While recovering from COVID-19, you may find yourself getting breathless easily from activities that didn’t used to tire you, like carrying laundry or walking up the stairs.
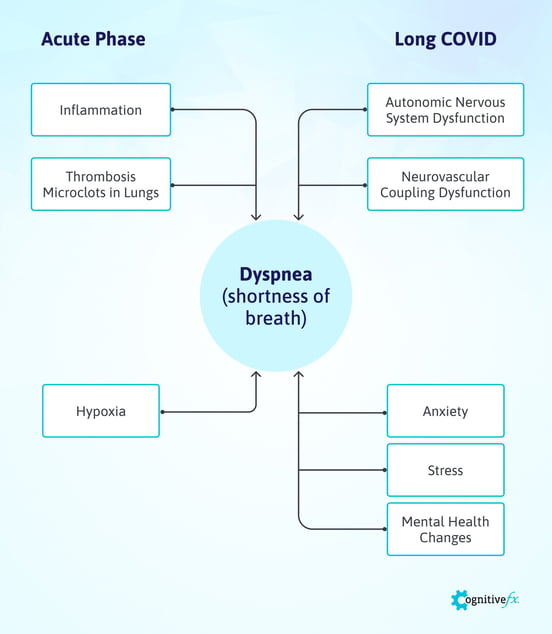
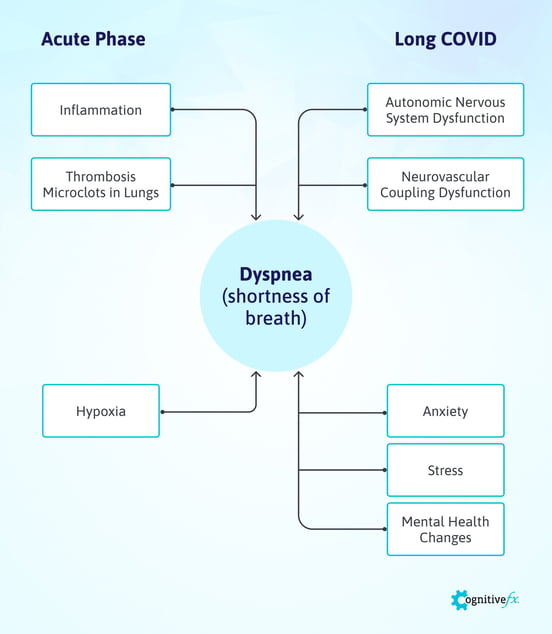
That’s because COVID-19 can significantly impact the respiratory system. Many patients suffer the effects of lung damage during the acute phase, including shortness of breath and coughing. This is likely due to a combination of the body’s exaggerated immune system reaction to the virus and blood clots that obstruct oxygen intake in the lungs. Fortunately, the symptom is usually short-lived.
For patients who go on to develop long COVID, however, this may become a long-term symptom affecting quality of life. There’s limited research to be able to say for sure, but in this case, shortness of breath may be linked to interference with brain blood flow or problems related to the autonomic nervous system.
As a result, many Long COVID patients have a dysfunctional breathing pattern. In this case, breathing control exercises can be very effective in helping to restore normal breathing patterns, which is why they are an integral part of the treatment we offer at Cognitive FX.
In this article, we’ll look at:
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What Does It Feel like to Have Shortness of Breath?

Not many sensations are as frightening as not being able to breathe. Shortness of breath — medically known as dyspnea — is often described as air hunger, difficulty breathing, or a feeling of suffocation.
Each person with COVID-19 experiences dyspnea in a slightly different manner. For some, it’s a mild symptom that comes and goes, while for others, it’s a severe, persistent feeling.
If you feel breathless, you might notice any of the following sensations:
- Your chest feels tight.
- You can’t inhale or exhale properly.
- It’s difficult to take a deep or satisfying breath.
- It is hard to control your breathing.
- You feel exhausted easily.
- You feel anxious.
- Your heart feels like it’s always racing.
It's important to get immediate help if you’re experiencing rapid, labored breathing accompanied by pain or tightness in your chest or if you need to catch your breath constantly. These symptoms may indicate a severe condition that requires immediate treatment.
