How COVID-19 affects the brain | Cognitive FX
A growing body of scientific evidence suggests some COVID-19 patients will experience neurological signs or symptoms of the infection. Genetic material from SARS-CoV-2, the virus that causes...

You’d think a family of eight with the foresight to pull their children out of school earlier than the rest of the nation would be safe during the COVID-19 pandemic. Instead, seven out of the eight family members contracted the coronavirus at the very beginning of the pandemic, back when testing was frustratingly difficult to obtain, and our knowledge about the disease was limited.
Unfortunately, the Sharp family members weren’t just some of the first to catch COVID-19: they were also some of the first to develop Long COVID, a condition where COVID-19 symptoms persist for months, and new symptoms develop at any time affecting many internal organs, such as the heart and the brain.
We sat down with Sarah Sharp, the family’s matron, and two of her older children, Madison Sharp (21) and Boston Sharp (19), to learn what Long COVID looked like for them and how they found relief through treatment at Cognitive FX.
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
 The Sharps’ story began when Madison developed a bad cough in January 2020. The young Mormon missionary working in Germany and Switzerland dismissed it as just a cold, but when the cough persisted for over a month, she looked for medical help. After blood tests and an x-ray, doctors blamed bronchitis. But the antibiotics they gave her had no impact.
The Sharps’ story began when Madison developed a bad cough in January 2020. The young Mormon missionary working in Germany and Switzerland dismissed it as just a cold, but when the cough persisted for over a month, she looked for medical help. After blood tests and an x-ray, doctors blamed bronchitis. But the antibiotics they gave her had no impact.
In the meantime, Madison started noticing other symptoms (though she didn’t realize they were related). She had always been a voracious reader, but suddenly, every time she tried to read something, she couldn’t focus. Even reading the same paragraph multiple times didn’t improve her understanding.
After weeks of no improvement — and still lacking a clear diagnosis — Madison was finally sent home. "My lungs were very weak," Madison explained. Her family was worried about borders closing, so they were happy she returned when she did.
The good news is that Madison did not infect her family with COVID-19 when she returned. The bad news? They had already caught it.
By the time Madison got back home in March, the whole family was fighting off COVID. Just a few days before, her mother, Sarah, had taken drastic measures to care for her family: “I pulled my kids out of school because I wanted to protect my family and also I wanted to protect my neighbors,” she said. But shortly after the children stopped attending school, 12-year old Mercedes and Sarah started showing the first signs of infection.
At the same time, they learned Madison had been in contact with a known COVID case just days before her flight home, necessitating a COVID test. Sarah tried to get tested as well, but at this stage, doctors were only testing people who had a cough, fever, a recent history of travel abroad, and known contact with an infected person. As nobody in the Sharp household matched all the criteria, getting tested was virtually impossible. Initially, Madison was the only person tested due to her confirmed exposure to the virus.
Madison tested positive, but Sarah still believes her results were caused by a lingering virus or recent exposure rather than an active COVID case. We know now that some people continue to test positive after the original illness for weeks or even months afterward, which could explain Madison’s results after contracting COVID-19 while still in Germany.
Meanwhile, Sarah had all the signs of a COVID infection. “I was three days into a cold that my 12-year-old had brought home from school. My symptoms included a sustained fever of 101.8, a solid cough, an increasing heaviness in my chest, and shortness of breath. I was filling the car with the virus as we drove to the testing site.”
One week later, the Health Department offered the family of eight three more tests. Sarah and two of her sons, Talmage and Titan, tested positive.
 “Then the hell began. We all got infected with COVID-19”, said Sarah. “And I was probably the sickest of all.”
“Then the hell began. We all got infected with COVID-19”, said Sarah. “And I was probably the sickest of all.”
She can barely remember the second week of her illness. Her blood pressure swung up and down, she was plagued with a constant cough, intense fatigue, and she spent her nights gasping for air. An oximeter showed her oxygen levels flexing between 89% and 92%, dropping as low as 82% throughout her illness.
