You used to power through 10-hour workdays. Now you're exhausted after emptying the dishwasher.
You've tried sleeping more, drinking more coffee, taking every supplement the internet recommended. Nothing works. Your doctor says your labs look "normal," but you know something is deeply wrong.
If this sounds familiar, you're not imagining it. And you're far from alone.
Post-COVID fatigue affects nearly half of all COVID-19 survivors, making it the most common and persistent symptom of Long COVID. But here's what most people don't realize: this isn't ordinary tiredness. It's a measurable biological dysfunction that shows up on advanced brain imaging, and it responds to targeted treatment.
At Cognitive FX, we've treated hundreds of Long COVID patients using the same functional brain imaging and multidisciplinary rehabilitation approach that has helped thousands of post-concussion patients recover. The connection isn't coincidental. Both conditions disrupt the same brain systems, and both respond to the same evidence-based treatments.
In this comprehensive guide, you'll learn:
Struggling with Long COVID symptoms? Our team of 12 specialists uses functional brain imaging to identify exactly what's happening in your brain, then creates a customized treatment plan. Take our free consultation quiz to see if you're a candidate for treatment.
What Does Post-COVID Fatigue Feel Like?

Long COVID fatigue is fundamentally different from ordinary tiredness. Patients describe it as:
"My battery drains in hours instead of days." You wake up feeling like you slept for two hours when you actually slept for ten. Basic activities like showering, cooking, or having a conversation can deplete your energy reserves completely.
"It's like running on 20% power." Your body feels heavy. Your brain feels foggy. Tasks that used to take minutes now take hours, and you make mistakes you never used to make.
"Rest doesn't fix it." This is the hallmark of post-COVID fatigue. Unlike normal tiredness, sleeping more doesn't restore your energy. You can spend an entire weekend in bed and still feel exhausted on Monday.
The Physical Symptoms
- Persistent, crushing exhaustion that doesn't improve with rest
- Muscle weakness and heaviness
- Headaches (often daily)
- Dizziness and lightheadedness, especially when standing
- Heart palpitations and racing heart
- Shortness of breath with minimal exertion
- Body aches and joint pain
The Cognitive Symptoms
- Brain fog (difficulty thinking clearly)
- Problems with short-term memory
- Difficulty concentrating or paying attention
- Word-finding difficulties
- Slower mental processing speed
- Feeling mentally "blank"
The Behavioral Symptoms
- Low motivation
- Irritability and mood swings
- Social withdrawal
- Difficulty handling stress
- Sleep disturbances (too much or too little)
Key Point: If your symptoms get significantly worse 12-72 hours after physical or mental exertion, you're likely experiencing post-exertional malaise (PEM). This affects approximately 80% of Long COVID fatigue patients and requires a different treatment approach than standard fatigue. Keep reading to learn why this matters.
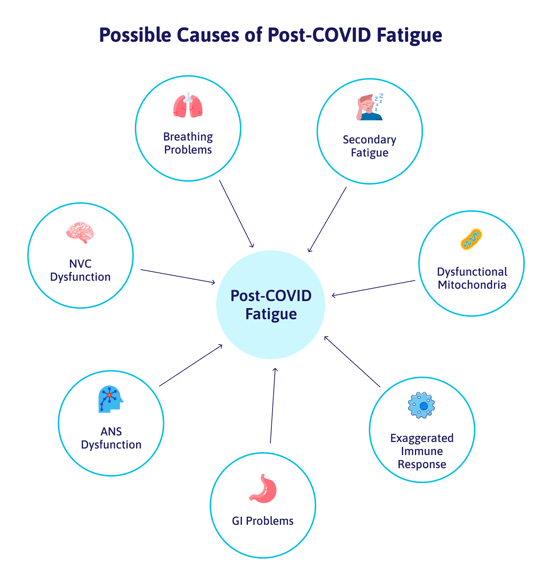
What causes post-COVID fatigue?