How Does COVID-19 Cause Shortness of Breath during the Acute Phase?
Intense exercise, high altitudes, or extreme temperatures can all cause shortness of breath in a healthy person, but it's only a temporary symptom that goes away within a few minutes (except when it’s caused by altitude, as that may last up to two weeks).
For 37% of COVID-19 patients, however, shortness of breath is a serious and persistent problem, especially if accompanied by other symptoms, such as fever, cough, and fatigue. Difficulties with breathing may start anytime after an infection appears; appearance at 5 days is the median.
It’s more prevalent in older and frailer patients, as well as in patients who are overweight or who have pre-existing medical conditions, such as diabetes, hypertension, and cardiovascular disease. At this stage, patients with severe shortness of breath are more likely to develop a critical illness and need hospitalization.
In COVID-19 survivors, the virus may cause a wide range of long-term respiratory problems in addition to shortness of breath, including lung diseases such as acute respiratory distress syndrome (ARDS) and pulmonary fibrosis. A small proportion of patients may even need supplemental oxygen due to persistent hypoxemia (below normal oxygen levels in the blood).
Scientists believe there are two main mechanisms by which the coronavirus triggers breathlessness during the acute phase of the infection: inflammation in the lungs and formation of microclots.
Shortness of Breath Caused by Inflammation
SARS-CoV-2, the virus that causes COVID-19, enters your body through the upper airways, starting with the nose and mouth. As the infection travels down your respiratory tract, your immune system starts to fight back and triggers an inflammatory response.
The problem is, as the inflammation progresses, the lungs become swollen and filled with fluid and debris from dead cells, which quickly prevents gas transfer in the lungs, making it harder to breathe.
If the transfer of oxygen into the bloodstream is severely reduced, patients may need supplemental oxygen and close monitoring in the hospital. Severe cases may require ventilator support in intensive care.
In the long term, there is also a chance that patients could develop permanent scarring in the lungs due to this inflammatory response. This scarring causes stiffness in the lungs and makes it difficult to get oxygen to the bloodstream, resulting in breathlessness long after the infection is cured.
Thrombosis and Microclots in the Lungs
As well as causing severe respiratory problems, COVID-19 also seems to trigger abnormalities in blood clotting. Studies show that as many as 30% of critically ill patients develop blood clots in veins and arteries, increasing the risk of heart attacks and strokes. If a blood vessel carrying blood to or from the lungs is blocked by a clot, it can cause sudden and intense breathing problems.
Typically, these clots are bigger than 1mm in size and can be detected by a CT scan. However, healthcare providers are becoming increasingly aware that smaller clots — named microclots — can be just as dangerous and virtually impossible to see. If these microclots start to develop in the capillaries in the lung, they may block gas exchange, ultimately leading to shortness of breath.
Doctors are concerned that standard blood-thinning medication to prevent these clots doesn't seem to work in COVID-19 patients. Some hospitals are giving patients much higher doses than normal, and clinical trials testing different doses of blood thinners are currently underway.
The Mystery of Patients With “Happy” Hypoxia
Despite the intense research done over the past two years, the COVID-19 pandemic still holds many mysteries. One of them refers to patients who should be struggling to breathe because they present with very low oxygen levels but show no signs of respiratory distress. This phenomenon has become known as silent or “happy” hypoxia.
Researchers believe that the respiratory center in the brain doesn’t recognize immediately that blood oxygen levels have reduced and/or carbon dioxide levels have increased. As oxygen levels continue to drop, the brain remains unresponsive until oxygen falls to dangerously low levels. If these patients do not receive prompt medical care, their condition is associated with rapid clinical worsening and often a fatal outcome.
How Does COVID-19 Cause Shortness of Breath in Long COVID Patients?

Shortness of breath is not exclusive to patients during the acute phase. In fact, it’s much more common among Long COVID patients, and two-thirds of long COVID patients only experience this symptom weeks or even months after the original illness.
Research is extremely limited with Long COVID patients, but two factors that frequently come up as the most likely explanation for shortness of breath in these patients are dysfunction of the autonomic nervous system and disruption of neurovascular coupling in the brain. These are also the two main factors behind the cases of long-term symptoms from mild traumatic brain injuries, hypoxia, and infectious diseases that we treat at Cognitive FX.
