Headache pain is the most common symptom after a traumatic brain injury, with up to 90% of patients experiencing this symptom for at least a few days after suffering a concussion. These headaches can also develop after other causes of head trauma, such as bacterial and viral brain infections, carbon monoxide poisoning, “chemo” brain, transient ischemic attack, and COVID-19.
The vast majority of people with post-traumatic headaches (PTH) experience symptom improvement within weeks; however, for some patients, headaches may persist for months or years. Alongside headaches, these patients may also experience a wide range of other persistent symptoms, such as brain fog, mood swings or "personality changes", memory problems, and difficulty concentrating. This condition is called post-concussion syndrome (PCS).
For PCS patients, the most common types of chronic post-traumatic headaches include tension-type headaches and migraines. If you’re experiencing these types of headaches and your doctor prescribed analgesics to control the pain, you may have found that your headaches didn’t respond well to medication. We’ve written in detail about why medication is often not a good solution for PCS patients. It has to do with a combination of factors, such as head trauma patients being more at risk for side effects and medications not being designed with the pathophysiology of PTH in mind.
For example, while patients with PTH often use painkillers and/or antidepressants for their symptoms, SSRIs (a class of antidepressants) may increase or cause headaches, and pain medicine can cause rebound headaches. Treating post-traumatic headaches is complicated and may require a multidisciplinary approach. Because of that, going to just one doctor (such as a neurology practitioner) may not be enough to resolve your symptoms.
In contrast, at Cognitive FX, we offer an alternative treatment that doesn’t rely on medication. We use a combination of exercise and multidisciplinary therapies to address the root cause of post-traumatic headaches. Therapy improves headaches while also addressing many other common, persistent symptoms of head trauma.
In this article, we’ll look at:
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.
What Is a Post-traumatic Headache?
One of the most debilitating symptoms you can experience after a concussion or other head injury is a headache. These headaches are known as post-traumatic headaches (PTH). Curiously, post-traumatic headaches are more common after mild traumatic brain injuries (mTBI) than moderate or severe TBIs.
The International Headache Society defines this type of headache as a headache caused by trauma to the head that develops within seven days after the incident or after regaining consciousness. However, doctors have challenged this part of the international classification of headache disorders because some patients only start experiencing headaches caused by a concussion several months, or even years, after the neurotrauma.
Although the official definition includes headaches after a traumatic incident, we have found that patients with other conditions that may affect the brain, such as CO poisoning, viral infections, and COVID-19, also suffer from the same type of headaches.
Patients may experience acute or persistent headaches. Acute headaches typically resolve within three months after the incident, whereas persistent headaches last more than three months. For many PCS patients, their acute headache turns into a more persistent or chronic symptom; in fact, more than half of all patients with headaches immediately after a concussion are still experiencing this symptom 12 months after the trauma.
Potential risk factors for developing persistent headaches after a concussion include:
- Being female
- Being elderly
- Having a family history of headaches
- Having pre-existing headaches, migraines, or migraine-like headaches
- Developing a headache immediately after a concussion
- Experiencing chronic pain other than headaches
For example, if you already experience migraine headaches before a concussion, you’re twice as likely to develop post-traumatic headaches than a patient who doesn’t have a history of headaches. Patients with pre-existing tension-type headaches may also experience an increase in attack frequency. In contrast, the severity of headaches at the time of a head injury and the subsequent recovery time do not seem to increase the risk for developing persistent headaches.
When Should You Worry about Post-traumatic Headaches?
