When the pandemic started, we were told that children wouldn’t be seriously affected by the virus. And while most children only experience a mild version of the disease, evidence shows that some children are at risk of developing persistent symptoms after their initial COVID-19 infection.
In other words, children can get long COVID (sometimes called post-acute COVID-19). Months after their initial viral infection, some children continue to struggle with symptoms such as fatigue, headaches, brain fog, and abdominal pain, to name just a few.
Many parents are now facing the challenge of getting a diagnosis for their children. Diagnosing long COVID in children and adolescents is difficult because the symptoms resemble those of other conditions, such as attention deficit hyperactivity disorder (ADHD).
During the diagnostic process, your child’s doctor may ask for a variety of tests, including blood tests, measurements of blood oxygenation levels, and a chest x-ray. While these tests can help shed light on what’s happening, none of them can determine with certainty that your child is suffering from long COVID.
At Cognitive FX, we follow a different strategy. We use a special type of MRI brain scan to determine what parts of the brain were affected by the virus. We also evaluate the patient’s vision and autonomic nervous system, both of which can be affected by long COVID. Then, we design a custom treatment plan to target any issues we find.
We’ve already demonstrated that this approach works for long COVID patients, including some younger than 18 years old.
For more information on how we developed our treatment program and stories from long COVID patients, see these articles:
In this article, we focus on long COVID in children. Specifically, we answer the following questions:
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, these patients report a 60% improvement in symptoms on average. Thus far, we’ve seen similar results with long COVID patients who pass our screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Yes, Children Can Get Long COVID

Fewer cases of COVID-19 have been reported in children than in adults, but children can still get infected. In most cases, when children have a mild or even asymptomatic disease, they recover within one to two weeks. For these young patients, fatal cases are extremely rare.
According to CDC data for April 2022, out of over 12 million cases of COVID-19, there were only 1,501 coronavirus-associated deaths in patients younger than 18 years of age.
Despite these figures painting a picture of a relatively harmless disease for children, it has now become clear that even these young patients — many of them previously healthy — can show signs of long-term issues caused by the virus.
A study in the UK involving over 3,000 11-to-17-year-olds who tested positive for COVID found that about 14% of teenagers were still experiencing fatigue, persistent headaches, and shortness of breath more than three months after their positive PCR test.
The Israeli Health Ministry also released their own survey: Out of over 13,000 participants aged 3 to 18-years, 11% of children experienced some symptoms of long COVID in the weeks following recovery and about 4% still had symptoms six months later.
With the emergence of the new Omicron variant and subvariant BA.2 — which are more infectious than previous forms of Covid-19 — the number of children with COVID is increasing, which will likely lead to increased prevalence of long COVID in children.
To address this problem, the National Institutes of Health (NIH) started a study to track up to 1,000 children and young adults who tested positive for COVID-19, following them for three years. The idea is to assess long-term sequelae on health and quality of life after a COVID infection.
Doctors are also investigating whether COVID-19 vaccines can help reduce lingering symptoms in children suffering from long COVID. This approach seems to help some adults struggling with the effects of long COVID, most likely by eliminating any remaining viral particles by boosting antibodies in the body.
When It’s Not Long COVID
Long COVID is not the only health issue for parents to worry about during this pandemic. Although rare, a small number of children also suffer from Multisystem inflammatory syndrome in children (MIS-C) after their COVID infection. Typically, this happens about 2 to 6 weeks after the SARS-CoV-2 infection, and it represents less than 0.1% of pediatric cases of COVID.
In these children, internal organs such as the heart, lungs, kidneys, digestive system, and brain can become severely inflamed. In some extreme cases, it can be fatal. Doctors don’t know exactly what’s causing MIS-C, but it seems to be a consequence of an excessive immune response to fight COVID.
Initial symptoms include fever, dizziness, headaches, skin rashes, and vomiting. If your child has severe stomach pain, difficulty breathing, or cannot stay awake, get medical care immediately. Take your child to the nearest ER or call 911. They might require intensive care to recover.
Definition of Long COVID in Children

Scientists at University College London, UK, recently came up with the first standardized definition for long COVID in children. It closely follows the definition proposed by the World Health Organization (WHO) for long COVID in adults. It is hoped that this will make it easier for doctors and scientists to assess the disease and understand how children are affected by it.
