If you're reading this, you've probably tried everything for the headaches that won't quit since your COVID infection. Maybe it's been three months. Maybe it's been two years. You've likely cycled through Tylenol, ibuprofen, and perhaps even prescription medications that your doctor assured you would help.
And yet here you are, still searching for answers.
You're not imagining things, and you're certainly not alone. Research published in 2025 shows that 16.2% of people who never had headache problems before COVID develop persistent headaches that last well beyond their initial infection. For those who already dealt with headaches before getting sick, the numbers are even higher.
The frustrating truth? Most conventional treatments focus on masking the pain rather than addressing what's actually causing it. But recent scientific discoveries are changing how we understand and treat long COVID headaches, and the results are encouraging.
In this article, you'll learn:
Are persistent symptoms affecting your quality of life? Our team at Cognitive FX has helped thousands of patients recover from brain injuries, including those caused by viral infections like COVID-19. After just one week of treatment, patients report a 60% average improvement in symptoms. Schedule a free consultation to discuss whether our approach could help you.
Characteristics of Long COVID Headaches
Headaches are one of the most common symptoms of COVID-19. In most cases, the headaches begin within the first few days after symptom onset and may even be the first sign of infection that patients notice (instead of the typical loss of smell and loss of taste).Curiously, patients with a headache during the first few days of illness had a lower risk of mortality. The incidence of headache as a symptom of COVID-19 has yet to be determined; reports share values anywhere from 10 to 70%.
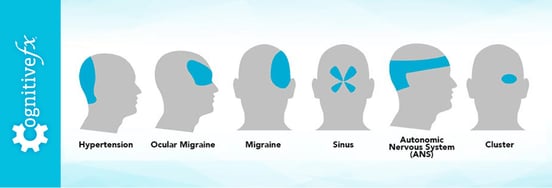
Some COVID patients describe their headaches as moderate to severe pressure at the front of the head. Others say it spreads throughout the skull or that it feels like a pulsating pain on both sides of the head. About one in four patients who develop a headache experience migraine-like headaches after their COVID-19 diagnosis.
Most patients recover within a few weeks, but some develop long-term headaches. A study found that about 20% of patients who presented with headaches during the acute phase of COVID-19 still had chronic, daily headaches after three months, but this value had dropped to 16% after nine months. The authors noticed that the greater the intensity of the headache during the first few days, the greater the chances that it would persist for longer.
What Causes Long COVID Headaches
Long COVID headaches aren't like ordinary headaches. Patients describe them in ways that often puzzle their doctors:
Pressure and tightness. Many people feel like a band is wrapped around their head, squeezing from all sides. Others describe it as their skull being slowly inflated from the inside.
Location varies. Some experience pain concentrated at the front of the head. Others feel it spreading across the entire skull or pulsating on both sides. About one in four patients develop migraine-like symptoms complete with light sensitivity, nausea, and visual disturbances.
Unpredictable patterns. Your headache might be constant, or it might come and go without any obvious trigger. Some patients wake up feeling fine only to develop crushing head pain by afternoon. Others wake up with headaches that gradually improve throughout the day.
A 2025 population study following 448 COVID patients for two years found that among those who developed new headaches after infection, nearly 65% experienced migraine-like symptoms. What surprised researchers was that over half of these new migraine cases occurred in people over age 50, well past the typical age when migraines first appear.
How Long Do Post-COVID Headaches Last?
Here's what the research tells us about timing:
The first two months are critical. Headache rates drop rapidly during this window, from nearly half of all COVID patients at onset down to about 10-16% by day 60.
After two months, things stabilize. If you still have significant headaches at the two-month mark, they're unlikely to resolve on their own without treatment. A Spanish multicenter study found that patients with headaches persisting at two months showed almost no spontaneous improvement by nine months.
Long-term outlook with treatment. Among patients who develop chronic daily headaches, about 72% still experience symptoms at long-term follow-up. However, most report gradual improvement in intensity over time, especially with appropriate treatment.
The takeaway? Don't wait and hope your headaches will simply disappear. Early intervention matters.
What Causes Long COVID Headaches
This is where things get interesting. Unlike a simple tension headache from stress or a migraine triggered by certain foods, long COVID headaches can stem from multiple overlapping causes. Understanding your specific triggers is essential for finding relief.
1. Neuroinflammation and Microglial Activation
Your brain has its own immune system, and COVID can throw it into overdrive.
A groundbreaking 2024 study from the University of Greifswald identified specific inflammatory markers that predict headache severity in long COVID patients. People with new or worsened headaches showed significantly elevated levels of a protein called CX3CL1 (also known as fractalkine), which indicates that the brain's immune cells, called microglia, are chronically activated.
Other inflammatory markers linked to post-COVID headaches include VEGF, TGF-β1, and β-NGF. The higher these markers, the more frequent and severe the headaches tend to be.
This isn't just academic. It explains why anti-inflammatory approaches sometimes help and points toward potential diagnostic tests that could identify which patients need more aggressive treatment.