For most patients, headaches after a mild traumatic brain injury (mild TBI) are not life-threatening and leave no sequelae (i.e., development of additional medical issues due to the headaches). Nevertheless, there are situations where you should look for medical advice, including if:
- The headache gets significantly and persistently worse than usual
- You also experience nausea and vomiting (repeated incidents)
- Your arms are numb
- You struggle to speak
- You feel severe drowsiness
- You develop symptoms that you never experienced before (especially if they’re severe)
Types of Post-Traumatic Headaches
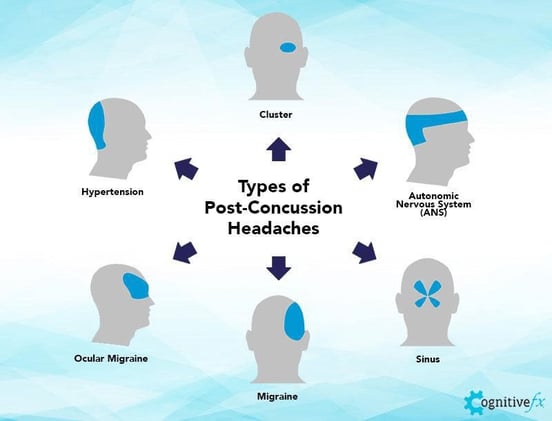
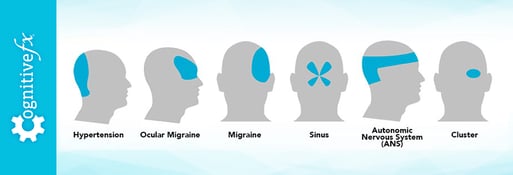
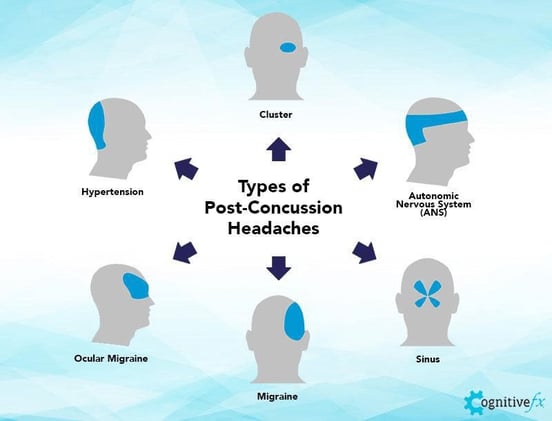
Concussions can trigger post-traumatic headaches in different regions of the head. The most frequent subtype is pain in the temple, followed by the forehead, neck, back of the head, and eyes.
Not all post-traumatic headaches are the same. There are many different mechanisms potentially involved and you may find that your headache description fits more than one type. It may be useful to keep a diary of your headaches: take notes regarding the location, cause, sensation, remedies, pain rating, and length of your headaches. Writing down how you feel and what helps to alleviate your headaches will not only help you understand how to better address your symptoms but may also help your doctor pinpoint what’s causing your persistent PTH.
In this section, we’ll describe PTH that presents as tension-type headaches, migraines, cervicogenic headaches, and medication overuse headaches.
Post-Traumatic Headaches Similar to Tension-Type Headache
Post-traumatic headaches resembling chronic tension-type headaches is one of the most common types present in patients with a brain injury (both immediately after a concussion or in PCS patients). Studies estimate that between 20% to 40% of patients experience this headache type during the first year after a concussion.
As the name suggests, these headaches are associated with muscle tension or muscle spasms. They usually have some of the following features:
- Tight, squeezing or pressing sensation around the entire head
- Pain level rated as mild to moderate.
- Occur later in the day
- Concurrent with neck pain (especially if patients suffered whiplash)
- May last a few minutes or a few hours
- Gradual increase in intensity
- Often aggravated by stress
- Concurrent sensitivity to light
Post-Traumatic Headaches Similar to Migraines
Migraines are the other common type of post-traumatic headaches, affecting almost half of all patients. This kind of headache occurs because some areas in the brain become hypersensitive and can trigger a pain signal that quickly spreads to other parts of the brain.
Patients with this type of headache often experience:
- A dull and throbbing sensation, usually on one side of the head.
- Moderate to severe intensity
- Sensitivity to light, sound, and smell
- Nausea and vomiting
- Dizziness
- Worsening pain with physical activity
- An aura (a warning signal that the migraine is coming on, such as seeing spots or bright lights, smelling a strange smell without cause, or feeling tingling in the hands).
Post-Traumatic Headaches Similar to Cervicogenic Headaches
This type of headache occurs if you've suffered an injury to the muscles and soft tissues in the neck and the back of the head. Headaches that develop more than three months after the concussion are more likely to have a cervical cause.
This type of persistent post-traumatic headache often…
- Starts where the occipital bone meets the neck, shoulders, and back of the head but can travel over the top of the head
- Worsens with head and neck movement
- Causes dizziness and balance problems (but not nausea)
- Ranges from mild to severe
- Causes a non-throbbing type of pain (sometimes described like a something is pulling around the neck)
- Causes a reduced range of motion in the neck
Post-Traumatic Headaches from Medication
It’s not uncommon for patients with post-traumatic headaches to resort to painkillers to deal with their headaches. The problem is that excessive use (or even just continued use at reasonable doses) of these medications can actually cause headaches, which are called rebound headaches. A study found that about 40% of patients may experience headaches caused by analgesic overuse. Luckily, most patients improve after they’ve weaned off those medications. The downside, of course, is that some medications — such as opioids — are difficult to stop taking and may cause side effects if stopped too quickly.