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Autonomic Nervous System Dysfunction
Like our patients with a mild traumatic brain injury, many Long COVID patients typically show signs of autonomic nervous system dysfunction.
The autonomic nervous system (ANS) is divided into the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS is often described as driving the “fight or flight” response, whereas the PNS leads to a calmer “rest and digest” reaction.
In other words, the SNS prepares the body for action by increasing heart rate, dilating pupil size, and stimulating breathing patterns. In contrast, the PNS helps the body slow down, and it includes functions like stimulating digestion, lowering heart rate, and reducing breathing rates.
The autonomic nervous system interacts with almost every organ in the body.
In Long COVID patients, ANS dysfunction usually involves an overactive SNS, while the PNS becomes more subdued. This condition, known as dysautonomia, can manifest itself through many symptoms, such as blood pressure changes, heart palpitations, exercise intolerance, incontinence, temperature sensitivity, and shortness of breath.
Slow, deep breathing stimulates the activity of the vagus nerve, which is part of the PNS. The vagus nerve controls the activity of many internal organs, and when this nerve is stimulated, it can lower heart rate, improve blood pressure, and regulate breathing patterns.
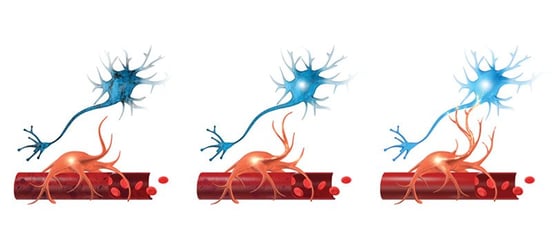
Neurovascular Coupling Dysfunction
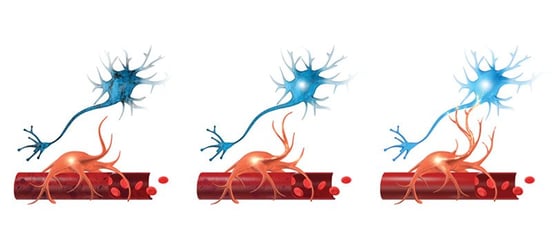
Although the exact mechanism is not yet fully understood, researchers believe shortness of breath in Long COVID patients may also be the result of disruption to the blood supply of oxygen to the the brain, causing some areas to lose the ability to complete the tasks expected of them. This is known as neurovascular coupling dysfunction.
We have seen this kind of disruption firsthand with our Long COVID patients. We explain in more detail later in the article, but before treatment starts, every patient undergoes a brain scan to detect which areas are affected. In all of our Long COVID patients, brain imaging revealed the same pattern of neurovascular coupling disruption that we detect in concussion patients. You can read more about how we found a viable treatment for COVID-19 Long-Haulers.
Studies show that the feeling of shortness of breath is controlled in multiple areas in the brain, including the amygdala, the cingulate cortex, the hypothalamus, and the anterior insula, to name just a few. If these areas happen to be affected by neurovascular coupling dysfunction, it may trigger shortness of breath without necessarily being accompanied by low oxygen levels in the blood.
Anxiety, Stress and Other Behavioral Issues
One last factor that may cause shortness of breath is an indirect consequence of living with Long COVID. Facing the prospect of losing your job or experiencing financial difficulties because you’re struggling with a case of COVID-19 can have a significant impact on mental health and well-being. In fact, one study found that 1 in 3 COVID-19 survivors end up diagnosed with a psychiatric condition within six months of being infected.
When patients feel anxious, heart rate increases, which in turn stimulates breathing rate and triggers shortness of breath. Some patients also feel increased tightness in different muscles, including the neck and chest, which may further aggravate breathing difficulties.
To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Treatment at Cognitive FX for Long COVID

At Cognitive FX, we treat patients with mild traumatic brain injuries.
When we noticed that common symptoms of COVID-19 weeks after acute infection were similar to the complaints we hear from our brain injury patients, we established that they could be treated in a very similar way.