They defined long COVID as a condition in which a young person has at least one physical symptom that:
- Developed after a diagnosis of COVID-19 (confirmed with at least one positive COVID test).
- Has an impact over their physical, mental, or social wellbeing.
- Interferes with some aspect of daily living, including school, work, or at-home activities.
- Persists for at least 12 weeks after initial testing for COVID-19 (including if symptoms waxed and waned over that period).
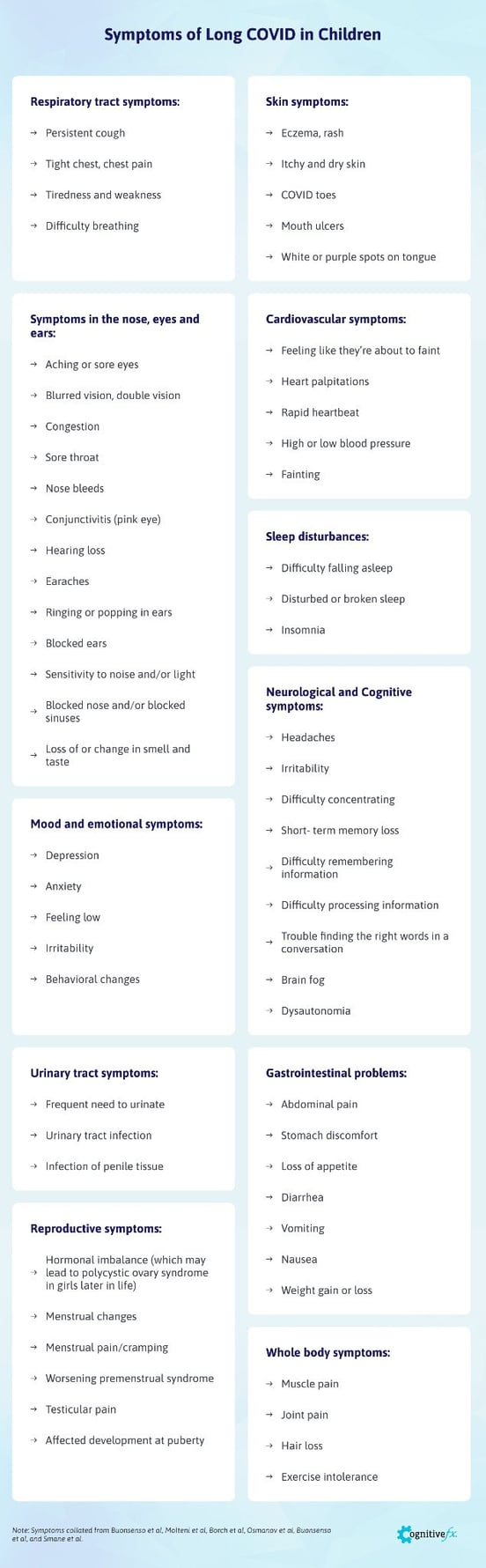
Symptoms of Long COVID in Children
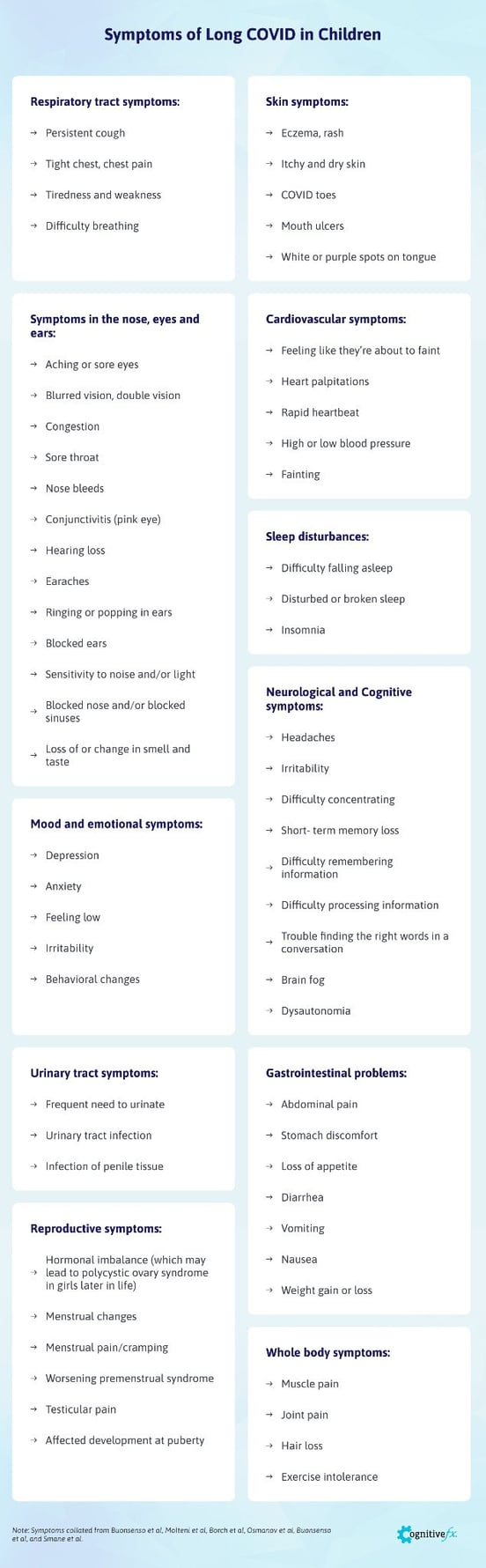
Post-COVID symptoms in adults include symptoms such as fatigue, muscle and joint pain, headache, insomnia, respiratory problems, and heart palpitations, to name just a few. Most long COVID research is based on adult long haulers, and for a long time there was limited information about patients under the age of 18.
In recent months, however, there have been several studies from research groups around the world looking at COVID-19 symptoms experienced by children. Combining all these studies, the list of symptoms in long COVID kids includes:
Respiratory Tract Symptoms
- Persistent cough
- Tight chest, chest pain
- Tiredness and weakness
- Difficulty breathing
Skin Symptoms
- Eczema, rash
- Itchy and dry skin
- COVID toes
- Mouth ulcers
- White or purple spots on tongue
Symptoms in the Nose, Eyes and Ears
- Aching or sore eyes
- Blurred vision, double vision
- Congestion
- Sore throat
- Nose bleeds
- Conjunctivitis (pink eye)
- Hearing loss
- Earaches
- Ringing or popping in ears
- Blocked ears
- Sensitivity to noise and/or light
- Blocked nose and/or blocked sinuses
- Loss of or change in smell and taste
Cardiovascular Symptoms
- Feeling like they’re about to faint
- Heart palpitations
- Rapid heartbeat
- High or low blood pressure
- Fainting
Sleep Disturbances