These headaches often resemble the underlying type of headache that the patient is already experiencing, which means it can be virtually impossible to distinguish between the headache caused by the concussion and the headache caused by medication. If you feel that you may be experiencing rebound headaches, contact your healthcare provider.
What Causes Post-Traumatic Headaches
Despite the high prevalence of post-traumatic headaches, the mechanism behind these headaches is still under research. Not all cases of post-traumatic headaches are caused by the same process. The most common causes include:
- Dysfunction of the autonomic nervous system
- Neurovascular coupling dysfunction
- Vision problems
- Vestibular problems
- Sleep disturbances
Let’s explore each.
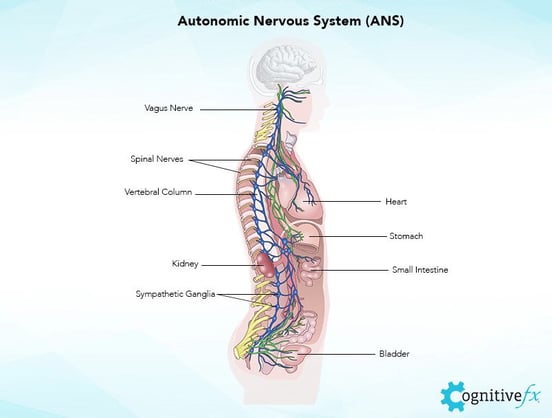
Autonomic Nervous System Dysfunction
Headaches caused by disruption of the autonomic nervous system (ANS) are some of the most distinct headaches after a head injury.
The ANS controls breathing rates, heart rate, blood pressure, and many other body functions that keep us alive. There are two parts of the ANS involved in PTH: the sympathetic nervous system (SNS), which regulates the “fight or flight” response, and the parasympathetic nervous system (PNS), which controls the “rest and digest” process. In a healthy body, these two sections work in harmony, allowing the body to respond quickly to what happens in your environment.
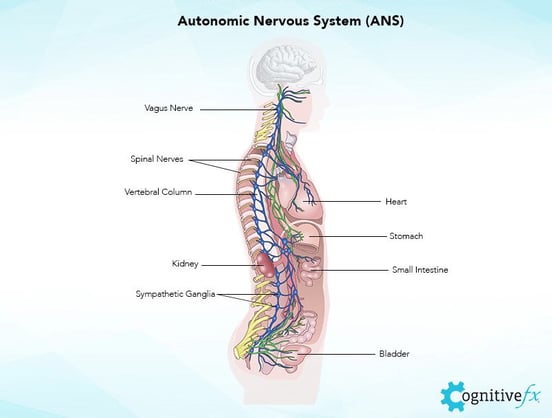
After a concussion, this equilibrium is disrupted; for most patients, the SNS tries to stay in control all the time. That means your body is constantly in a heightened, tense state, which can be very stressful for your brain. This leads to a variety of symptoms, including fatigue, sleep disturbances, memory problems, and headaches.
These headaches may present in different ways. Some patients describe these headaches as feeling like their head is blowing up like a balloon or like there’s a clamp tightening around their head. Others complain that the headaches start in the neck and move up around the back of the head to the temples. This pain is thought to be related to ANS dysfunction causing issues with cortical blood flow regulation and cortical blood pressure.
Autonomic dysfunction may also cause tension-type headaches. In this case, the pain often starts on the jaw and then moves across the face and over the top of the head. ANS headaches may also feel like pressure on the sinus area, with pain around the cheekbones (where the sinuses are located) and then spreading to the rest of the head.
Note: Post-concussion ANS dysfunction can exacerbate post-traumatic stress disorder and injury-related anxiety.
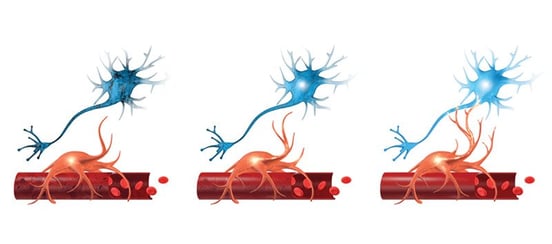
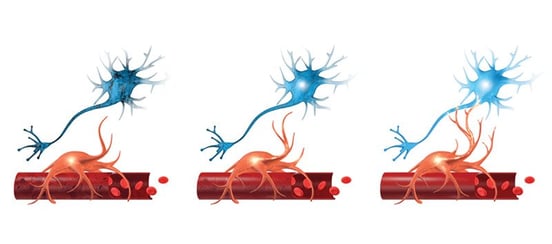
Neurovascular Coupling Dysfunction
Headaches can be the result of a breakdown in the mechanism that ensures that nerve cells in the brain receive the amount of oxygen and nutrients they need to function normally. If the dynamic between certain clusters of neurons and the blood vessels around them (called neurovascular coupling, or NVC) is disrupted, the brain struggles to perform its regular functions, which may trigger a headache.