In addition to all these symptoms, Sarah also started experiencing heart irregularities. At the time, her doctors insisted that COVID-19 doesn't affect the heart, and they wrote it off as anxiety.
“Nobody knew anything about COVID, and that was probably the hardest part,” Madison said. “I watched my mom's blood pressure freak out, and it was the weirdest thing I've ever seen. Her pulse was low and blood pressure was very high. And everyone said that it doesn't affect your heart; it only affects your lungs. But I knew that wasn’t true because I was seeing it!”
Sarah believes she had oxygen deprivation for as many as four days of her illness. In the following weeks, she participated in a sleep study that showed her oxygen levels dropping randomly without any explanation. She continued to experience persistent heart issues for 13 months post-infection. Curiously, after the second vaccine, most of her heart-related symptoms faded.
Although several symptoms resolved after vaccination, Sarah still had a lingering feeling that something was wrong. “After my illness, I couldn’t explain it, but I knew something was wrong. I felt like something was wrong with my brain. I just felt different.” After months of reading as much information about COVID-19 as she could find, Sarah believed the virus had somehow affected her autonomic nervous system.
As suggested by the name, the autonomic nervous system (ANS) is the part of the nervous system that controls internal organs without any conscious recognition. The ANS can be subdivided into the sympathetic (SNS) and the parasympathetic nervous systems (PNS). The SNS prepares the body to handle stressful situations by, for example, increasing heart rate, dilating the lungs, and releasing stress hormones. In contrast, the PNS calms the body by reducing heart rate, stimulating digestion, and lowering breathing patterns.
Autonomic nervous system dysfunction (known as dysautonomia) could undoubtedly explain many of her symptoms. Sarah was struggling with a laundry list of symptoms, many tied in with the ANS:
It even got to the point that she would find herself mid-conversation but forget who she was talking to and why.
“What I now know is that COVID-19 gave me a brain injury,” said Sarah. “I had a brain injury, which was why I had all these different issues.”
But as Sarah started putting the puzzle pieces together about what was happening to her, her daughter Madison and son Boston were struggling through their own perplexing symptoms.

Boston Sharp contracted COVID-19 in July 2020. Initially, he only experienced mild symptoms — a lost sense of taste and smell, along with some chills and aches.
At first, he thought he had it easy. But the formerly ace student began to struggle with subjects in school that wouldn’t have caused him to blink before. He was always tired and started losing weight for no apparent reason.
At first, he assumed his problems in school were just because of remote learning. He hated staring at the computer screen all day. But when the same symptoms followed him on his mission in Hagerstown, Maryland, he realized that something was seriously wrong.
The worst symptom was brain fog. “I knew where I was, and I knew what I wanted to do — say leaving the apartment. I knew I wanted to leave, but filling in the space to get there was impossible. My brain couldn't process it,” Boston said. “I just couldn't function. I couldn't figure out what I needed to do.”
He also struggled with word retrieval. He would find himself talking to people, and then, out of the blue, his brain would go completely empty. Almost as if there was nothing there in the first place.
Meanwhile, Madison signed up for a college summer course in chemistry — twelve weeks’ worth of material condensed into six weeks. She started the course confident in her abilities but soon realized she couldn't even read the textbook. She would experience short spurts of energy, followed by a crash and extended recovery periods leading to persistent headaches, more prolonged and more intense every day. Sometimes, migraines would force her out of action for days.
As a result, her exam marks were unusually low for this straight-A student. Madison tried to work harder, but it seemed like nothing was getting into her brain. She managed to pass the class, but not with the high marks she was used to. Her aspirations of becoming a doctor seemed virtually impossible to reach at this point.
Madison also noticed behavioral changes. She was spending her time with people she wouldn’t typically have been drawn to and made what she now sees as questionable decisions in her personal life. She felt overwhelmed regularly, riding an emotional rollercoaster. It led to breakdowns multiple times a week with hysterical crying, to the point that Sarah considered getting her psychiatric help and medication.