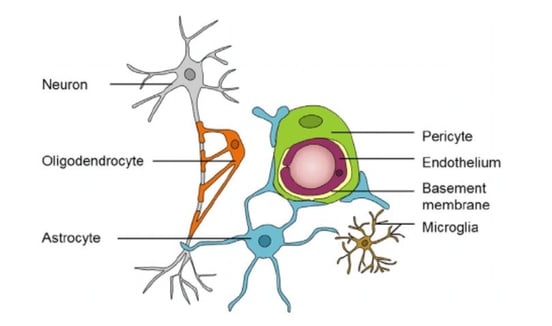
2. Neurovascular Coupling Dysfunction
Here's a concept that's central to understanding long COVID symptoms: neurovascular coupling.
Your brain cells need a constant supply of oxygen and nutrients delivered through blood vessels. In a healthy brain, there's a dynamic communication system where neurons signal for exactly the right amount of blood flow at exactly the right time. This relationship is called neurovascular coupling (NVC).
COVID-19 damages the lining of blood vessels throughout the body, including in the brain. When this happens, the communication between neurons and blood vessels breaks down. Brain regions can't get the resources they need when they need them.
Research published in Brain Communications in 2024 confirmed this mechanism using specialized imaging. COVID patients showed significantly decreased neurovascular coupling in key brain regions alongside impaired blood vessel function. This dysfunction doesn't just cause headaches. It also explains brain fog, difficulty concentrating, and memory problems that often accompany long COVID.
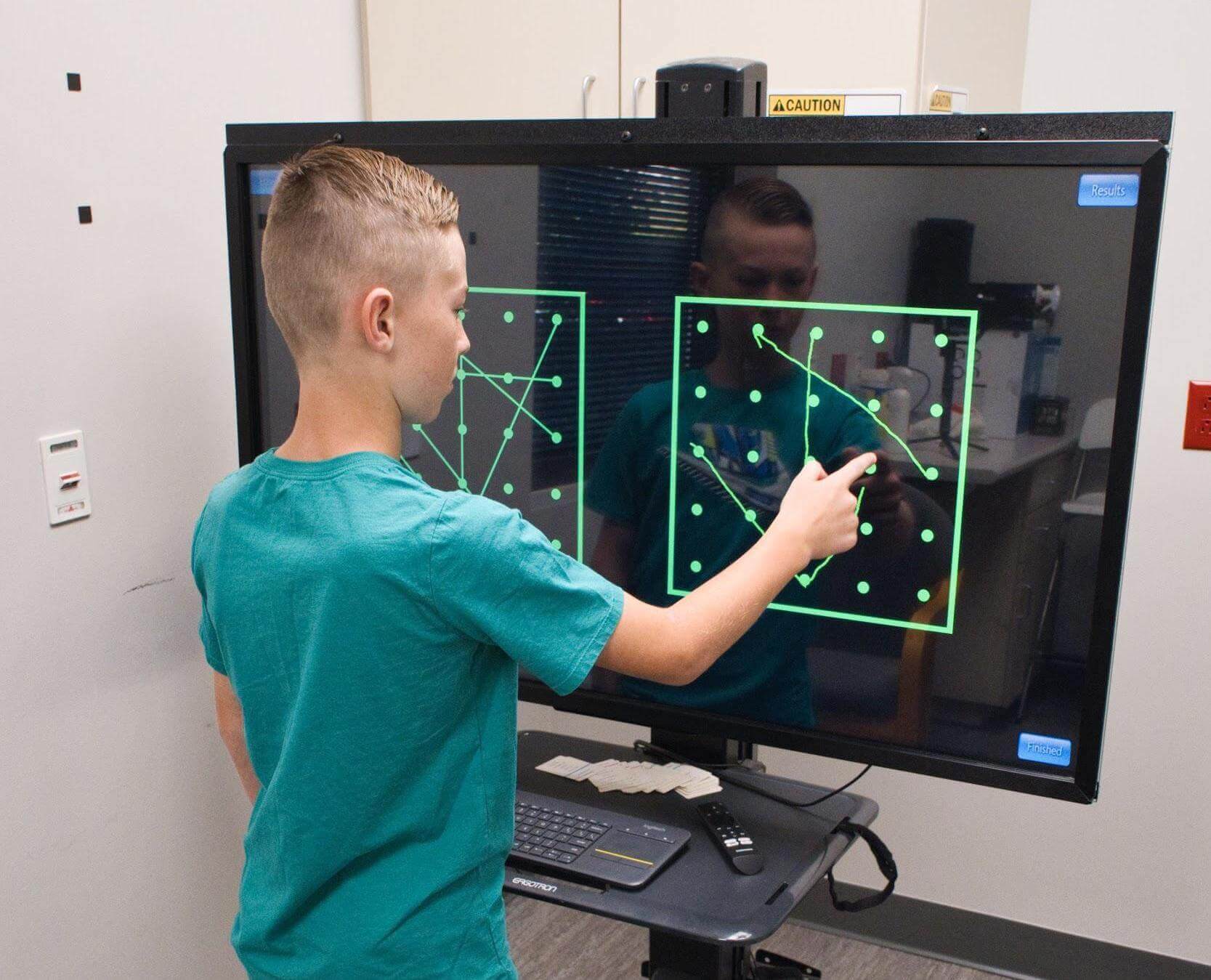
At Cognitive FX, neurovascular coupling dysfunction is one of the primary issues we identify and treat. Our functional NeuroCognitive Imaging (fNCI) technology allows us to see exactly which brain regions are affected and tailor treatment accordingly.