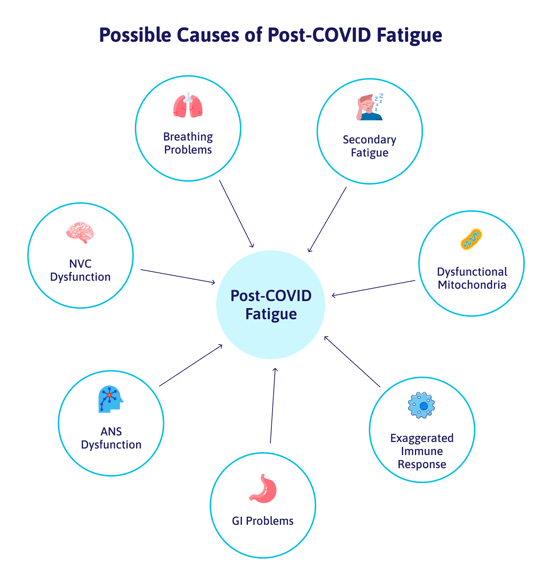
What Causes Long COVID Fatigue? The Science
For years, Long COVID patients were told their symptoms were psychological. The latest research proves otherwise. Scientists have now identified six distinct biological mechanisms that explain why you feel so exhausted.
1. Mitochondrial Dysfunction: Your Cells Can't Make Energy
Your mitochondria are the power plants inside every cell, converting food into usable energy (ATP). A landmark 2024 study from Amsterdam UMC found that mitochondria in Long COVID patients produce significantly less energy than healthy controls, and this dysfunction gets worse after exercise.
This explains why you feel depleted after activities that shouldn't be tiring. Your cells literally cannot generate enough fuel.
Research citation: Mitochondrial dysfunction in long COVID: mechanisms, consequences, and potential therapeutic approaches (GeroScience, 2024)
2. Neuroinflammation: Your Brain Is Still Fighting
Advanced PET imaging studies show that Long COVID patients have elevated markers of brain inflammation, particularly in areas controlling attention, memory, and energy regulation. Inflammatory chemicals called cytokines cross the blood-brain barrier, keeping your brain in a state of "sickness behavior" long after the virus is gone.
This chronic inflammation disrupts normal brain function and contributes to both physical fatigue and brain fog.
Research citation: Neuroinflammation in post-acute sequelae of COVID-19 (PASC) as assessed by PET (Brain, Behavior, and Immunity, 2024)
3. Autonomic Nervous System Dysfunction
Your autonomic nervous system controls everything you don't consciously think about: heart rate, blood pressure, digestion, breathing. In Long COVID patients, this system becomes dysregulated.
The most common manifestation is POTS (Postural Orthostatic Tachycardia Syndrome), which affects approximately 30% of highly symptomatic Long COVID patients. When you stand up, your heart races, you feel dizzy, and your body struggles to regulate blood flow. This keeps you in a constant state of physiological stress, draining your energy reserves.
Research citation: Treatment of long COVID complicated by postural orthostatic tachycardia syndrome (2024)
4. Neurovascular Coupling Disruption
In a healthy brain, blood vessels automatically deliver more oxygen and nutrients to active brain regions. This coordination is called neurovascular coupling (NVC).
COVID-19 can disrupt this system, causing a mismatch between what your brain needs and what it receives. When you try to concentrate, think, or problem-solve, the affected brain regions don't get adequate blood flow. The result? Mental exhaustion from tasks that should be easy.
At Cognitive FX, we use functional NeuroCognitive Imaging (fNCI) to identify exactly which brain regions have impaired neurovascular coupling. This allows us to create targeted treatment plans.
5. Microclots and Vascular Damage
Researchers have discovered that some Long COVID patients have microscopic blood clots (microclots) that resist normal breakdown. These tiny clots can block capillaries throughout the body, reducing oxygen delivery to tissues.