“Now, looking back, knowing that I had a brain injury, there was this impulse control that I didn't have anymore,” Madison reflected. “None of it made sense at the time; it was very much out of character for me,” she added.

At this stage, the Sharp family was at a loss about what to do. A trip to Guatemala in the summer for Sarah and Madison seemed to have helped a little — the exercise and practice speaking a foreign language did their brains some good — but Madison was still struggling when she went back to school. “I had days where I didn't want to get out of bed, and my grades were suffering. It was really rough,” Madison said.
When one of Sarah’s friends went to Cognitive FX for her case of Long COVID, she came out raving about the results. Sarah was a little skeptical at first; Cognitive FX is for patients with a brain injury. However, her COVID experience, combined with emerging medical research, led her to believe that the virus had affected her autonomic nervous system, which also happens in mild traumatic brain injuries.
In early October, Sarah decided to book a consultation for herself and Madison. From the moment they went in, they felt comfortable. “I had no idea what to expect, but the culture is incredible. It doesn't feel like you're a number. You feel like a human. We realized that we were surrounded by people who know how we feel,” Sarah said. “I broke down during the first group meeting. I was the last to introduce myself and struggled to speak. Tears streamed down my face with my ugly cry. I was not alone. All of these people knew exactly what I was going through.”
Sarah and Madison underwent a functional Neurocognitive Imaging scan (fNCI) as part of their assessment. This is a special type of MRI that can reveal which regions in the brain are either over or underactive, affecting normal brain function. Both Sarah’s and Madison’s scans showed many areas affected.
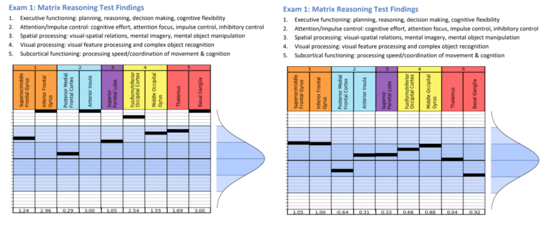 Madison’s scans showed hyperactivity in the Inferior Frontal Gyrus, Anterior Insula, Fusiform/Interior Occipital Cortex, and Basal Ganglia (left). Her scores in those regions were three standard deviations from the norm. All of those values returned to normal (within the blue region on the graph) on her second scan after treatment (right).
Madison’s scans showed hyperactivity in the Inferior Frontal Gyrus, Anterior Insula, Fusiform/Interior Occipital Cortex, and Basal Ganglia (left). Her scores in those regions were three standard deviations from the norm. All of those values returned to normal (within the blue region on the graph) on her second scan after treatment (right).
Despite her milder symptoms, Madison’s scan was worse than Sarah’s. “When I got my brain scan, I literally cried. I cried happy tears because there was something wrong with me. I wasn't just lazy and stupid. I had a brain injury. Even if they couldn't fix it, knowing that would have been enough,” Madison said.
With the results from the scan, the therapists were able to develop a treatment plan specifically designed to address the areas highlighted in Sarah and Madison’s scans, respectively. This treatment plan included a week of therapies such as vision therapy, occupational therapy, cognitive therapy, neuromuscular therapy, sensorimotor therapy, and psychotherapy completed during our week-long treatment.
This is a slightly modified version from the standard treatment offered to concussion patients, developed after they realized the impact on the brain is remarkably similar between patients with a mild traumatic injury and those with Long COVID.
The first day was challenging for Sarah, but after a good night's sleep, she awoke a different person. “I woke up, and I felt a mental clarity like I could see for the first time in 20 months. It's like getting glasses for the first time,” she said. “I could think clearly. I know it sounds weird to say that just after one day, but that's what it was. It turned my brain on.”
Cognitive FX’s treatment helped many of Sarah’s symptoms, including a dysfunctional diaphragm, which caused heartburn, a persistent cough, and difficulty breathing.