- Difficulty falling asleep
- Disturbed or broken sleep
- Insomnia
Neurological and Cognitive Symptoms
- Headaches
- Irritability
- Difficulty concentrating
- Short-term memory loss
- Difficulty remembering information
- Difficulty processing information
- Trouble finding the right words in a conversation
- Brain fog
- Dysautonomia
Mood and Emotional Symptoms
- Depression
- Anxiety
- Feeling low
- Irritability
- Behavioral changes
Urinary Tract Symptoms
- Frequent need to urinate
- Urinary tract infection
- Infection of penile tissue
Gastrointestinal Problems
- Abdominal pain
- Stomach discomfort
- Loss of appetite
- Diarrhea
- Vomiting
- Nausea
- Weight gain or loss
Reproductive Symptoms
- Hormonal imbalance (which may lead to polycystic ovary syndrome in girls later in life)
- Menstrual changes
- Menstrual pain/cramping
- Worsening premenstrual syndrome
- Testicular pain
- Affected development at puberty
Whole Body Symptoms
- Muscle pain
- Joint pain
- Hair loss
- Exercise intolerance
At Cognitive FX, we’ve seen many of these symptoms in our younger patients. For our very young patients — younger than 8 years old — parents report mostly emotional symptoms, like anxiety and personality changes, and physical symptoms, like fatigue and headaches. These patients are too young to be able to explain their post-COVID condition. If they’re struggling to focus or can’t think properly, for example, they express it with angry outbursts.
In contrast, teenagers — older than 12 years old — are able to explain what they’re feeling. The most common symptoms they’ve reported to us include chronic fatigue, brain fog, and difficulty concentrating at school. They also report mental health changes, such as feeling sad and depressed.
Note: Symptoms collated from Buonsenso et al, Molteni et al, Borch et al, Osmanov et al, Buonsenso et al, and Smane et al.
How Does Long COVID Affect Children?