The more the brain is affected by NVC dysfunction, the more likely it is for patients to experience headaches. If you notice that your headaches get worse when you’re doing cognitive tasks, you might be experiencing headaches caused by NVC dysfunction.
It’s not unusual for the effects of NVC dysfunction to combine with ANS dysfunction, causing symptoms of both.
Vision Problems
It’s common for head trauma to cause vision problems, which in turn may trigger headaches. Many patients report that symptoms tend to get worse in visually-busy environments, while using the computer, or when trying to read. Vision problems can be connected to NVC issues. NVC dysfunction in cortical areas involved in vision, which are in the occipital lobe, can contribute to visual headaches.
Pain from vision-related headaches tends to concentrate behind the eyes and the forehead.
Further reading: Vision problems after a concussion
Vestibular Dysfunction
Vestibular dysfunction may also lead to headaches. Located in your inner ears, your vestibular system sends messages to the brain regarding how your body is moving. Your brain combines information from your inner ears, eyes, and body to understand the position of your head relative to the rest of the body: whether you’re moving or at rest, whether your environment is moving, and so forth. Any breakdown in communication during this process could result in post-concussion dizziness, nausea, balance issues, and headaches.
Headaches caused by vestibular problems can cause the following symptoms:
- Migraines
- Severe, throbbing headaches
- Pain usually on one side of the head
- Nausea and vomiting
- Dizziness and loss of balance
- Sensitivity to light, smell and noise
Further reading: Vestibular therapy after a concussion
Poor Sleep and Other Sleep Disturbances
Poor sleep quality is one the most common complaints after a brain injury. Curiously, this symptom seems to be more frequent among mTBI patients than those with moderate or severe TBIs.
Patients may get stuck in a vicious cycle: post-traumatic headaches cause disrupted sleep, which in turn causes more headaches. At this stage, the mechanism by which sleep abnormalities aggravate headaches remains unclear.
If you’re struggling to sleep, your brain isn't getting the rest it needs to heal. We’ll discuss more later, but one of the goals of our treatment is to rehabilitate the areas in the brain that were affected by the concussion, including the thalamus, which is involved in regulating sleep. If your headaches are caused by poor sleep, our treatment program can help.
Further reading: How to address post-concussion sleep problems
Treatment for Post-Traumatic Headaches

Treating post-traumatic headaches can be challenging. As described in this article, patients can experience different types of headaches caused by different mechanisms. A one-size-fits-all approach cannot help every patient.
Treating PTH with Medication
Post-traumatic headaches can sometimes be helped with over-the-counter medications, but only as a short-term option. Immediately after a concussion, it’s safe to take Tylenol (acetaminophen) if you need pain relief. Forty-eight hours after the concussion, you can start taking non-steroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen and Aleve (naproxen sodium).
When it comes to long-term options, it’s a different story. At the moment, there are no pharmacological treatments approved by the Food and Drug Administration (FDA) to treat chronic post-traumatic headaches.
In addition, there are a limited number of studies and clinical trials looking at the efficacy of different medications to treat this type of headache. One study found that, although most participants reported short-term improvements after taking painkillers, about one-third started experiencing headaches again on follow-up. Despite these findings, many doctors turn to conventional approaches to treat patients with primary headaches, which often results in poor treatment responses.
This result makes sense when you consider that most pain medications were designed for other precipitating factors. For example, some patients with PTH are given triptans, a class of drugs that attempt to prevent or stop migraine attacks and cluster headaches. These do so partially by constricting blood flow in the brain; but if your headaches are caused by NVC or ANS dysfunction, constricting blood flow could make the problem worse!
Further reading: What a neurologist can do for post-concussion syndrome
Treating PTH without Medication
There are several non-pharmacological interventions that can be used to treat post-traumatic headaches. For example, physical therapy and massage can reduce the intensity of headaches. In addition, techniques used in cognitive behavioral therapy can be used to teach patients to deal with triggers. This involves gradual exposure, progressively increasing intensity or frequency of situations that cause headaches, allowing your brain to get used to them without triggering symptoms.
