Even after you've recovered from the acute symptoms of COVID-19, you might find yourself struggling with short-term memory loss, concentration issues, and other cognitive symptoms. If it's been weeks (or even months) since you had COVID-19, it can feel like there is no reason why you should still feel this way. These lingering symptoms after initial recovery from COVID-19 have become known as “long COVID” and can have a debilitating effect on your life.
How long COVID affects the brain is becoming increasingly clearer. Evidence gathered by research teams across the world suggests that the coronavirus can have multiple effects, including disrupting healthy blood flow to the brain and triggering inflammatory responses throughout the body that eventually cause neuroinflammation.
As we followed the emerging research, we noticed that the effects of COVID-19 on the brain are remarkably similar to what happens in concussion (mild TBI) patients whose symptoms persist beyond the expected recovery window. Long COVID patients didn't get a brain injury from hitting their heads, but they did get one from a viral illness. The overlap in symptoms is more than just a coincidence.
We could see this clearly with a patient who received treatment for a brain injury and then came back a few months later for a second treatment when she developed symptoms of long COVID. The patient’s symptoms and brain scans showed similar dysfunction before treatment, and she responded well to both treatment for the mTBI and for long COVID.
Since then, we’ve treated dozens of long COVID patients who made significant strides in recovery during their time at our clinic. A whole year of treating COVID patients has helped us understand how their brains, nervous system, vision, and even vestibular systems can be affected by the virus.
This article will explain how long COVID affects the brain and nervous system, the treatment approach we use, and which types of COVID “long-haulers” can benefit from this type of treatment.
Here’s a quick summary of what we'll cover:
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, over 90% of our patients experience significant symptom improvement. Thus far, we’ve seen similar results with long COVID patients who pass our screening criteria. To discuss your specific symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Who Are We, and What Qualifies Us to Treat Long COVID?
Before we dive into the explanations of what causes long-haul COVID in most patients and how we approach remedying those problems, here’s a quick explanation of what we did before the pandemic hit and why it gave us the needed expertise to treat long COVID patients.
At Cognitive FX, we use state-of-the-art brain imaging techniques and the world’s largest multidisciplinary team focused on patients suffering from persistent post-concussion symptoms. Our team includes clinical neuropsychologists, neuroscientists, a neuroradiologist, a neurosurgeon, psychologists, cognitive therapists, occupational therapists, physical therapists, a neurointegration specialist, MRI technicians, and more. We actively engage in and publish research on brain injury rehabilitation.
We treat hundreds of patients every year at our clinic in Provo, Utah. They come from not just across the U.S., but also from Canada, Europe, and other parts of the world.
Because the effect of certain other conditions on the brain is similar to that of concussion, we’re often able to treat patients who suffered transient ischemic attack, carbon monoxide poisoning, encephalitis from infectious diseases, and more. What they all have in common is that their injury affected neurovascular coupling (NVC) in the brain (something we explain below), autonomic nervous system function, and more.
As it turns out, post-COVID syndrome results in these issues as well. While there are post-COVID conditions we can’t treat, our patients go through a screening process for these complications before we accept them to our clinic. We only treat patients we believe we can help. Sometimes, this means that patients see other treatment providers first, and then visit our clinic when they’re ready.
Want to hear from the patients themselves? View patient stories here.
What Is Long COVID?

Most people who catch COVID-19 only have a mild illness or are even completely asymptomatic. When any symptoms develop at all, they usually disappear within a couple of weeks.