A 2025 study found that exercise may actually fragment (but not clear) these microclots, potentially explaining why physical exertion worsens symptoms in some patients.
6. Persistent Immune Dysregulation
Your immune system may remain in a state of chronic activation months or years after COVID infection. Studies show elevated inflammatory markers in over half of Long COVID patients more than three months post-infection.
This sustained immune response depletes cellular energy and maintains the malaise you feel, similar to how you feel exhausted when fighting any illness.
The Bottom Line: Long COVID fatigue isn't "just tiredness" or "in your head." It involves measurable dysfunction in multiple body systems. The good news? When you can identify what's going wrong, you can treat it effectively.
How long does post-COVID fatigue last?

How Long Does Fatigue Last After COVID?
This is the question every Long COVID patient asks, and the honest answer is: it varies significantly.
The Statistics (2024-2025 Research)
For most COVID patients: Fatigue resolves within 2-4 weeks after the acute infection. If you're reading this article, you're probably not in this group.
For Long COVID patients: The timeline is much longer and less predictable.
- 75.9% report severe fatigue at 3-6 months post-infection
- 57.1% still experience fatigue at 9-12 months
- 26% report fatigue at follow-up times exceeding one year (actually higher than the 19% at earlier timepoints)
A sobering finding from the NIH RECOVER study: only 1.8% of Long COVID patients experience complete symptom resolution. However, this doesn't mean improvement isn't possible, just that some residual symptoms often persist.
Research citation: Global Prevalence of Long COVID, its Subtypes and Risk factors: An Updated Systematic Review and Meta-Analysis (2025)
Why Some People Recover Faster Than Others
Several factors influence recovery time:
Factors associated with longer duration:
- Female sex (OR: 1.55-11.11 across studies)
- Pre-existing conditions (diabetes, cardiovascular disease, obesity)
- Severity of initial infection
- Number of symptoms during acute infection
- Being unvaccinated (2.34x higher odds of Long COVID)
- Lack of early treatment
Factors associated with better outcomes:
- Early intervention
- Targeted rehabilitation
- Proper pacing and energy management
- Treatment of underlying autonomic dysfunction
The Critical Insight
Recovery from Long COVID is rarely linear. You'll have good days and bad days. Pushing too hard on good days often leads to crashes. The patients who recover fastest are those who:
- Get proper diagnosis and treatment early
- Learn to manage their energy (pacing)
- Address all contributing factors, not just one symptom at a time
How to Recover from Post-COVID Fatigue

There's no FDA-approved medication specifically for Long COVID fatigue. However, multiple treatment approaches have shown significant benefits in clinical research.
1. Multidisciplinary Rehabilitation (Strongest Evidence)
A systematic review with meta-analysis found that after comprehensive rehabilitation, only 17% of patients reported persistent fatigue compared to nearly all at baseline. That's a dramatic improvement.
What makes rehabilitation effective is the multidisciplinary approach: combining physical therapy, occupational therapy, cognitive therapy, and other specialties based on each patient's specific deficits.
Research citation: Impact of Rehabilitation on Fatigue in Post-COVID-19 Patients: A Systematic Review and Meta-Analysis (Applied Sciences, 2022)
2. Pacing and Energy Management (Essential for PEM)
If you experience post-exertional malaise (symptoms worsening after activity), pacing is critical. The World Health Organization explicitly states that graded exercise therapy should NOT be recommended for patients with post-exertional symptom exacerbation.
Survey research shows that 74% of patients with PEM actually deteriorate with traditional graded exercise programs.