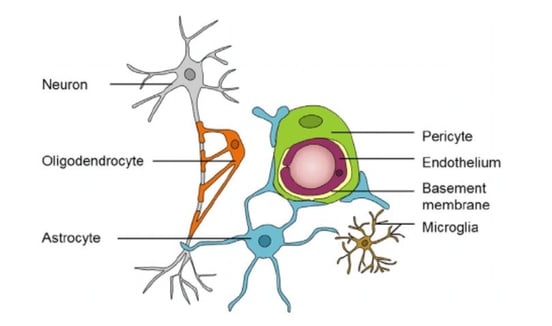
Image source: Nelson et al (2016).
3. Autonomic Nervous System Dysfunction
Your autonomic nervous system controls functions you don't consciously think about: heart rate, blood pressure, breathing, digestion. COVID frequently disrupts this system, leading to a condition called dysautonomia.
The numbers are striking. The LISTEN Study published in 2025 found that 30% of long COVID patients meet criteria for POTS (postural orthostatic tachycardia syndrome), where heart rate spikes abnormally when standing. And here's the connection to headaches: migraine occurs in over 40% of POTS patients, making it the most common associated condition.
Autonomic headaches often have distinctive features:
- Orthostatic headaches that worsen when you stand up and improve when you lie down
- Crown-shaped pain starting at the back of the neck and spreading up and around the head
- Sinus-like pressure around the nose and cheekbones that doesn't respond to allergy treatment
- Exercise intolerance where physical activity triggers or worsens head pain
- Accompanying symptoms like heart palpitations, lightheadedness, or temperature regulation problems
If your headaches fit this pattern, treating the underlying autonomic dysfunction often resolves the head pain as well.
4. Breathing Pattern Disorders
COVID attacks the lungs, and even after the acute infection clears, many people are left with subtly dysfunctional breathing patterns.
Think about it: we breathe roughly 25,000 times per day. It only takes about four days of altered breathing during acute illness to establish new motor patterns that persist long after recovery.
The most common pattern is chronic low-grade hyperventilation. You take shallow, rapid breaths that leave stale air in the lower lungs. This disrupts the balance between oxygen and carbon dioxide. Carbon dioxide is actually essential for oxygen to be used by your cells, so excess oxygen ends up unused while your brain struggles with inadequate resources.
These breathing patterns trigger headaches through multiple mechanisms: reduced oxygen delivery to the brain, activation of the sympathetic "fight or flight" nervous system, and perpetuation of autonomic dysfunction.
The tricky part? Many people hyperventilate without feeling short of breath. You might have no idea your breathing is contributing to your headaches until a trained professional evaluates your breathing mechanics.
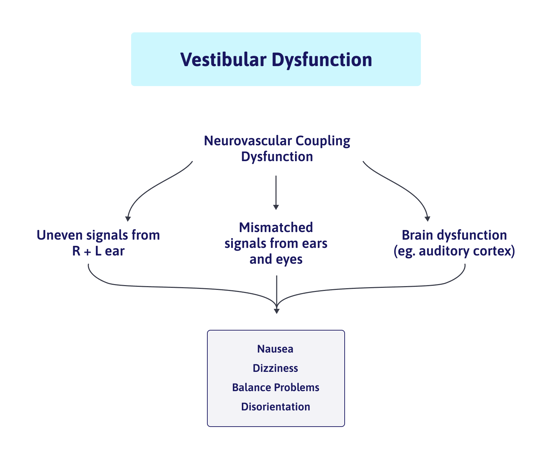
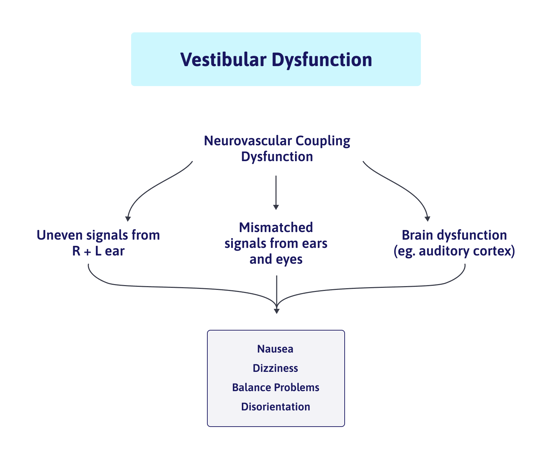
5. Vestibular Problems
Your vestibular system, located in your inner ear, helps you maintain balance and spatial orientation. COVID can damage this system, leading to dizziness, vertigo, and yes, headaches.
Vestibular headaches often:
- Appear when you wake up in the morning
- Come with dizziness, nausea, or motion sensitivity
- Worsen with head movements
- Include a sensation that the room is spinning or tilting
Some long COVID patients are being diagnosed with "vestibular migraine" after their infection despite having no prior history or risk factors. The virus appears capable of directly affecting the vestibular apparatus.