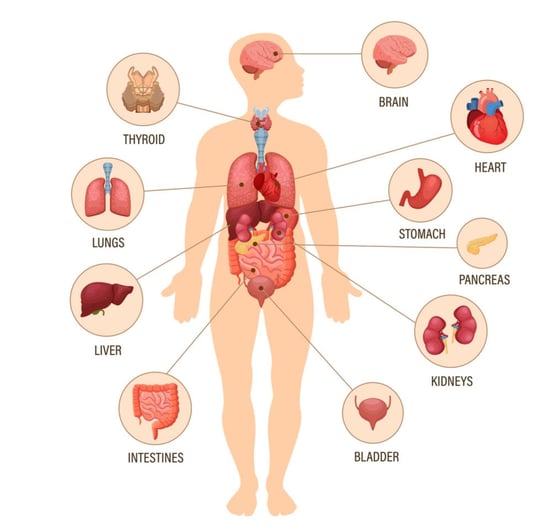
However, for a significant proportion of those infected with the virus (even in mild cases), COVID-19 becomes a long-term condition with a wide range of symptoms affecting just about every organ in the body. This has become known by several names, including post-acute sequelae of SARS-CoV-2 infection or post COVID syndrome. More commonly, people call it Long COVID, and those living with this condition are known as “COVID long-haulers.”
At first, doctors believed these cases had a purely psychosomatic cause, most likely due to the stress and anxiety caused by the pandemic. Others blamed it on post-traumatic stress disorder in patients who received life-saving interventions in intensive care units (ICUs). However, the sheer number of cases of patients suffering from long COVID is too high to be explained solely by psychosomatic factors, ICU experiences, or unrelated medical conditions.
There is ample evidence that COVID can cause long-lasting effects: you aren’t imagining your symptoms. For patients who needed hospitalization, an Italian study showed that 87% still had symptoms two months after release, and a British study found similar results. However, long COVID can happen to anyone: A German studyfound that 78% of patients who recovered at home still had heart problems after about three months.
In the United States, the Centers for Disease Control and Prevention (CDC) found that at least a third of non-hospitalized patients were still struggling to return to full health after a few weeks.
Because it’s such a new phenomenon, many doctors don't know how to diagnose these patients. To further complicate matters, not every patient experiences the same symptoms, and some signs appear intermittently and in different parts of the body. This makes it very hard for doctors to identify what’s wrong and decide how to treat it.
Long COVID Can Affect Multiple Parts of the Body
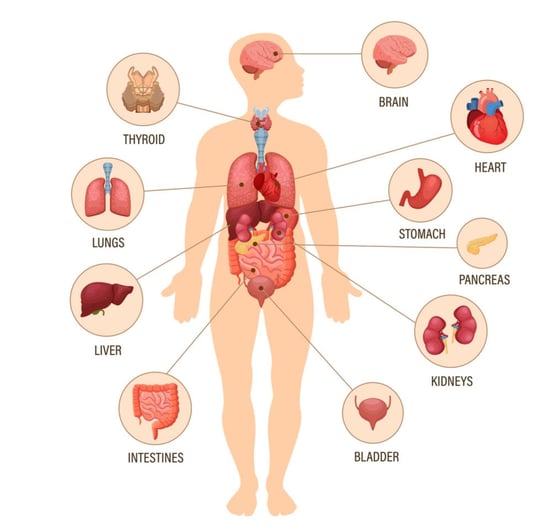
The most common symptoms associated with Long COVID are fairly non-specific and include headaches, fatigue, breathlessness, and joint pain. However, patients can experience a wide range of symptoms with some surveys identifying more than 50 different symptoms affecting every organ in the body.
Here are a few of the major systems affected by Long COVID:
- Respiratory system: COVID-19 is primarily considered a respiratory condition. In COVID-19 survivors, the virus may cause a wide range of long-term respiratory problems, from shortness of breath (dyspnea) to acute respiratory distress syndrome (ARDS) and pulmonary fibrosis. A small proportion of patients may even need supplemental oxygen due to persistent hypoxemia (below normal oxygen levels in the blood). Experts say it may take months or even years for lung function to return to normal in these patients.
- Cardiovascular system: Studies have shown that heart problems are also common, including impaired pumping function of the heart, inflammation of the heart muscle, or the presence of scarring. Such heart damage could explain long-term symptoms such as shortness of breath, sharp and persistent chest pain, heart palpitations, and exercise intolerance. This inflammation appeared even in people with a mild case of COVID-19 and no medical issues before they got sick.