Exactly how children develop long-haul COVID symptoms is still a mystery.
There are a series of theories regarding why long COVID occurs in adults, ranging from an excessive immune reaction from the body to disruption of normal neurovascular coupling in the brain or dysfunction of the autonomic nervous system (ANS). We’ve explained this in more detail in some of our previous articles, looking at how long COVID causes fatigue, dysautonomia, and other symptoms.
The same may be true for children, but researchers are not entirely convinced that long COVID in children is always caused by the same mechanisms as in adults. The symptoms experienced by children and adults are slightly different. Many adults experience brain fog and other neurological issues, whereas children with long COVID are more likely to experience at least one gastrointestinal issue, such as abdominal pain, diarrhea, and/or vomiting.
There is one study in particular where the researchers found that young children with long COVID symptoms have a biomarker in their blood which is associated with a leaky gut (a condition which allows microbes from the GI tract to move into the bloodstream and spread around the body). According to the authors, COVID-19 may be considered a respiratory disease in adults, but this finding suggests it may be more of a gastrointestinal problem in children.
Young patients also report many cognitive issues, such as brain fog or difficulty concentrating and learning new information. We often see these types of cognitive symptoms in patients who come to us after months or even years of suffering the long-term effects of a concussion.
For these post-concussion patients, the main problem is disruption of neurovascular coupling (NVC) — the connection between brain cells and the blood vessels that surround them. NVC ensures brain cells receive the oxygen and nutrients they need. Without these essential items, the brain cannot perform its normal activities.
In a healthy brain, NVC can deliver the right amount of oxygen and energy at the right time and to the right place, ensuring the brain can perform a particular task. In long COVID patients — both adults and children — we can see that neurovascular coupling is disrupted. We believe neurovascular coupling dysfunction is one of the main causes of symptoms in long COVID patients.
NVC dysfunction can cause a series of long-term problems in adults, but it may be even worse in children as their brain is not yet fully developed. It’s still too early to determine the long-term effects in children living with long COVID, but we can expect similar problems as in children who have experienced other conditions that also disrupt normal NVC in the brain, such as a traumatic brain injury.
Problems with concentration, attention, coordination and short-term memory are common, as well as headache, light-headedness, dizziness, and problems breathing, to name just a few. These difficulties can persist over time, sometimes into adulthood.
Long COVID in Children is Difficult to Diagnose

During the acute phase of the infection, diagnosis is easy. Parents should test their children if they notice some of the hallmark symptoms of COVID-19, including a persistent cough, fever, and loss of smell and taste.
But long COVID diagnosis becomes extremely difficult, because:
- Symptoms are not specific to long COVID. Symptoms like headaches, fatigue, and brain fog can be explained by a variety of other conditions. This makes it very difficult to distinguish between long COVID and other conditions.
- Young children can’t explain their symptoms very well. Physical symptoms like stomachache or cough are easy to describe, but 8-year-olds or younger don’t understand cognitive or emotional issues, such as difficulty understanding new information or feeling anxious.
- The pandemic itself may cause similar symptoms, especially cognitive and emotional problems. For example, difficulty concentrating at school may be due to wearing a mask or online learning with limited social contact with friends. Other symptoms may be the result of social isolation, a poor diet, or less exercise.
- Pediatric long COVID is a new condition. Many healthcare professionals don’t believe long COVID affects children. You’re more likely to get medical help either a) from a doctor who has known your child their whole life and who can recognize subtle changes, or b) from a doctor who is actively researching or at least advertises treating long COVID.
- Finally, symptoms may not show immediately after the acute infection. It can take weeks for symptoms to show, and they can come and go, making it harder to attribute them to the initial COVID infection.
Getting a Diagnosis at Cognitive FX

Any children who start experiencing symptoms such as persistent headache, fatigue, sleep disturbance, difficulty in concentrating, and stomach pain a few weeks after their original infection should be assessed for possible long COVID.