Instead, effective approaches include:
- The STOP-REST-PACE method
- "Energy envelope" management
- Activity logging to identify triggers
- Strategic rest before and after demanding activities
Research citation: Post-exertional malaise may persist in Long COVID despite learning STOP-REST-PACE (Fatigue: Biomedicine, Health & Behavior, 2023)
3. Transcranial Magnetic Stimulation (TMS) - Promising Emerging Treatment
TMS uses magnetic pulses to stimulate specific brain regions. Early research in Long COVID patients shows encouraging results:
- A pilot study of 12 patients receiving high-frequency rTMS demonstrated significant decreases in fatigue scores, improved cognitive function, and enhanced cerebral blood flow visible on brain imaging
- A Japanese registry study of 23 patients reported fatigue performance status improving from 5.4 to 4.2 with theta burst stimulation
These are small studies and need larger trials to confirm, but the early signals are positive.
Research citation: Effect of Repetitive Transcranial Magnetic Stimulation on Long COVID with Fatigue and Cognitive Dysfunction (2023)
4. Autonomic Nervous System Treatments
For patients with POTS or other autonomic dysfunction, targeted treatments include:
- Increased fluid and salt intake
- Compression garments
- Medications like ivabradine (currently in clinical trials)
- Specific physical therapy for reconditioning
The NIH RECOVER-AUTONOMIC trial is currently testing these interventions in 380 participants.
5. Addressing Underlying Dysfunction
The most effective treatment approach addresses all contributing factors:
- Breathing dysfunction: Respiratory therapy, breathing exercises
- Sleep disruption: Sleep hygiene, treating sleep disorders
- Vestibular problems: Balance and coordination therapy
- Vision issues: Neuro-optometric rehabilitation
- Cognitive deficits: Targeted cognitive exercises
.
How Cognitive FX Treats Long COVID Fatigue
At Cognitive FX, we recognized early in the pandemic that Long COVID affects the brain in remarkably similar ways to post-concussion syndrome, the primary condition we've treated since 2014. Both conditions involve:
- Neurovascular coupling dysfunction
- Autonomic nervous system dysregulation
- Neuroinflammation
- Similar symptom profiles (fatigue, brain fog, headaches, dizziness)
This isn't coincidental. Researchers at the University of Denver found that Long COVID patients show similar deficits on concussion assessment tests and experience 60-70% improvement using concussion rehabilitation protocols.
Our Approach: The EPIC Treatment Protocol
EPIC (Enhanced Performance in Cognition) is our intensive, one-week treatment program adapted for Long COVID patients. Here's what makes it different:
Step 1: Functional Brain Imaging (fNCI)
Before treatment begins, every patient undergoes our proprietary functional NeuroCognitive Imaging (fNCI) scan. This advanced fMRI-based assessment identifies:
- Which brain regions have impaired function
- The severity of neurovascular coupling dysfunction
- How different brain areas are (or aren't) communicating
Unlike standard MRI or CT scans that only show structure, fNCI shows function. This allows us to create a precisely targeted treatment plan.
Step 2: Comprehensive Evaluation
Our team of 12 different specialists evaluates every aspect of your condition:
- Neuropsychological function
- Autonomic nervous system dynamics
- Vestibular (balance) function
- Vision and eye tracking
- Breathing patterns
- Physical conditioning
- Cognitive processing
We look for everything that wouldn't show up on a brain scan but contributes to your symptoms.
Step 3: Intensive Multidisciplinary Treatment
Treatment follows our proven Prepare-Activate-Recover cycle:
Prepare: Short bursts of aerobic exercise promote healthier blood flow to the brain and trigger the release of brain-derived neurotrophic factor (BDNF), which supports healing.
Activate: Immediately after exercise, you engage in targeted therapies designed to challenge and rehabilitate the specific brain systems identified on your fNCI. This takes advantage of "post-exercise cognitive boost," when your brain is primed for change.
Recover: Built-in rest periods allow your brain to consolidate gains and prevent overexertion.
Throughout the week, you rotate through multiple therapies including:
- Neuromuscular therapy
- Sensorimotor therapy
- Cognitive rehabilitation
- Vision therapy
- Vestibular therapy
- Occupational therapy
- Psychological support
Step 4: Post-Treatment fNCI and Home Program
At the end of treatment, a second fNCI scan documents your improvement. Our therapists then meet with you to create a customized home exercise program to continue your recovery.