- Nervous system: A U.K. study looking at over 200,000 patients diagnosed with COVID-19, determined that at least one in three survivors suffered from neurological or psychiatric problems six months after the initial COVID-19 infection. The symptoms were observed in all age groups, both in patients who isolated at home and in those admitted to hospital. Plus, research has now linked mild COVID infections to brain damage in elderly patients.
- Digestive system: Many patients with Long COVID experience digestive issues and stomach cramps. For example, 44% of patients still had lingering gastrointestinal symptoms after three months, including loss of appetite, nausea, acid reflux, vomiting, abdominal discomfort, and diarrhea.
- Other organs: The list includes many other symptoms, from hair loss and sleeping problems to formation of blood clots and chronic kidney disease. It is also likely that the list is not complete yet and more symptoms will come to light. Further research is needed to explore the full impact caused by Long COVID.
Symptoms of Long COVID

One study reported over 200 symptoms that can fluctuate or even appear out of the blue after patients have recovered. We’ve covered a few of the most common ones in other blog posts:
Some other COVID-19 symptoms that can linger for weeks, months, or years include…
- Loss of sense of taste or smell
- Difficulty concentrating
- Muscle ache
- Cough
- High temperature
- Sore throat
- Joint pain
- Chest pain or tightness
- Heart palpitations
- Dizziness
- Malaise
- Pins and needles
- Tinnitus or earache
- Nausea
- Diarrhea
- Abdominal pain
- Loss of appetite
- Skin rashes
- Depression and anxiety
- Problems sleeping
- Changes in the menstrual cycle
What Causes Long COVID
As soon as the first patients started reporting cognitive and neurological long-term effects last year, scientists started wondering why this was happening.
Although the exact mechanism and risk factors are not yet fully understood, researchers believe long COVID-19 triggers inflammatory responses throughout the body, which leads to neuroinflammation in the brain. There is also some evidence that COVID-19 restricts blood flow to the brain, most likely resulting from a general state of hypoxia in the body caused by breathing problems and dyspnea.
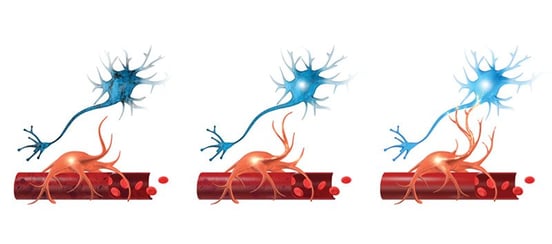
In the brain, these mechanisms are known to interfere with the supply of oxygen to the areas that need it to perform a particular function. This connection between brain cells and the blood vessels that supply them with energy and oxygen is called neurovascular coupling (NVC). In a healthy brain, NVC is how the vascular system delivers the right amount of blood at the right time for neurons to complete the tasks required of them.
In long COVID patients, however, the normal supply of energy to the brain via neurovascular coupling is disrupted. This is known as neurovascular coupling dysfunction, and we believe it’s one of the main causes of lingering symptoms in the brain after the virus is gone. We’ve clear indicators of NVC dysfunction in dozens of long-haul COVID patients who have come to our clinic for help.
But there are other dynamics in play than just NVC dysfunction. Like mTBI patients, COVID long-haulers also experience symptoms that stem from…
- Autonomic nervous system dysfunction
- Vision dysfunction
- Vestibular dysfunction
- Breathing dysregulation
We’ve written more extensively about those issues in our post on how COVID affects the nervous system. In short, Long COVID affects the brain and body in much the same way as a mild traumatic injury.
How We Diagnose and Treat COVID Long-Haulers at Cognitive FX

At our clinic, we’ve treated hundreds of patients who suffer from long-term symptoms from a brain injury. While the majority of our patients come to us after suffering a mild, moderate, or severe traumatic brain injury, we’ve also treated many other patients with non-traumatic acquired brain injuries.