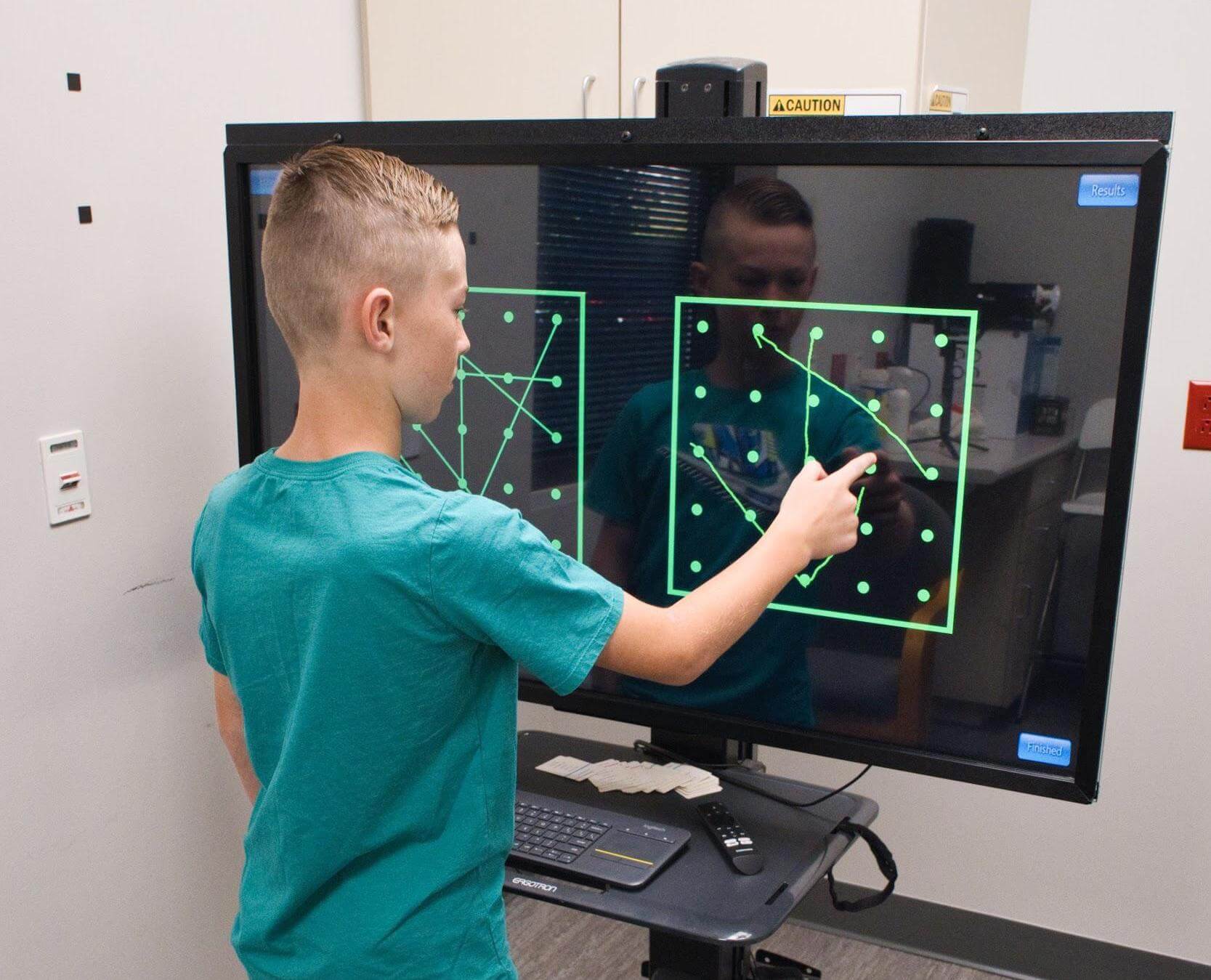
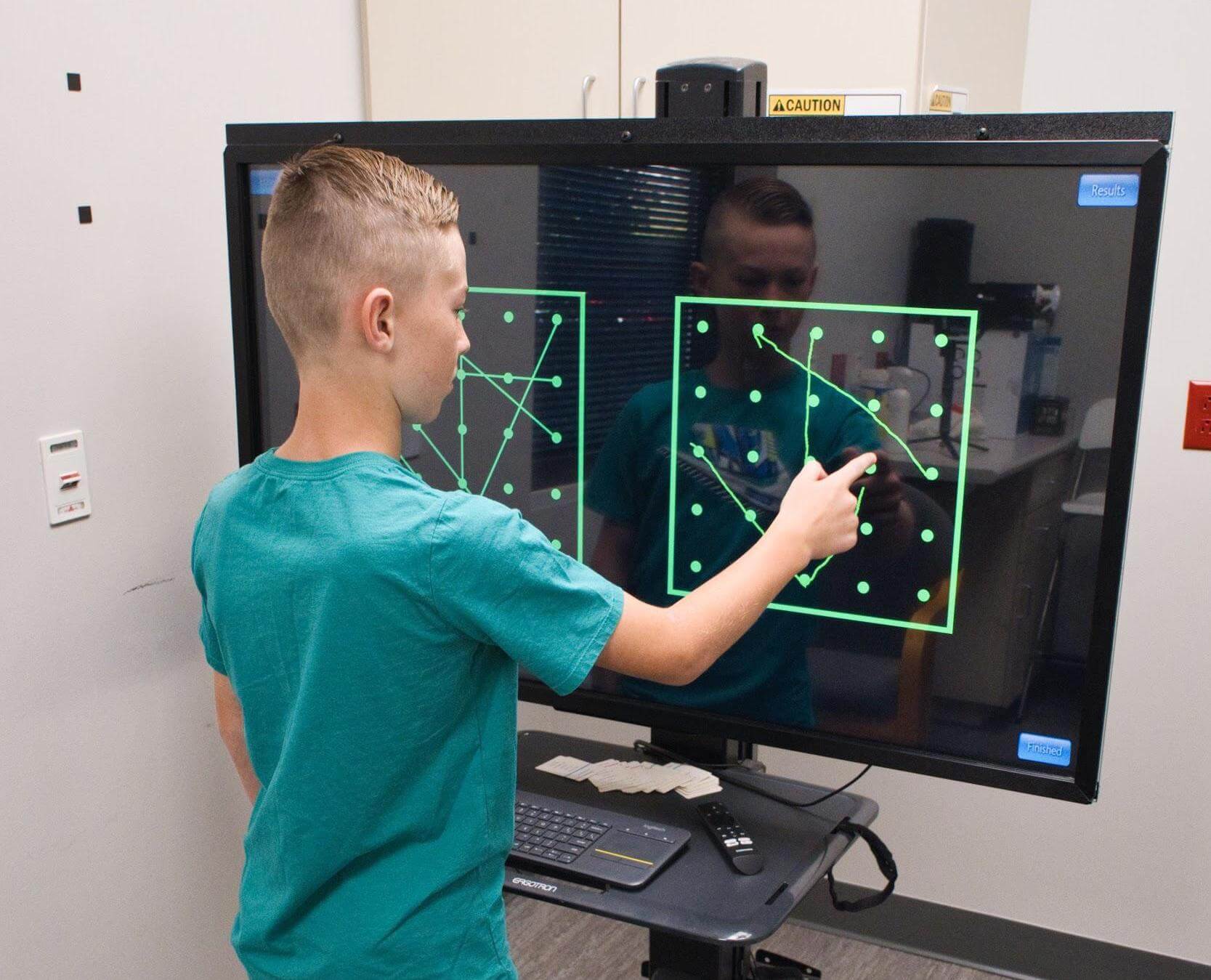
At Cognitive FX, we have a special type of brain scan — called functional Neurocognitive Imaging (fNCI) — to detect dysfunctional neurovascular coupling. In turn, we can interpret that information to understand how your child’s brain has been affected by the virus. (Note that the most accurate pediatric data is at age 14 and above. Children younger than 14 years of age may have unusual fNCI findings because their brain is still rapidly developing. We hope to improve scan reliability for children as we’re able to get more control data for pediatric patients.)
During the scan, patients must complete a series of cognitive tasks while our therapists image 56 regions of the brain. The scan looks both at individual brain regions and the connections between them, allowing us to assess brain function with a high degree of specificity.
In addition, patients also undergo an interview with one of our therapists to discuss medical history, symptoms, and what to expect from treatment.
The final step in the assessment includes a series of physical tests to assess vision, autonomic, and vestibular function. With all this information, our team of experts then designs a treatment plan to target the areas of your child’s brain that were most impacted by COVID-19.
Treatment for Long Covid in Children
Not surprisingly, long COVID is not an easy condition to treat. Instead of treating individual symptoms, we aim to address the root of the problem: NVC dysfunction, autonomic nervous system dysfunction, and vision changes.
With this in mind, during treatment, we call it Enhanced Performance in Cognition (EPIC) Treatment, patients undergo multiple types of therapies, including vision therapy, occupational therapy, cognitive therapy, neuromuscular therapy, sensorimotor therapy, psychotherapy, and more.