6. Vision Dysfunction
About one in ten COVID patients experience eye problems during their infection, including dryness, light sensitivity, and pain behind the eyes.
Vision-related headaches typically:
- Feel better in the morning after your eyes have rested overnight
- Progressively worsen throughout the day as eye fatigue builds
- Concentrate around or behind the eyes
- Accompany difficulty with screen use or reading
7. Pre-Existing Migraine Tendency
If you had migraines before COVID, you're nearly three times more likely to experience headaches during and after infection. But there's a twist: many patients report that their post-COVID headaches feel different from their previous migraines.
COVID may also unmask migraine tendencies in people who were predisposed but had never experienced significant headaches before. The virus acts as a trigger, pushing a vulnerable system over the threshold.
8. Medication Overuse
Here's an irony that catches many patients: the medications you're taking to control headaches may actually be causing them.
When you use pain relievers frequently, your brain adapts by becoming more sensitive to pain. This creates rebound headaches that drive you to take more medication, perpetuating the cycle. One Brazilian study found that 45% of long COVID patients with chronic daily headaches showed patterns of excessive analgesic use.
Common culprits include:
- Over-the-counter pain relievers (Tylenol, Advil, Aleve)
- Triptans prescribed for migraines
- Combination analgesics
- Opioid medications
If you're taking pain medication more than two or three days per week, medication overuse could be contributing to your problem.
9. Lifestyle Disruptions
Long COVID often forces major changes to daily routines. You might be sleeping more (or less), exercising differently, working from home, or struggling to maintain your usual activities. These shifts can contribute to headaches independent of any direct effect from the virus.
Common factors include:
- Dehydration from reduced activity or altered thirst signals
- Poor sleep quality even when total sleep time is adequate
- Reduced physical activity that decreases blood flow and cardiovascular fitness
- Increased screen time that strains the visual system
- Social isolation and its effects on mental health
10. Caffeine, Alcohol, and Medication Changes
Changes to caffeine intake, either increasing or decreasing, can trigger headaches. Alcohol affects some long COVID patients differently than before their infection. And if you've started or stopped any medications since COVID, they could be contributing to head pain.
Vestibular symptoms like dizziness, vertigo, and lightheadedness are common in patients with COVID-19, not only during the acute phase but also as a sign of long-termpost-COVID-19 infection. Some long COVID patients are being diagnosed with “vestibular migraine” after their infection, despite having no risk factors or pre-existing conditions that would contribute to it developing.
Vestibular symptoms are often accompanied by headaches, and sometimes by nausea and sensitivity to light and/or sound. It’s common for patients to experience this headache pain when they wake up.
Under normal circumstances, when you’re asleep, your head moves only minimally. Most of your vestibular system thus does not activate; instead, “non-adaptive fibers” in the utricle and saccule of your ear take over. If this part of the vestibular system was affected by COVID, then you might experience problems during sleep and wake up with headache, dizziness, nausea, or other related symptoms. And if there is an additional imbalance or altered function in your vestibular system, that discomfort might only clear temporarily, only to worsen as you go about your day.
On the other hand, if you wake up feeling fine and then feel worse as the day progresses, it’s more likely that your problems stem from vision dysfunction. The eyes are refreshed overnight, but as they are fatigued during the day, they will contribute more and more to your symptoms. But that’s not to say the vestibular system can’t be the culprit if you wake up feeling fine at first.
Problems with the Eyes
Researchers know that SARS-CoV-2 infection can also have an impact on the eyes. About one in ten patients with COVID-19 experience at least one eye problem, such as conjunctivitis, dryness, redness, and sensitivity to light. In addition, some patients also experience a vision-related type of headache that affects the area behind the eyes.
Predisposition to Migraines
Patients with a history of headaches or migraine attacks are more likely to experience headaches following COVID infection. Alternatively, long COVID may be the ‘trigger’ needed to bring on migraines in a patient with a predisposition to migraines who hadn’t yet experienced them before infection.
Curiously, many patients with pre-existing headaches or migraines notice that headaches caused by COVID feel different. For example, some patients reported less frequency and reduced severity of their headaches after their coronavirus infection. It’s possible that less severe headaches could be due to increased time at home with family during the lockdown or new work-from-home arrangements.
Overuse of Medication
The easiest way to respond to a headache or other long COVID symptoms is to take some over-the-counter painkillers. However, if you do this frequently, you may develop rebound headaches. In other words, the same medicines that initially are useful to relieve mild headaches can trigger subsequent headaches if they’re used too often.
Many different types of medication can lead to rebound headaches, including over-the-counter painkillers such as acetaminophen (Tylenol) and NSAIDs such as ibuprofen (Advil, Motrin) and naproxen (Aleve). Prescription drugs, including ergotamine, triptan, opioids, and combination analgesics can lead to rebound headaches as well.
Why Medication Often Fails
Let's be direct about something most doctors won't tell you: painkillers don't fix long COVID headaches. At best, they temporarily mask symptoms while the underlying dysfunction continues.