Madison found treatment equally difficult. “When I got called to do cognitive therapy, it was really hard. It felt like my brain was melting the entire time,” Madison explained. “But I was beyond excited. I could see the holes in my brain and the connections I was missing.”
Next in line for treatment was Boston. After seeing his mother’s and sister’s brain scans, he scheduled his consultation. A few days later, looking at his scan results, it was like a massive weight came off his shoulders. “At that moment, I knew I wasn't crazy, that there was actually something wrong with me. And even better, it could be fixed. I could get back to normal,” said Boston.
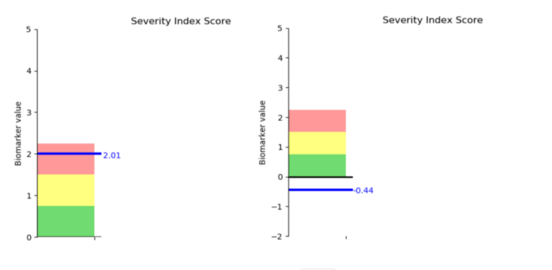 Boston’s initial scan results showed significant brain dysfunction. His scans after treatment were in the normal range (anything at or below zero).
Boston’s initial scan results showed significant brain dysfunction. His scans after treatment were in the normal range (anything at or below zero).
Therapy was demanding but rewarding. For Boston, the big issue was word retrieval. At one point during treatment, he was challenged to think of animals for each letter in the alphabet. Try as he might, he simply couldn’t think of one that started with the letter T. He returned home every night feeling exhausted but hopeful he would feel the effects soon.
Finally, on the last day of treatment, he felt the progress. Talking to friends, he noticed that he could remember books he read, even the characters’ names, which he hadn’t been able to do for some time.
“I was really happy because I felt like me again,” he shared. “This is super cliché, but I felt like me. And it was the greatest feeling that I was back.”

It’s still only a couple of months after their treatment, but all three members of the Sharp family have noticed significant improvements after their week at Cognitive FX. “This treatment has been life changing! I feel the most normal in 20 months; I feel very much more like myself,” Sarah said. She’s still dealing with some lingering symptoms but is focused on building strength and eating healthier.
Likewise, Madison feels like she’s getting her brain back. Her headaches are still noticeable, and she feels overstimulated sometimes, but nothing like before treatment. “Before COVID, I was able to focus on things, and I was able to really dive into things I was passionate about. I lost that with COVID, but now I have it back,” Madison said.
Both Sarah and Boston have noticed the positive impact on Madison. “Madison is my daughter again. I see her as 100% herself,” Sarah agreed.
Boston’s brain fog still makes an appearance occasionally, but not nearly as much as before. He continues to do his homework from the Cognitive FX therapists and feels optimistic about the future. “At this point, it's only been a month. I'm pretty optimistic that in the coming months that I'll continue to get better. I'm feeling good about it,” he said.
Overall, the members of the Sharp family who have undergone treatment at Cognitive FX all feel very positive about it. “Cognitive FX is voodoo or magic,” joked Sarah. “Or maybe it's just really good science.”
“I feel the way they do medicine is the way medicine should be done,” Madison added. “Especially with brain injuries, the care is better when it's patient-centric and collaborative.”
Sarah firmly believes Madison and Boston would be on a different trajectory in their lives if they hadn’t been treated. “I'm not leaving it to chance with my other children,” who are also showing signs of Long COVID, she concluded. They’re likely to visit Cognitive FX as well in the coming months.
Note: Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.

Alex Reis is a freelance writer who loves to write about science and technology.
A growing body of scientific evidence suggests some COVID-19 patients will experience neurological signs or symptoms of the infection. Genetic material from SARS-CoV-2, the virus that causes...

Most people who get infected with the coronavirus recover within a few weeks. However, some continue to experience symptoms weeks or even months after they are infected. They have what are known as ...