Non-traumatic acquired brain injuries can be the result of a viral infection, oxygen deprivation, metabolic disorders, aneurysms, cardiac arrest, and near-drowning experiences, to name just a few. In short, it refers to all brain injuries that are not the result of an external physical force applied to the brain but which still cause severe symptoms.
These may seem totally unrelated, but they’re all very similar in their effect on the brain. All of them can result in neurovascular coupling (NVC) dysfunction.
The same is true for long COVID. The long list of symptoms described by COVID long-haulers are strikingly similar to complaints from patients with a mild traumatic brain injury. This resemblance inspired us to assess whether we could offer a treatment for those suffering with long COVID. So far, we are seeing promising results with the patients who underwent non-pharmacological treatment for long COVID at Cognitive FX. Continue reading to see some of our results.
Diagnosis: Knowing How COVID Changed Your Brain
Long COVID patients receive an assessment and treatment plan similar to those our concussion patients receive.
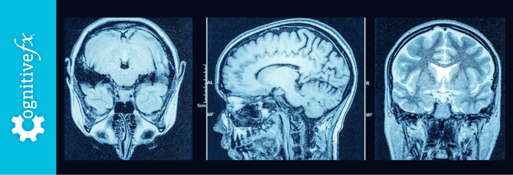
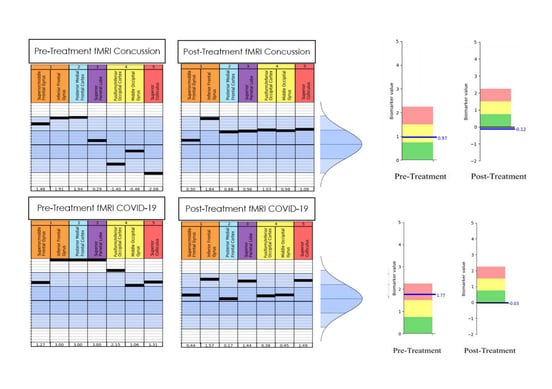
Before we can decide on the best course of action, we need to assess how their brain is affected. At our clinic, the main way we detect neurovascular coupling dysfunction is with functional Neurocognitive Imaging (fNCI), which is a special type of functional MRI. During the fNCI, each patient goes through a series of cognitive activities while we take images of their brain.
The scan produces over 7000 near-real-time images across 56 regions of the brain, which are then compared to a healthy control database to assess where NVC dysfunction is occurring and to what severity in different regions of the brain. The scan highlights areas that are operating normally and areas that are not activating as expected.
.jpg?width=552&height=303&name=How%20We%20Found%20a%20Viable%20Treatment%20for%20COVID-19%20Long-Haulers%20(4).jpg)
.jpg?width=552&height=382&name=How%20We%20Found%20a%20Viable%20Treatment%20for%20COVID-19%20Long-Haulers%20(6).jpg)
Total scores in the yellow, orange, or red indicate neurovascular coupling dysfunction. We also assess communication between regions of the brain. In the region-by-region report, dark blue indicates less activity than we would expect, revealing underperforming connections in the brain.
The scans for our COVID long-haulers showed the same kind of dysfunction as we see in patients suffering from post-concussion syndrome. Just like in our post-concussion patients, every scan was different, affecting different areas in the brain for each COVID long-hauler. We found some patients with such extreme deviations from normal that there was effectively no activation in that brain region as observed on the fNCI.
Further Diagnostic Assessment
Alongside the fNCI scan, all our patients undergo a detailed interview before treatment starts to assess previous history of health problems, track progression of symptoms, assess current physical and neurocognitive performance, and inform them of what to expect from our treatment.
Although the general procedures are the same, this initial assessment is slightly adjusted for COVID patients, allowing our therapists to focus on some points which may be more important for these patients. For example, we look particularly at loss of smell and taste, which is a common symptom for COVID patients but unusual for concussion patients. We also focus on cardiovascular and respiratory systems, which, as explained earlier, are organs commonly affected by Long COVID.