Our patients consistently report one of three experiences with medication:
- It helped a little but never fully controlled the headaches
- It didn't help at all and they've tried multiple drugs without improvement
- It made things worse by causing rebound headaches or intolerable side effects
This isn't because the medications are bad. It's because they're targeting the wrong thing.
If your headache stems from neurovascular coupling dysfunction, no painkiller will restore healthy communication between your neurons and blood vessels. If autonomic dysfunction is driving your symptoms, masking the pain does nothing to rebalance your nervous system. If breathing pattern disorders are reducing oxygen delivery to your brain, taking ibuprofen won't teach you to breathe correctly.
Effective treatment requires identifying and addressing root causes. That takes specialized evaluation and targeted intervention, not a one-size-fits-all prescription.
Long COVID Treatment Options for Headache and Other Symptoms

Headaches are common for long-haul patients, as is the use of over-the-counter analgesics to deal with the pain. However, many of our patients complain that the painkillers didn’t really work and may have even caused rebound headaches.
The problem is that these meds may be able to hide the pain for a while, but they don’t fix the problem. If you’re suffering from long COVID, medication can’t solve the problem by itself. You need an experienced healthcare professional who can help you identify the cause of the headaches and provide an appropriate treatment regimen to improve long COVID symptoms.
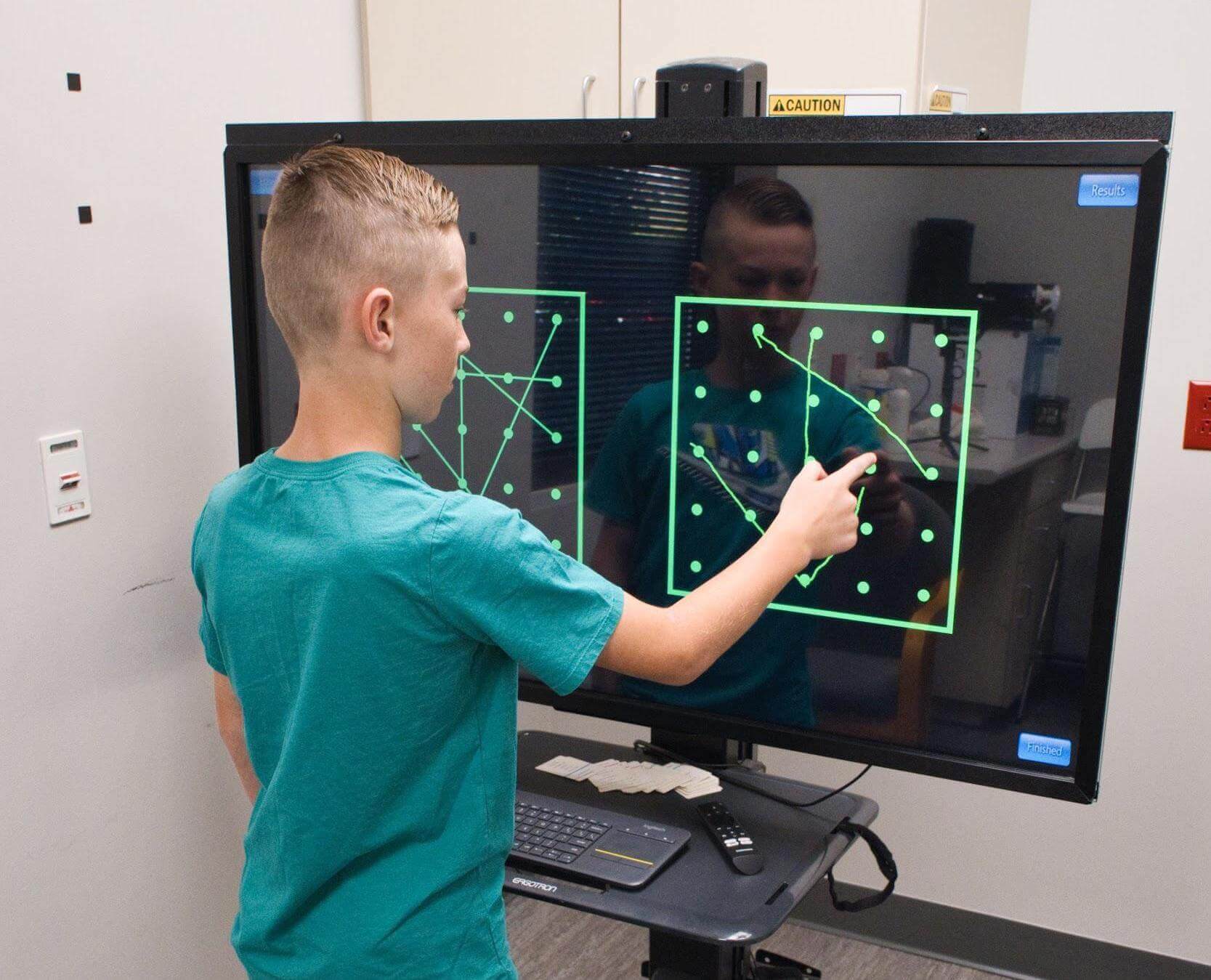
At our clinic, we use targeted, multidisciplinary therapies to treat the most common conditions resulting from brain injury, including neurovascular coupling dysfunction, autonomic nervous system dysfunction, vestibular dysfunction, and vision problems. We have modified our usual protocol specifically for long COVID patients, as they often need more attention to their breathing dynamics due to respiratory symptoms and may have cardiovascular complications that change how they can exercise safely.