Why Intensive Treatment Works for Long COVID
You might wonder: "If I'm exhausted, how can I handle intensive treatment?"
This is a valid concern. The key is our structured approach:
- We carefully calibrate exercise intensity to each patient's current capacity
- Rest periods are built into every day
- Therapies are sequenced to maximize benefit while preventing crashes
- We monitor for signs of overexertion and adjust accordingly
Every Long COVID patient we've treated has been able to complete the program. Most notice improvement during the treatment week.
Ready to find out if Cognitive FX can help you? Schedule a free consultation with our team to discuss your symptoms and determine if you're a candidate for treatment.
What can I do to manage post-COVID fatigue?

While professional treatment offers the fastest path to recovery, there's much you can do on your own. These strategies are supported by research and clinical experience.
Energy Management (Pacing)
Track your "energy envelope." For one week, log your activities and energy levels. Note what depletes you and what helps you recover. This identifies your limits.
Plan ahead. If you have an important event, rest before and after. Don't stack demanding activities on consecutive days.
Break tasks into smaller pieces. Instead of cleaning the house in one session, do one room, rest, then continue another day.
Stop before you crash. If you feel good, the temptation is to do more. Resist it. Overdoing it on good days leads to crashes that can last days or weeks.
Sleep Optimization
Maintain strict sleep-wake times. Go to bed and wake up at the same time every day, including weekends.
Limit daytime naps. If you must nap, keep it under 30 minutes and before 3 PM.
Create a wind-down routine. Dim lights, avoid screens, and do calming activities for an hour before bed.
Consider melatonin. Low-dose melatonin (0.5-3mg) 30-60 minutes before bed may help regulate your sleep cycle.
Breathing Exercises
Controlled breathing activates your parasympathetic nervous system (rest and digest mode), countering the sympathetic overdrive common in Long COVID.
Try 4-6-1 breathing:
- Breathe in for 4 seconds
- Breathe out for 6 seconds
- Hold for 1 second
- Repeat for 5-10 minutes
Humming, singing, or gargling stimulates the vagus nerve, which helps regulate autonomic function. It sounds simple, but research supports it.
Nutrition and Hydration
Stay well hydrated. Dehydration worsens fatigue and autonomic symptoms. Aim for at least 2-3 liters of water daily.
Consider increasing salt intake (if you have POTS symptoms and no contraindications like high blood pressure). This helps maintain blood volume.
Eat regular, balanced meals. Blood sugar swings worsen fatigue. Include protein and complex carbohydrates at each meal.
Limit alcohol and caffeine. Both can worsen sleep and autonomic dysfunction.
Gentle Movement (With Caution)
If you have post-exertional malaise: Start very conservatively. Even 5 minutes of gentle walking may be too much initially. Work with a physical therapist who understands PEM.
If you tolerate activity: Gentle, low-intensity movement can help. Swimming, recumbent cycling, and walking are often better tolerated than upright exercise.
Always listen to your body. If activity consistently makes you worse, stop and consult a healthcare provider familiar with Long COVID.
Supplements (Consult Your Doctor First)
Some supplements show promise for Long COVID fatigue, though evidence remains preliminary:
- Coenzyme Q10: Supports mitochondrial function
- Magnesium: May help with muscle function and headaches
- B vitamins: Essential for energy metabolism
- Vitamin D: Often depleted in Long COVID patients
- Omega-3 fatty acids: Anti-inflammatory effects
Always consult your healthcare provider before starting supplements, especially if you take medications.
Mental Health Support
Long COVID is exhausting emotionally as well as physically. Depression and anxiety are common, and they can worsen fatigue.
Don't isolate. Stay connected with friends and family, even if just by phone or video call.
Consider therapy. A mental health professional can help you process the challenges of chronic illness and develop coping strategies.
