, your heart rate should be slow and steady.
Your heart rate also responds to your emotions. If your coworker taps you on the shoulder and startles you, your heart rate will spike in response (as part of your fight or flight response, which is part of healthy autonomic function). But when you realize there’s no danger, your heart should settle into its resting rate quickly.
The autonomic nervous system plays a large role in these reactions. The ANS controls automatic processes in your body like blood pressure, heart rate, breathing (unless you’re actively thinking about it), digestion, and more. Two parts of the ANS are the sympathetic nervous system (SNS) and parasympathetic nervous system (PNS).
The SNS is responsible for your “fight or flight” response, while the PNS is in charge of “rest and digest.” The SNS, when activated, will pull your heart rate higher. The PNS, on the other hand, will help it decrease. Together, the ups and downs in your heart rate are part of a healthy, functioning body.
What Is Heart Rate Variability (HRV)?
Heart rate variability is how we describe the variation in time between each heartbeat. In other words, it’s the variability in how long the heart takes to do an entire cycle between one moment to the next. The shorter the cycle, the faster the pace, and vice-versa. It is strongly influenced by the autonomic nervous system. A healthy heart has high HRV because it shows adaptability to the needs of your body on the order of milliseconds. A low HRV means your heart is less flexible in its response to your body’s needs.
A concussion often causes low heart rate variability, indicating tighter control by the sympathetic nervous system. This means your heart has less flexibility to react in the moment and is connected to poorer concussion outcomes. At the same, stronger control by the sympathetic nervous system could mean that your heart rate spends more time at a higher rate.
For example, let’s say someone drops a plate and it shatters. Your heart rate spikes in response. When the SNS has a stronger influence over your heart than the PNS, it will take longer to settle back into your resting heart rate.
Low heart rate variability is often an indicator of poor health and may even shorten your lifespan. Some scientists think that every heart has a set number of beats before it gives out (just like the treads on your tire need replacing after a certain level of use). The extra wear and tear placed on your heart from low HRV and high SNS control can impact your health throughout your lifetime, which is why it’s important to seek treatment.
Can HRV Help Detect Concussion?
Some researchers are actively investigating whether HRV can be used to diagnose acute concussion. Unfortunately, it’s challenging to study. It would be ideal to have both pre-concussion and post-concussion data on patients for a rigorous investigation, but that’s often not possible. At the very least, you do need information such as…
- Control data (patient age, sex, meal times and types, time spent sitting before the measurement, existing mental health, and so forth…)
- Extensive standardization
- Long monitoring times
The many factors that play into HRV make it extremely complex and difficult to study.
One recent study showed that a soccer player had low HRV after a concussion, which resolved when the rest of his concussion symptoms did. But it took over a week for the low HRV to appear, which is too slow for immediate diagnosis. That said, it could be used in the future, with more research, by sports medicine providers as one criteria to evaluate when concussed athletes can return to play.
The Effects of Concussion on Heart Rate
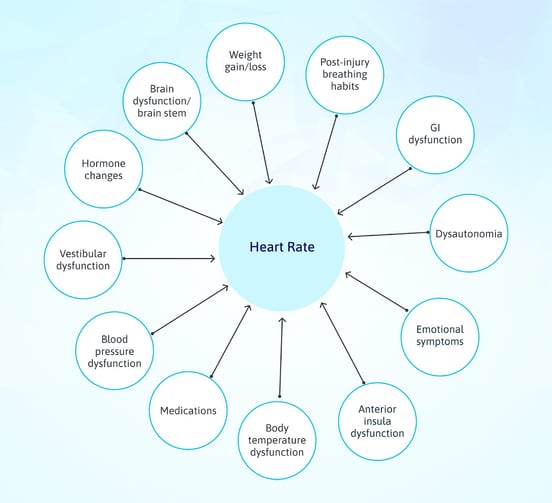
There are many reasons that your heart rate could change after a concussion. One of the biggest is dysautonomia: Dysregulation of the autonomic nervous system. In most patients, dysautonomia presents as overactivation of the sympathetic nervous system (SNS). Dysautonomia could cause your heart to receive imbalanced signals, leading to symptoms.