Since not every case of long COVID is the same, any patient at our clinic needs to undergo a full evaluation by our team before starting treatment. Unlike most treatment providers, we have access to advanced brain imaging technology so we can determine what effect COVID-19 had on your brain’s vascular health. Here’s an explanation of how that scan works and why it matters for treatment, followed by what happens during treatment.
Why functional NeuroCognitive Imaging (fNCI) Makes a Difference in Post-COVID Treatment

Evidence-Based Treatment Options
The good news: research from 2024-2025 points toward several treatment approaches that actually work for long COVID headaches.
Targeted Preventive Medications
When medication is appropriate, choosing the right one matters enormously.
Amitriptyline remains the best-studied preventive option. A multicenter study documented an average reduction of nearly 10 headache days per month, with 44% of patients achieving at least 50% improvement. Patients with tension-type headache characteristics responded best, and only 5% discontinued due to side effects.
CGRP monoclonal antibodies (fremanezumab, galcanezumab) show impressive results for migraine-like presentations that haven't responded to other treatments. A 2025 study found that monthly headache days dropped from 25 to 5, pain severity fell from 8/10 to 3/10, and medication use decreased dramatically. These are injectable medications typically given monthly.
Triptans work well for acute migraine-like attacks, achieving pain freedom within two hours in about 58% of patients.
The key is matching medication to your specific headache type and avoiding the trap of daily painkiller use that leads to rebound headaches.
Autonomic Nervous System Rehabilitation
For patients with dysautonomia or POTS symptoms alongside their headaches, treating the autonomic dysfunction often resolves head pain as a secondary benefit.
The NIH launched the RECOVER-AUTONOMIC trials in 2024, testing ivabradine (a heart rate-lowering medication) and IVIG (intravenous immunoglobulin) for post-COVID POTS. Early case series data suggest benefit, particularly in patients with autoimmune markers.
Vagus nerve stimulation is emerging as a promising non-drug approach. A 2024 pilot study found that twice-daily transcutaneous stimulation (using a simple ear clip device) for 10 days significantly improved fatigue, cognition, and anxiety in long COVID patients, with benefits sustained at one-month follow-up.
Heart rate variability biofeedback trains you to consciously influence your autonomic balance through controlled breathing and real-time feedback. Long COVID patients consistently show abnormal HRV patterns, and restoring healthy variability appears to reduce symptoms.
Breathing Retraining
Given that dysfunctional breathing affects up to 88% of long COVID patients with unexplained shortness of breath, addressing breathing mechanics is often essential.
Effective approaches include:
- Buteyko breathing technique focusing on nasal breathing and reduced breathing volume
- Resonance frequency breathing at approximately 6 breaths per minute to optimize heart-lung-brain synchronization
- Diaphragmatic breathing exercises to restore normal breathing mechanics
Our treatment protocol at Cognitive FX includes comprehensive breathing assessment and retraining because we've found it's often a missing piece in patients who haven't responded to other interventions.
Vestibular Rehabilitation
If your headaches are accompanied by dizziness or balance problems, vestibular therapy can make a significant difference. This involves specific exercises that "retrain" your brain to correctly process motion and balance signals.
Our therapists use techniques like:
- Balance exercises with progressive difficulty
- Gaze stabilization training
- Habituation exercises for motion sensitivity
- Integration activities that challenge multiple sensory systems simultaneously
Vision Therapy
For headaches driven by visual dysfunction, targeted exercises can relieve eye strain and restore normal visual processing. This might include:
- Visual tracking exercises
- Convergence training
- Exercises using specialized tools like the Brock string
- Dynavision training for visual-motor integration
While significant progress often occurs during our one-week intensive program, vision issues may require ongoing exercises or referral to a neuro-optometrist for complete resolution.
Neuroplasticity-Based Cognitive Rehabilitation
The strongest evidence for any long COVID intervention comes from a randomized controlled trial of computerized brain training with coaching support. Participants showed large improvements across multiple symptoms, with statistically significant cognitive gains that enabled return to work.
The principle is simple: your brain can form new pathways and strengthen connections when given the right stimulus. Passive waiting rarely leads to improvement. Active, targeted rehabilitation does.
Ready to find out what's causing your symptoms? Cognitive FX offers the only treatment approach with third-party validated outcomes for post-concussion syndrome, and we've adapted our protocols specifically for long COVID patients. Schedule your free consultation to learn whether you're a candidate for treatment.
How Brain Imaging Makes Treatment More Effective
Here's what makes our approach at Cognitive FX fundamentally different: we can actually see what COVID did to your brain.
Functional NeuroCognitive Imaging (fNCI)
Standard brain scans like MRI and CT show structure. They're good at finding tumors, bleeds, or physical damage. But they can't reveal dysfunction in how brain regions communicate and function.