Although essentially the same as for adults, we use age-appropriate activities for each type of therapy. For example, we’ve found that patients younger than 18 years old need more attentional exercises because their brain is not fully developed yet.
Especially for younger children (under 12 years old), parents can choose to accompany their children to all the sessions. We often recommend that parents not attend therapy sessions for older teenagers, but we do require your presence at the initial evaluation meeting and at the post-treatment results and recommendations conversation.

On the last day, patients undergo a follow-up fNCI to see how much each area of the brain has improved. Although we see significant improvements in their symptoms, we often find that progress in these young patients is slower than in adults.
This finding goes against long-held views that children are more resilient and capable of healing faster than adults because of their greater capacity for neuroplasticity. This could be because a child’s brain is in constant interaction with the environment and learns with each new experience. This is essential for personal development but makes the brain very vulnerable to disruption, including the negative changes caused by long COVID.
In adults with a mature brain, long COVID has an impact on already established communication pathways between nerve cells. This gives the brain many opportunities to find alternative pathways and recover normal functioning in areas affected by the virus.
In contrast, in children, long COVID affects an immature brain. This not only disrupts the network already established, but also limits the development of new communication pathways. This means finding alternative pathways or restoring affected ones is harder for young patients. As a consequence, recovery may be somewhat longer.
For this reason, at the end of the treatment, our therapists meet with you and your child to discuss how you can continue recovery at home. We make specific recommendations for a daily therapy and exercise routine, as well as share resources for better nutrition and sleep.
What Can Parents Do at Home?

The pandemic has affected children in many ways, and for those suffering the effects of long COVID, it’s even worse. Don’t push your child to resume all activities too quickly after their illness, particularly if they continue experiencing symptoms.
- If you think your child may have long COVID, keep notes about symptoms and patterns. This information will be a valuable addition to your doctor’s diagnostic process. Also, ask other adults in your child’s life, like teachers and sports coaches, if they’ve noticed any changes in your child’s behavior.
- If your child is showing any signs of mental health problems, like being withdrawn and losing interest in hobbies, seek help from a psychologist.
- If your child plays sports at a competitive level, it may be better to reduce their training schedule or stop for a while. If they really enjoy the sport, however, try to find a participation level they can sustain without making their symptoms significantly worse.
- Make sure your child is getting enough support from their school, especially if they need extra help with school work. This may include, for example, increased time for tests or tutoring for some subjects.
Depending on what symptoms your child is experiencing, you may need access to different types of testing and treatment. Here are some links to the most common types you may need:
|
Type of Therapy
|
More Information
|
|
Please see the hyperlinked headings for help finding each type of therapy and testing.
|
|
Vision therapy
|
Many children develop visual processing issues after COVID-19 which may develop immediately after infection or months later. Certified vision therapists can evaluate and treat such visual symptoms.
|
|
Physical therapy
|
If children develop exercise intolerance after COVID-19, a physical therapist can provide monitored therapy sessions and activities that your child can do at home.
|
|
Psychology
|
Whether mood changes are due to Long COVID or environmental changes as a result of the pandemic, psychological support can help children process emotional disruption.
|
|
Hormone and blood tests
|
COVID-19 can affect organs in the body that regulate and produce hormones that are essential for growth and development. While some pediatricians may be able to order blood tests, you may want to consult an endocrinologist for a more specialized opinion.
|
|
Nutritionist
|
The pandemic has changed how and what we eat. Poor nutrition can exacerbate poor outcomes of COVID-19, so accessing nutrition resources can be beneficial for both children and their families.
Look for a pediatric Registered Dietitian Nutritionist (RDN), also known as a child nutritionist or dietitian. They generally treat children from birth until the age of 18 and consider nutrition and dietetics most pertinent to the areas of growth or disease a particular patient is experiencing.
|
|
Pediatrician
|
Pediatricians are often at the front lines of pediatric Long COVID. Keeping your pediatrician in the loop with your child's symptoms and asking them about local resources for therapy (including ones mentioned above) can help get your child the best care.
|
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, these patients report a 60% improvement in symptoms on average. Thus far, we’ve seen similar results with long COVID patients who pass our screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.












.png?height=175&name=Physical%20therapy%20covid%20(2).png)