With this background information and the results from the scan, our therapists can then tailor a therapy schedule to target specific areas of the brain that were most impacted by the effects of COVID-19.
What Treatment Involves

The good news is that, in many cases, long COVID symptoms are treatable if you know where to turn for help. As the brain dysfunction caused by the virus seems identical to that of concussion patients, we’ve applied the same therapy that we use routinely for our concussion patients and obtained promising results.
A condition as complex and wide-ranging as long COVID is not going to be cured with a single treatment or medication. This is why our approach — which we call Enhanced Performance in Cognition (EPIC) Treatment — includes various multidisciplinary therapies, including vision therapy, occupational therapy, cognitive therapy, neuromuscular therapy, sensorimotor therapy, psychotherapy, and more.
.jpg?width=1999&height=1333&name=Why%20Most%20Post-Trauma%20Vision%20Syndrome%20Treatment%20Falls%20Short%20(4).jpg)
During each day of personalized treatment, patients see different therapists for their prescribed routine. For example, a patient may start with cardio to prepare their brain and then do occupational and vision therapy. After that, they might have a quick break before starting again with cognitive therapy. After lunch, they may engage in neuromuscular therapy, then psychotherapy, and then complete the day with sensorimotor therapy.
%20(5).jpg?width=1999&height=1333&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(5).jpg)
Every therapist knows how hard to push each patient and can adapt to the patient's needs. For example, it’s common for COVID long-haulers to struggle with cardio, but our therapists are prepared to offer them various exercises to help break the dominance of the sympathetic nervous system and restore balance in the autonomic nervous system. The trick is to slowly recondition a patient’s nervous system through careful exercises, without triggering a debilitating crash. You can read more about this process here.
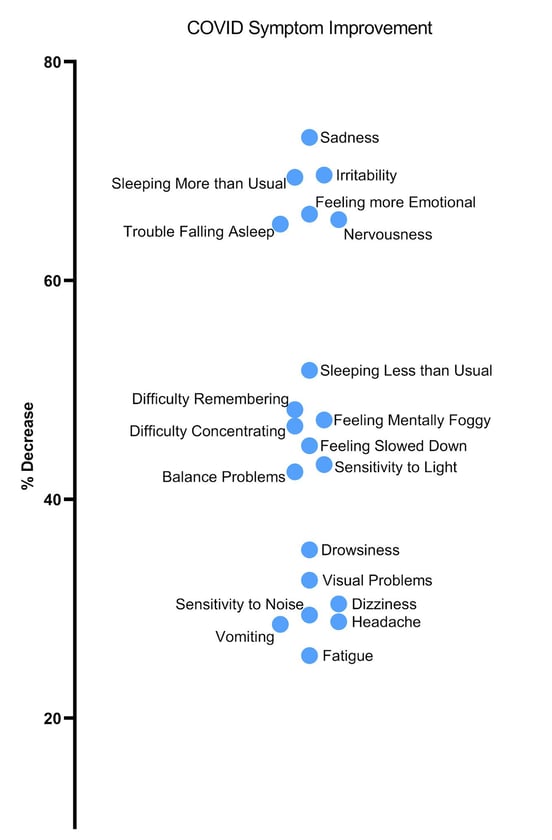
Finally, on the last day, we administer a follow-up fNCI to see how much each area has improved. By the end of treatment, patients improve by an average of 60% on their symptom severity. The exact percentage each symptom decreases varies, but we’ve seen some clustering in symptom improvement (data based on 43 patients polled).