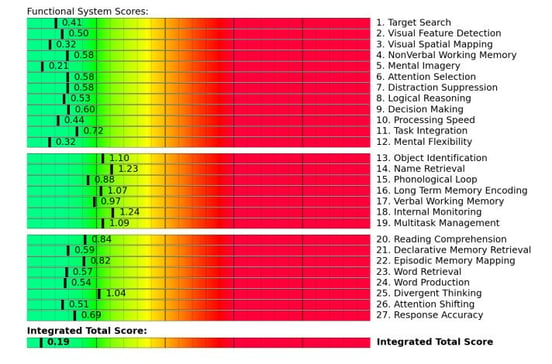
Our fNCI technology measures blood flow dynamics across 56 brain regions while you perform a series of cognitive tasks. This shows us exactly which areas have impaired neurovascular coupling, which regions aren't communicating properly with others, and how the dysfunction maps to your specific symptoms.
Here's why this matters for treatment: instead of guessing what might help, we can design a therapy plan targeting your specific areas of dysfunction. Two patients with identical symptoms might have very different patterns of brain involvement, requiring different therapeutic approaches.
What fNCI Results Look Like
After your scan, we map the data to brain functions like attention, memory, processing speed, and decision-making. Each region receives a score showing how well it's performing compared to healthy function.
Green indicates healthy function. Yellow suggests mild dysfunction. Red signals significant impairment requiring focused treatment.
This imaging guides every aspect of your treatment plan, ensuring therapy time is spent on what will actually help you recover.
Results We See
Among post-concussion patients, 77% experience meaningful symptom improvement after one week of treatment, with an average 60% reduction in symptoms. We've observed similar outcomes in long COVID patients who meet our screening criteria.
Headache improvement specifically tends to occur alongside gains in other areas. As neurovascular coupling normalizes, as autonomic function rebalances, as breathing patterns correct, patients consistently report that their headaches become less frequent, less intense, and more manageable.
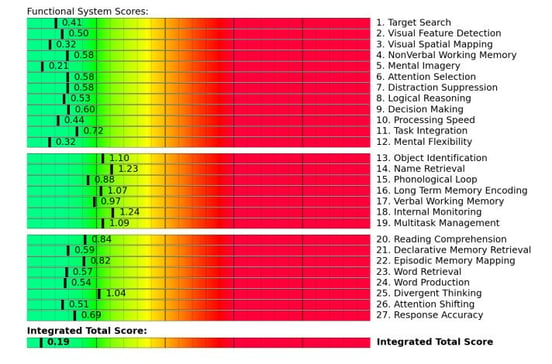
Armed with these results, we can tailor your treatment program to your specific needs. Most of our patients with long COVID report improvements after treatment, including breathing easier, experiencing fewer headaches, and feeling less dizzy and lightheaded.
Treatment for Long COVID at Cognitive FX
Our Treatment Approach: EPIC Protocol
EPIC stands for Enhanced Performance in Cognition, and it represents our comprehensive approach to treating brain dysfunction after injury or illness.
Treatment follows a structured daily cycle:
Prepare: Short bursts of cardiovascular exercise boost blood flow to the brain and trigger release of beneficial neurochemicals. This primes your brain for the therapeutic work to follow.
Activate: Following exercise, you engage in targeted therapies designed to challenge and restore function in your specific areas of dysfunction. This takes advantage of the post-exercise cognitive boost (PECB), when your brain is optimally ready to adapt and learn.
Recover: Periods of rest allow your brain to consolidate gains before the next therapy session. We've found this rhythm of challenge and recovery produces better outcomes than constant stimulation.
What Treatment Includes
Over the course of one week, patients work with specialists across multiple disciplines:
- Neuromuscular therapy addressing physical tension patterns that contribute to headaches
- Cognitive therapy rebuilding attention, memory, and processing capabilities
- Sensorimotor therapy restoring integration between your senses and movement
- Vestibular therapy retraining balance and spatial orientation systems
- Vision therapy addressing eye-tracking and visual processing problems
- Neurointegration therapy teaching breathing techniques and mindfulness practices
- Cardiovascular exercise calibrated to your specific tolerance and needs
Long COVID patients often need modified protocols compared to our typical concussion patients. You may have cardiovascular limitations that change how exercise is incorporated. You may need more intensive breathing work due to respiratory involvement. Our team adjusts everything based on your individual presentation and fNCI results.
What to Expect During Recovery
Recovery from long COVID headaches isn't usually instant, but understanding the typical trajectory helps set realistic expectations.
During Treatment
Most patients notice some improvement during their week of intensive therapy. This might be reduced headache frequency, lower intensity, or simply more energy and clearer thinking. The degree of improvement varies based on the severity and complexity of your dysfunction.
First Weeks After Treatment
Your brain continues to consolidate changes for several weeks after you leave our clinic. Many patients report progressive improvement during this period as new patterns become automatic. We provide specific home exercises to support this process.
Ongoing Recovery
Complete resolution of symptoms typically takes weeks to months, not days. The brain heals gradually. What treatment does is jump-start the recovery process and give your brain the tools it needs to continue improving.