Join a support group. Connecting with others who understand your experience can be profoundly helpful. Many online communities exist for Long COVID patients.
Track Your Progress
Keep a symptom diary. Note your energy levels, activities, sleep, and symptoms daily. This helps identify patterns and triggers.
Celebrate small wins. Recovery isn't linear. Acknowledge improvements, even small ones.
Don't compare yourself to your pre-COVID self. Focus on where you are now versus a month ago.
The Long COVID-ME/CFS Connection
If your symptoms persist, you should know about the significant overlap between Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
A 2024 meta-analysis found that 51% of Long COVID patients meet diagnostic criteria for ME/CFS. Both conditions share:
- Fatigue that doesn't improve with rest
- Post-exertional malaise
- Brain fog and cognitive difficulties
- Unrefreshing sleep
- Orthostatic intolerance
The NIH RECOVER Initiative documented a 15-fold increase in ME/CFS incidence post-pandemic.
Why does this matter? Because three decades of ME/CFS research can inform Long COVID treatment. Approaches that help ME/CFS patients (pacing, autonomic support, avoiding overexertion) often help Long COVID patients too.
Research citation: The persistence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) after SARS-CoV-2 infection: A systematic review and meta-analysis (Journal of Infection, 2024)
Frequently Asked Questions
Is Long COVID fatigue the same as being tired?
No. Normal tiredness improves with rest. Long COVID fatigue doesn't. It's a biological condition involving mitochondrial dysfunction, neuroinflammation, and other measurable abnormalities.
Can Long COVID fatigue cause brain fog too?
Yes, they're closely connected. Many of the same mechanisms (neuroinflammation, neurovascular coupling disruption, autonomic dysfunction) cause both symptoms. Most Long COVID patients with fatigue also experience cognitive difficulties.
Should I exercise if I have Long COVID fatigue?
It depends on whether you have post-exertional malaise (PEM). If activity consistently makes you worse 12-72 hours later, traditional exercise can be harmful. Work with a physical therapist who understands Long COVID and PEM.
How do I know if I have Long COVID or something else?
Long COVID is a diagnosis of exclusion. Your doctor should rule out other conditions like thyroid dysfunction, anemia, sleep disorders, and depression. If no other cause is found and symptoms persist 3+ months after COVID infection, Long COVID is likely.
Will I ever fully recover?
Many people do improve significantly with time and proper treatment. Complete resolution of all symptoms is less common (1.8% in one study), but meaningful improvement in function and quality of life is achievable for most patients.
How is Cognitive FX different from other Long COVID clinics?
We use functional brain imaging (fNCI) to identify exactly where brain function is impaired, then target treatment to those specific areas. Our intensive, one-week program delivers months of rehabilitation in a concentrated format, and our team of 12 specialists addresses every aspect of your condition.
When to Seek Treatment
Consider seeking professional treatment if:
- Your fatigue has lasted more than 3 months
- Rest doesn't restore your energy
- You experience post-exertional malaise
- Brain fog affects your work or daily life
- Your symptoms are getting worse, not better
- Self-management strategies aren't helping enough
Early intervention is associated with better outcomes. Don't wait years hoping symptoms will resolve on their own.
Take the Next Step
Long COVID fatigue is real, it's biological, and it's treatable.
At Cognitive FX, we've helped hundreds of Long COVID patients reclaim their energy, their cognition, and their lives using the same evidence-based approach that has helped thousands of post-concussion patients over the past decade.
Our intensive treatment program combines:
- Functional brain imaging (fNCI) to identify exactly what's wrong
- 12 different specialists addressing every aspect of your condition
- Customized treatment based on your unique brain function
- Proven protocols adapted from our successful concussion rehabilitation program
95% of our patients show statistically verified improvement in brain function after just one week of treatment.
You don't have to keep suffering. You don't have to keep waiting for symptoms to resolve on their own. Help is available.
Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Always consult with qualified healthcare providers regarding diagnosis and treatment options for your specific situation.