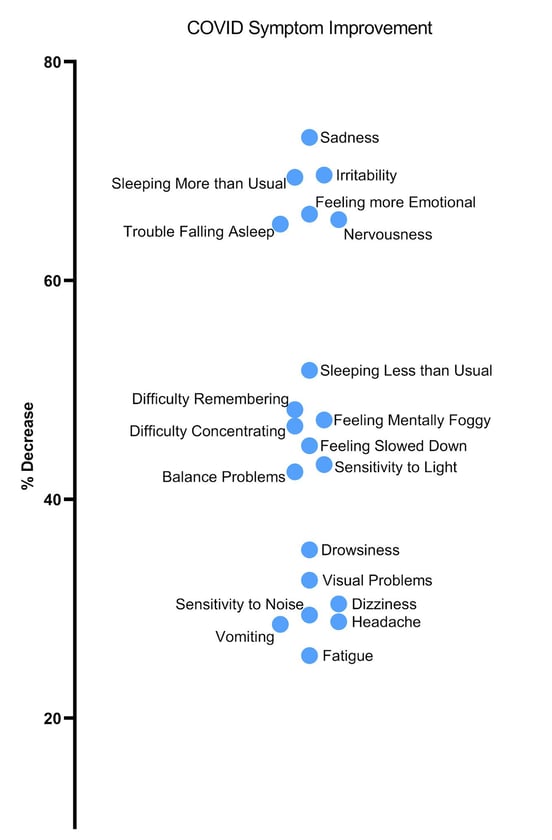
We often see that fatigue and headache symptoms improve as patients go home to rest after a very intense treatment period. Visual problems typically take sustained vision therapy (three to six months on average) for full improvement.
We encourage patients to continue their treatment regimen at home (all patients receive an EXIT packet with instructions for further care) and to join our patient support group (invitations are sent upon treatment completion).
To learn if you are eligible for treatment at our clinic, schedule a consultation with our team.
Data from Our Patients
As mentioned earlier, much of our work with COVID long-haulers began with a patient we treated for a brain injury back in March 2019. Some of the symptoms this patient was experiencing at the time included balance problems, exercise intolerance, brain fog, fatigue, headaches, irritability, memory problems, mood disruption, and sleep disruption, as well as mental health symptoms of anxiety, depression, and PTSD. After a week, her symptoms had reduced by 30%, and she continued to improve further afterwards.
However, in December 2020, she contracted COVID-19 and three months later decided to return for a second treatment at Cognitive FX. Many of the lingering effects she was now experiencing due to Long COVID were the same as before, including anxiety, irritability, cognitive fatigue, depression, headaches, lack of concentration, mood disruption, nervousness, sleep disruption, heart rate problems, and exercise intolerance. Her second week ended with a 45% improvement and put her back on her journey to recovery.
What we found remarkable with this patient is that, despite affecting different regions in the brain, the results from both fNCI scans clearly show disruption in neurovascular coupling, both with a concussion and long COVID. This data confirmed our suspicions that long COVID and traumatic brain injuries affect the brain in a similar manner and respond equally well to our EPIC treatment.
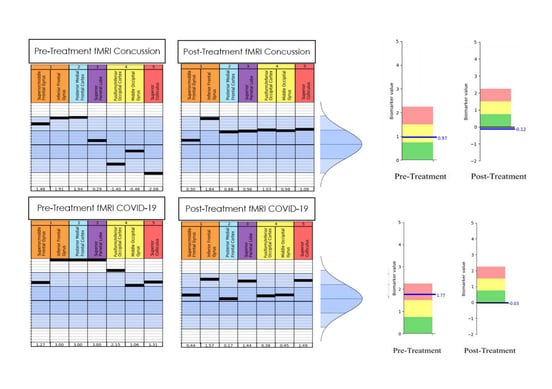
Note that this report is from our first-generation fNCI. We’re migrating the clinic to second-generation scans and reporting, which you saw earlier in this post.
For this patient’s initial scan for her concussion (the top left table), several areas involved in attention, focus, organization, and planning were hyperactive (as indicated by the black bars which are above the dark blue section in the middle, which is the “healthy zone”). Other brain areas involved in visual tracking and processing (yellow and red columns) were hypoactive (as indicated by the bars below the dark blue “healthy zone”). In addition, many black bars aren’t very close to one another, indicating these brain areas aren’t sharing the load of visual tasks equally. These results, in addition to results from the 5 other tasks, made her severity index score (SIS) a 0.97.