Patients with favorable factors tend to recover faster:
- Lower headache intensity during acute COVID infection
- Tension-type rather than migraine-type headaches
- Absence of chronic daily headache pattern
- Earlier treatment initiation
- Absence of medication overuse
- Good overall health and fitness
Patients with more complex presentations may need longer to fully recover, but improvement is still the typical trajectory.
Risk Factors: Who's Most Likely to Develop Persistent Headaches?
Understanding risk factors helps identify who should seek treatment sooner rather than waiting to see if symptoms resolve.
Female sex is the strongest demographic predictor, with women facing 37% higher risk of persistent post-COVID headaches according to 2025 research. Women aged 40-55 appear particularly vulnerable, possibly related to hormonal changes around perimenopause.
Prior headache history nearly triples the odds of headaches during acute COVID and increases chronic daily headache risk by about 24%. Interestingly, the post-COVID headache often feels different from previous headache patterns.
Severe headaches during initial infection predict worse long-term outcomes. Higher intensity in the first days correlates with greater likelihood of persistence.
Hospitalization roughly triples the risk of developing chronic headaches compared to outpatient COVID cases.
Accompanying symptoms during acute illness, including loss of smell/taste, back pain, insomnia, and tingling sensations, all correlate with higher headache persistence rates.
If you have multiple risk factors and are already several months into your post-COVID headache journey, prompt evaluation and treatment likely offers better outcomes than continued waiting.
Moving Forward
Moving Forward: Your Next Steps
Persistent headaches after COVID aren't something you have to accept as your new normal. The science is clear that these headaches have identifiable causes, and those causes can be treated.
Here's what we recommend:
If your headaches are recent (under 2 months): Focus on good basics including hydration, sleep, gentle movement, and avoiding medication overuse. Many cases resolve in this window without specialized treatment.
If your headaches have persisted beyond 2 months: Spontaneous resolution becomes unlikely. Seek evaluation from a provider who understands the multiple mechanisms behind long COVID symptoms.
If you've tried medications without success: This is a strong signal that the underlying dysfunction hasn't been addressed. Consider evaluation with functional brain imaging to identify what's actually happening.
If headaches accompany other symptoms like brain fog, fatigue, or dizziness: You likely have dysfunction across multiple systems that would benefit from comprehensive, multidisciplinary treatment.
Take the First Step Toward Recovery
At Cognitive FX, we've spent over a decade developing and refining our approach to treating brain dysfunction. Our methods are backed by peer-reviewed research and validated outcomes data showing that 77% of patients experience meaningful improvement.
We've successfully adapted our protocols for long COVID patients, addressing the unique combination of neuroinflammation, neurovascular dysfunction, autonomic imbalance, and breathing pattern disorders that characterize this condition.
Schedule a free consultation with our team to discuss your symptoms and determine whether you're a candidate for treatment. During this call, you'll have the opportunity to:
- Describe your specific symptoms and history
- Learn how our evaluation and treatment process works
- Ask questions about what to expect
- Understand whether our approach is likely to help your situation
You don't have to keep living with headaches that steal your quality of life. Treatment options exist, and they work.
Call us at (385) 375-8590 or book your consultation online to get started.
Related Articles
References
- Silva MTT, et al. Long-Term Persistent Headache After SARS-CoV-2 Infection: A Follow-Up Population-Based Study. European Journal of Neurology. May 2025. DOI: 10.1111/ene.70130
- Ruhnau J, et al. Occurrence of new or more severe headaches following COVID-19 is associated with markers of microglial activation and peripheral sensitization. Journal of Headache and Pain. 2024. DOI: 10.1186/s10194-024-01810-6
- Owens CD, et al. Neurovascular coupling impairment as a mechanism for cognitive deficits in COVID-19. Brain Communications. 2024. DOI: 10.1093/braincomms/fcae080
- Choi H, et al. CGRP monoclonal antibodies for persistent post-COVID headache. Journal of Korean Medical Science. 2025. DOI: 10.3346/jkms.2025.40.e127
- Gonzalez-Martinez A, et al. Amitriptyline for post-COVID headache: effectiveness, tolerability, and response predictors. Journal of Neurology. 2022. DOI: 10.1007/s00415-022-11225-5
- Zheng Q, et al. Transcutaneous vagus nerve stimulation improves Long COVID symptoms in a female cohort: a pilot study. Frontiers in Neurology. 2024. DOI: 10.3389/fneur.2024.1393371
- NIH RECOVER Initiative. Long COVID trials to evaluate treatments for autonomic nervous system dysfunction. March 2024. https://recovercovid.org/
- Carvalho GF, et al. Persistent headache and chronic daily headache after COVID-19: a prospective cohort study. Korean Journal of Pain. July 2024. DOI: 10.3344/kjp.24046
- Kim Y, et al. Gender Disparities in Neurological Symptoms of Long COVID: A Systematic Review and Meta-Analysis. Neuroepidemiology. 2025.
- NICE/SIGN/RCGP. COVID-19 rapid guideline: managing the long-term effects of COVID-19. Updated January 2024.