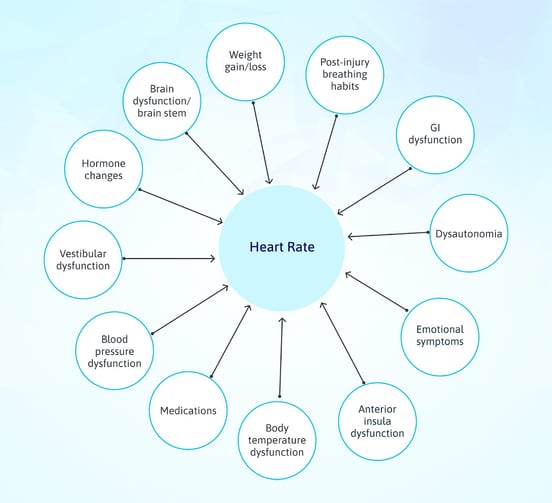
Here is a list of many other possible reasons you may have heart rate changes after a head injury:
- Brain dysfunction in the anterior insula, which interacts closely with the ANS
- Injury to the brain, brain stem, or vagus nerve, which sends signals directly to the heart (more common in whiplash injuries)
- Post-injury changes in blood pressure regulation
- Post-injury emotional changes (such as attention, impulse control, PTSD, anxiety, and anger)
- Weight gain or loss post-injury (body size and composition affects heart rate).
- Medication side effects (Adderall, thyroid medicine, any source of stimulants including the cold medicine pseudoephedrine, and some SSRIs)
- Body temperature regulation difficulties
- Vestibular dysfunction (an incorrect understanding of your position in space could lead to heart rate increasing or dropping inappropriately)
- Hormone changes (for example, hyperthyroidism could raise your heart rate, or low estrogen could lead to arrhythmias)
- Incorrect post-injury breathing dynamics
- Gastrointestinal symptoms (these can affect your healthy gut bacteria, which in turn affect cardiovascular health)
With all those possible drivers of heart rate changes and interactions between potential causes, it’s little wonder that patients have heart-related symptoms after concussion. Here are some common ones we’ve seen.
Can a Concussion Cause Heart Rate Increase or Decrease?
Yes. You may notice that your baseline, resting heart rate increases or decreases after a head injury. One common cause of a high heart rate would be overactivation of the sympathetic nervous system. Alternatively, the parasympathetic nervous system could overreact and drive your heart rate down.
A stable increase or decrease, however, is less common than situational heart rate symptoms such as heart palpitations or exercise intolerance.
Can Concussion Cause Heart Palpitations?
Yes, a concussion can lead to heart palpitations. Heart palpitations can involve sensations such as your heart beating harder, skipping a beat, and more.
The most common complaint we hear from patients is that they feel like their heart is pounding in their chest for seemingly no reason. It feels like your heart rate increased, but the “pounding” feeling is actually a sign that your heart is working harder than usual to pump blood.
Why is that? Imagine you try to squirt water out of a straw by blowing on one end. With no obstructions, the water flies out easily. But if you pinch the straw, you have to blow harder for the water to move through.
Similarly, if your blood vessels are constricted, your heart has to work harder to pump blood through them. Sometimes they constrict when they shouldn’t, due to incorrect signalling from the autonomic nervous system. The result is a pounding heart until the situation is remedied.
Can Concussion Lead to POTS?

Yes, a concussion could lead to POTS (postural orthostatic tachycardia syndrome). You might have POTS if you feel lightheaded, get heart palpitations, or faint after standing up. POTS patients’ heart rates increase when they stand (known as orthostatic tachycardia) to compensate for a blood pressure drop when they change positions.
They also experience a host of other symptoms affecting both cognition and physical well-being, such as anxiousness, brain fog, blurry vision, sleep problems, and fatigue. These symptoms overlap closely with post-concussion syndrome symptoms. If you are diagnosed with POTS after a head injury, the head injury is likely the cause (and can be treated).
What Are Other Symptoms Related to Heart Rate Changes?
Heart rate dysfunction can lead to secondary symptoms as well. Here are a few we’ve encountered in patients:
- Feeling like you have the flu after exercising. Some patients experience immediate symptoms during physical exertion (such as headaches, stomach pain, and lightheadedness). Others have delayed flu-like symptoms such as joint pain, body aches, and fatigue.