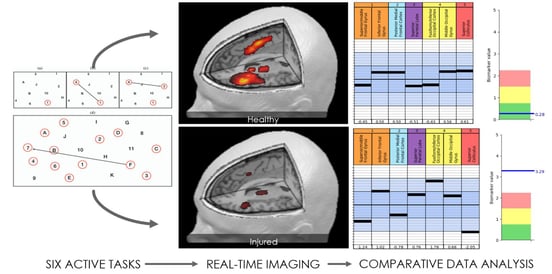
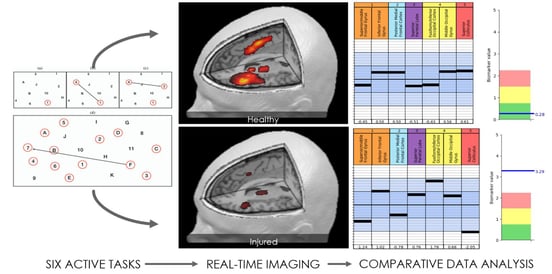
When Long COVID patients come to us, the first step is a functional Neurocognitive Imaging (fNCI) scan. While the scan was designed to detect dysfunction due to mild traumatic brain injury, signs of Long COVID-19 show up on the fNCI as well.
When patients complete the scan, they perform cognitive tasks so we can spot which regions are still operating normally and which are either under or overactive. These patients also undergo a detailed interview to assess medical history and track symptoms progression, in addition to several physiological and cognitive assessments.
With this information, our therapists can design a customized treatment plan to target the affected areas detected by the scan. Our multidisciplinary treatment takes one to two weeks to complete and includes various types of therapies, such as vision therapy, occupational therapy, cognitive therapy, neuromuscular therapy, sensorimotor therapy, and psychotherapy. We also spend time teaching patients breathing techniques.

Some of the ways we adapted our post-concussion syndrome protocol to better meet the needs of Long COVID patients include:
- Shorter cardio: Many Long COVID patients struggle with physical activity, so we offer shorter bursts of exercise (high intensity interval training) with a longer recovery period.
- Extra neuromuscular therapy: Long COVID patients also get additional neuromuscular therapy if they complain of neck pain.
- Adapted referral process: If we feel that our patients could benefit from further treatment, we always refer to specialists at the end of treatment. Most of our concussion patients don’t need to be referred, and those who do, need it mainly for vision therapy. In contrast, we’ve seen that many of our Long COVID patients need to be referred to vision therapy as well as continue meeting for a time with Cognitive FX specialists in person or via telehealth appointments.
- Greater focus on breathing techniques: Long COVID patients who suffer from shortness of breath benefit from extra time and attention on their breathing.
On the last day of treatment, patients repeat their fNCI scan to see how much their brain has improved. So far, the 17 patients who have already completed the treatment saw their scans improve by 112% and reported symptoms cut down by half. It’s still too early to quantify long-term recovery results, but we continue to monitor our patients and improve our treatment program.
Breathing Techniques to Do at Home

Unlike digestion or blood pressure, breathing is an unusual body function in that it is both involuntary and voluntary. Most of the time, we breathe without thinking about it, but at any point, we can consciously change our breathing pattern.
There are several breathing techniques that can help restore diaphragmatic breathing and increase lung capacity. These exercises also lessen feelings of anxiety and stress, which are common in Long COVID patients. These activities can be done anywhere and are easily incorporated into a daily routine.
Just remember that these exercises are not a replacement for medical advice or medical attention, especially if you are having severe symptoms.
Relaxed, slow, deep breathing: This is a quick technique you can easily perform anywhere. Find a comfortable position and relax your shoulders. Then, gently breathe in through your nose, and breathe out through your mouth. Repeat as many times as needed.
Deep breathing: The idea behind this exercise is to maximize the amount of oxygen entering the body and the amount of carbon dioxide leaving. It includes three parts: (1) start by inhaling deeply through the nose while counting to 5; (2) hold your breath briefly; (3) and finish by exhaling through your mouth longer than the inhalation. This activates the parasympathetic nervous system and counteracts the sympathetic nervous system’s fight or flight response (as described earlier).