After her initial week of treatment, these areas were much more stable and connected, meaning her brain was functioning much more efficiently (which you can see in the top right table) and her SIS was an amazing -0.12.
For the patient’s initial scan for her long COVID, everything on this same task was hyperactive, as can be seen in the bottom left table. In fact, some areas were now so hyperactive their black bars were at the very top — meaning the scan couldn’t measure anything higher. Plus, large gaps were present between many bars, and her SIS was a 1.77 — significantly above her concussion SIS. Treatment proved effective again and her score improved to a -0.03; however, the patient was sent home with specific exercises to keep improving the lingering hyperactivity and gaps seen in several areas in the bottom right table.
Want to read about a whole family who recovered from long COVID? Here’s how the Sharp family recovered from long COVID.
Frequently Asked Questions
Can Children Suffer From Long COVID?
Initially, researchers believed that COVID-19 was contracted only rarely by children. As the virus has changed with time, more and more children are experiencing post-acute COVID-19 symptoms. But they don’t always look the same as adult’s symptoms.
Read more about long COVID symptoms in children and how to get them treatment.
If your child started developing symptoms after a case of COVID-19, even if it was mild, our best advice is to visit a healthcare provider. Make sure you inform their primary care provider that your son or daughter had COVID, so they can watch for signs of long COVID.
What Patients May Not Be Eligible for Treatment at Cognitive FX?
EPIC treatment is not suitable for every patient. Those with severe gastrointestinal issues, such as losing weight or poor appetite, are advised to consult with a gastroenterologist to solve those issues first, before attempting to treat their brain condition. Unfortunately, some health conditions — in particular, drastic, uncontrolled, and continuing weight loss — interfere with the effectiveness of our treatment program.
What Does Long COVID Mean for Patients with a Pre-existing Brain Injury?
As neurovascular coupling dysfunction is one of the main factors in traumatic brain injuries, it should not come as a surprise that post-concussion patients are more likely to suffer from cognitive and neurological symptoms if they get infected with COVID-19.
Many of these patients may already have problems with vasculature regulation and their breathing patterns may be affected as well. As a result, they are more likely to experience difficulty breathing and suffer an immune system overload.
If you’re still recovering from a brain injury, we advise you to follow social distancing rules, wear a mask, and talk to your doctor about getting the COVID-19 vaccine, if you can. Take all the steps you can to minimize your chances of catching COVID-19, as your risk of developing long-term symptoms is high.
Long COVID Is an Acquired Brain Injury

After our success treating some patients with lingering symptoms after contracting COVID-19, we believe the impact of long COVID on the brain should be considered an acquired brain injury and treated accordingly. It has the hallmark signs of neurovascular coupling dysfunction that we can identify in our patients with traumatic brain injuries.
Despite positive results treating patients with long COVID, it’s reasonable to exercise some caution predicting how much and how fast these patients can recover. We have seen reasonably quick recoveries in some symptoms, such as loss of smell and taste, but more severe complications, such as depression and anxiety, may take longer to subside.
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.




.jpg?width=552&height=303&name=How%20We%20Found%20a%20Viable%20Treatment%20for%20COVID-19%20Long-Haulers%20(4).jpg)
.jpg?width=552&height=382&name=How%20We%20Found%20a%20Viable%20Treatment%20for%20COVID-19%20Long-Haulers%20(6).jpg)

.jpg?width=1999&height=1333&name=Why%20Most%20Post-Trauma%20Vision%20Syndrome%20Treatment%20Falls%20Short%20(4).jpg)
%20(5).jpg?width=1999&height=1333&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(5).jpg)








.png?height=175&name=Physical%20therapy%20covid%20(2).png)