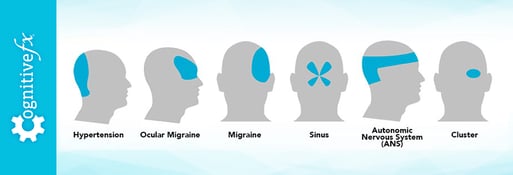
- Pounding headaches. Some patients “feel” their heart beat in their head, resulting in a persistent and painful headache.
- Lymphedema or other lymph-related problems. The lymphatic system expects a certain amount of blood flow. Heart rate changes can result in back flow, insufficient blood filtering, and other problems. Think of it like the garbage system. You have a specific size trash can that’s picked up at a regular interval. If you don’t put the garbage out on time, it gets backed up. The same applies to your lymph system (which you can think of as your body’s garbage disposal unit, among other roles).
- Cardiac infarction. Fortunately, concussion resulting in a heart attack is rare, but we have seen it happen.
- General decline in health. After a concussion, you may struggle to get enough exercise and sleep. If your symptoms persist for months, that takes a toll not only on your heart health (which relies on good sleep and exercise habits) but on your overall well-being.
What If You Have a Pre-Existing Heart Condition?
Some patients have pre-existing heart troubles before their head injury. This could result in a few scenarios:
- The concussion worsens your current health problems.
- The concussion triggers new, additional health issues that need to be managed.
- The concussion changes how you react to your heart medications, resulting in new side effects.
Some people (doctors, even) think that once you’ve tried a medicine and didn’t have any side effects, it will always be safe for you. That’s simply not true. A head injury can change the way your body interacts with that medicine.
Perhaps the injury worsens your condition, and you now need a higher dose to manage it. Or, perhaps autonomic dysfunction slows down your GI tract or changes its permeability (how well or poorly it absorbs nutrients). With food moving more slowly through your intestines, more of the drug gets absorbed than before your injury, and your body reacts to the increased dose with heart rate changes.
Another example is gaining or losing weight. A different body fat percentage could change how your body responds to a certain medication dose.
If you think any of your symptoms could be side effects of a medication you started taking before or after your injury, talk to your doctor about next steps.
Treatment for Persistent Post-Concussion Symptom

If your symptoms arose after a brain trauma of any kind, then it’s important to treat the root cause of symptoms: brain dysfunction and dysautonomia.
At CognitiveFX, every patient gets a functional neurocognitive imaging (fNCI) scan, which looks at cerebral blood flow biomarkers in over 60 brain regions. This shows us which areas likely suffered impairment of healthy brain function. We use this information, in addition to physical evaluation and a symptoms questionnaire, to target treatment to the unique needs of each patient.
Every patient receives neuromuscular therapy, cognitive therapy, occupational therapy, sensorimotor therapy, vestibular rehabilitation, and more. You can read more about why this helps post-concussion patients here.
Some of the specific techniques we use to help patients with heart rate symptoms and dysautonomia include:
- Physical therapy and physical activities designed to help your ANS function better.
- Breathing exercises.
- Meditation/mindfulness training.
- Two or more sessions with a psychologist (which will help if your heart rate fluctuations are related to post-injury emotional changes).
- Therapies that target neurovascular coupling in brain areas such as the anterior insula (which is activated whenever you exercise impulse control) that modulate ANS function.
- Brainwaves (auditory pattern to help you destimulate between therapy sessions). Research has shown that Brainwaves and similar frequency techniques increase the activation of the parasympathetic nervous system.
- Exercises for the vagus nerve, which directly connects to the heart.
You can expect to make rapid progress with brain dysfunction during treatment. Each patient gets a post-treatment fNCI scan to confirm the progress they’ve made. Dysautonomia-related symptoms may be slower to resolve and could take some upkeep at home to keep you feeling well. Each patient is unique, so post-concussion recovery looks a little different for each person.
What Can You Do Now?
If you have persistent symptoms after your head injury, including heart rate changes, it’s important to get treatment. You can consult our team after filling out some paperwork, so that we understand your medical history.
In the meantime, do your best to eat foods that will support your brain and nervous system, get exercise even if it’s difficult, and sleep as well as you can. If any of your heart-related symptoms are worrisome to you, see your doctor about short-term solutions until you’re able to get treatment for your injury.