Pursed-lips breathing: Breath in through your nose, then out through your mouth with your lips pursed, as if you’re whistling. It may help to imagine you are trying to gently make a candle flame flicker without actually blowing it out fully. This is an excellent technique to help slow down your breathing.
Blow as you go: This technique is ideal for doing something that needs a lot of effort, like opening a jar or picking up a heavy bag. Breathe in before you start and breathe out while you’re doing it.
Paced breathing: Breath in and out, keeping in time with whatever you’re doing. For example, walking upstairs, breathe in on one step and breathe out on the next step. We recommend spending fifteen minutes per day breathing in a 4-6-1 pattern: four seconds in, six seconds out, and one second hold before repeating.
Cooling your face: Cooling your face, especially around the nose, will make you feel less breathless. Try placing a cool, wet cloth on the nose and upper cheeks of your face or sitting in front of a fan for a few minutes.
What Else Can I Do?

Here are a few more ways you can improve your breathing:
Stay active: Regular exercise can help prevent episodes of breathlessness, increase your energy levels, and improve your overall health. Don’t worry about how hard you exercise when you start; slowly working up to cardio can be very beneficial.
If you smoke, stop: Smoking damages your lungs, causes mucus to build up in your airways, and makes breathlessness worse.
Eat a healthy and balanced diet: Extra weight located around the abdomen and chest areas can put your lungs under more strain and worsen breathlessness. A healthy diet will boost your energy levels and help your body heal from illness.
Pace Yourself: Avoid the pattern of doing too much one day, then nothing for the next few days because you feel too tired. Instead, try to pace yourself and spread what you have to do over a few days.
Manage anxiety: It’s normal to feel anxious if you think your breathing is out of control. Doing breathing exercises, listening to relaxing music, and using mindfulness techniques can help you stay in control.
Track your post-COVID symptoms: Record how you feel with different activity levels, stress, time of day, etc. This will help you identify triggers, which in turn can help you plan your daily activities more effectively.
Frequently Asked Questions
What are the most common symptoms of Long COVID?
The most common symptoms of Long Covid include shortness of breath, fatigue, and sleep disorders, but researchers have identified over 200 possible symptoms. Long COVID-19 affects virtually any organ in the body.
Some of the symptoms reported by COVID long-haulers include:
- Anosmia (lack of sense of smell)
- Blood clotting (deep vein thrombosis and pulmonary embolism)
- Body aches
- Changes in mood (including depression, anxiety, panic attacks, and other mental health problems)
- Changes in oral health
- Chest pains
- Diarrhea and bouts of vomiting
- Dry cough
- Extreme fatigue
- Headaches
- Heartburn
- Inability to concentrate (brain fog)
- Joint pain
- Kidney problems (acute kidney injury and chronic kidney disease)
- Long lasting cough
- Loss of taste and smell
- Low grade fever
- Memory lapses
- Muscle weakness
- Needle pains in arms and legs
- New onset of diabetes and hypertension
- Palpitations
- Parosmia (change in sense of smell)
- Sleep difficulties
- Sore throat and difficulties swallowing
- Tinnitus
- Trouble breathing or shortness of breath
Who gets Long COVID?
Long COVID is a new disorder, so we don’t have much data to answer this question yet. Current research suggests that Long COVID is more likely with age. Women and patients with pre-existing health conditions are twice as likely to develop lingering symptoms from a COVID-19 infection.
You do not have to have a life-threatening, severe COVID-19 case in order to develop Long COVID. In the United States, the Centers for Disease Control and Prevention (CDC) found that at least a third of non-hospitalized patients were still struggling to return to full health after a few weeks.
Does the COVID-19 vaccine help prevent Long COVID?
The short answer is yes.
UK researchers looked at data from over 900,000 people who received both doses of the vaccine and found that their risk of developing Long COVID was reduced by half if they actually caught COVID-19. Most common symptoms were similar to those experienced by unvaccinated adults — including loss of smell, cough, headaches, and fatigue — but symptoms in vaccinated adults were milder, and there were fewer hospitalizations.
We recommend keeping your vaccination against coronavirus disease up-to-date if you and your doctor agree that it’s best for you.
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.