Treating Post-Traumatic Headaches at Cognitive FX

At Cognitive FX, we use a multidisciplinary therapy approach that is much more effective than a single therapy would be. Furthermore, we go beyond just trying to improve headache symptoms. Instead, we seek to help the brain heal from the injury causing your symptoms.
Our treatment process begins with a detailed examination. Our team will go through your medical history, review the symptoms that you’re experiencing, and conduct a series of physical exams that help us understand how your brain and body were affected by the concussion. Most importantly, we use an imaging technique called functional neurocognitive imaging (fNCI) to zero in on which of your brain regions were affected by your injury and how well they’re communicating with other brain regions.

The next step is to combine all this information and design a treatment plan tailor-made for you. Ultimately, our treatment aims to restore normal neurovascular coupling and ANS function in the areas highlighted as dysfunctional by our evaluation. We also use specific methods that can help relieve your head pain, including breathing exercises, neuromuscular massage, and BrainWave.

During treatment, patients go through an intense regime of exercise and therapy. Sessions start with aerobic exercise to improve blood flow in the brain, followed by different therapies to help your brain heal. Therapies used include:

At the end of treatment, patients undergo a second scan to see how the brain is adapting to therapy. For some patients, the changes are significant, while for others, the brain takes longer to respond and change. Nevertheless, 90% of our patients experience improvements in their symptoms during treatment. Most of these patients go on to continue improving at home.
After treatment, our team also meets up with you to review your scan and other test results and give you “homework.” Your homework will include some combination of aerobic exercise, cognitive games, and cognitive rest to continue your recovery journey.
You may find it helpful to read the recovery stories some of our other patients have shared. Here are a few links to get you started:
- Quieren is a Cognitive FX patient from the Netherlands who suffered from PCS after a bike accident.
- Sam Gray sought treatment 33 years after a brain bleed.
- Myrthe van Boon is a mother of two who struggled with debilitating post-concussion symptoms for years before finding Cognitive FX.
- Olivia Seitz is a former figure skater who found symptom relief after more than a decade of chronic illness.
- Sam Pembleton was an adolescent hit by a soccer ball in the head; she tried treatment methods for five years before finding Cognitive FX.
- These patients all completed video testimonials about their initial injury and their experience at Cognitive FX.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.
How to Deal with Post-Traumatic Headaches at Home

Here are some techniques you can use to cope with post-traumatic headaches at home when they arise:
- Follow a consistent sleep pattern: As described earlier, sleep problems may worsen headache symptoms and cause cognitive issues, such as poor memory and difficulty concentrating. To avoid this, go to bed and get up at the same time every day, even weekends and holidays. If you need to take a nap during the day, restrict it to 20 - 30 minutes.
- Find ways to reduce stress in your life: Find what causes you stress and do what you can to minimize it. For example, if you struggle with busy and noisy places, go shopping at off-peak hours.
- Stay in touch with your friends: It may be tempting to stay at home alone to avoid triggers, but being isolated is not the solution. Find ways to stay in touch with family and friends, get involved in your community, or look for a support group for patients with chronic pain.
- Avoid stimulants such as alcohol and caffeine: These may bring you some temporary relief, but in the long term, they may aggravate your condition and delay your recovery.
- Practice mindfulness and breathing exercises: Learn mindfulness or breathing techniques to relax at home. This helps to dampen the sympathetic nervous system and improve blood flow, as well as many other benefits.
- Exercise regularly: It may make your headache worse at first, but regular exercise can alleviate your headaches and improve cardiovascular health. If you’re struggling, try exercising in short bursts of intervals interspersed with controlled breathing. If you struggle to find 30 minutes, start with 10 minutes and work your way up.
- Eat a balanced diet: It’s important to stay healthy overall to help your brain heal. Eat food that can help the brain recover from injury, take supplements and vitamins as needed, and avoid processed, fatty, or sugary foods.
- Consult your physician: If you haven’t yet, consult with your doctor to confirm there is no structural damage in your neck. If structural damage goes untreated, it could cause headache and other symptoms indefinitely.
- Try our headache relief masterclass: We put together a class specifically to help with post-traumatic headache pain relief.
- Try massage therapy: Tension in the neck and shoulders can contribute to headache pain. You can work with a massage or physical therapist to receive therapeutic massage and stretching exercises to help.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.