Yes, Long COVID Can Cause POTS and Dysautonomia
Your heart races when you stand. You hate the dizzy spells. Your head hurts, you’re exhausted, and you can’t think clearly like you used to.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
COVID-19 can affect the autonomic and central nervous systems. It can affect organ systems directly through infection or indirectly via dysfunction in the nervous system. That means a host of crazy-sounding symptoms — such as blood pressure changes, memory and attention issues, and gastrointestinal upset — are possible during and after COVID. But many of the lingering, post-COVID symptoms are related to nervous system dysfunction.
Up to two-thirds of long COVID patients endure some type of autonomic nervous system dysfunction. For example, one study found that 13% of long COVID patients experienced orthostatic hypotension, a condition that can result in dizziness and fainting due to a decrease in blood pressure upon standing.
Further reading: Long COVID causes POTS (and what you can do about it)
The ideal treatment program for autonomic nervous system issues (dysautonomia) requires multidisciplinary, integrated care, according to the American Autonomic Society. Many researchers and patients are concerned because that care is difficult to find. If you visit a neurologist, for example, they might offer medication for headaches but be unable to help with post-COVID digestion woes. (For those interested, we’ll discuss how our treatment program provides multidisciplinary, integrated care later in this post.)
In addition, recent research has shown that mild COVID can cause brain damage (study only performed in older populations). As a result, patients need to find care providers who can not only address nervous system dysfunction but who can provide rehabilitation for the brain as well.
Therefore, while this article will review how COVID affects the nervous system (based on the most current research), we will also explore…
Our treatment was originally designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, over 90% of our patients show improvement. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
In most cases, the SARS-CoV-2 virus does not appear to harm the central nervous system (CNS) through direct infection of neural tissue. While scientists previously thought the virus might gain access through ACE2receptors in the olfactory nerves, studies of cerebrospinal fluid from the spinal cord did not reveal the viral RNA from a SARS-CoV-2 infection. In addition, extreme presentations of the disease, such as encephalitis (swollen brain tissue), seem present in only a handful of extreme cases.
Instead, it may be the body’s response to the virus (and even the lifestyle changes that can come with illness) that causes nervous system dysfunction in most patients.
Most patients will notice symptoms that stem from problems with the autonomic nervous system (ANS). Via peripheral nerves, the ANS manages automatic, bodily functions that we don't need to think about, such as blood pressure, speed of digestion, breathing rate, heart rate, body temperature, kidney and bladder function, sexual function, and many others.
%20(7)-1.jpg?width=552&height=515&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(7)-1.jpg)
The two main parts of the ANS that can be affected after COVID-19 infection are the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). Think of the SNS as the “fight or flight” response. Given the right environmental stimuli, it might increase your heart rate, stimulate blood flow to your muscles, and increase muscle tension.
In contrast, the PNS is your “rest and digest” background system. It counterbalances the SNS — lowering heart rate, regulating digestion and bladder function, slowing your breathing rate, and so forth.
Typically, the PNS and SNS are constantly switching control back and forth throughout your body to meet the needs of each moment. You might notice your heart rate spike (SNS) if your friend says, “We need to talk,” and then relax when you learn it’s not a serious issue (PNS).
But after COVID, that interchange between branches of the PNS and SNS may be dysfunctional. You might be stuck with only one dominant branch (in most patients, the SNS is dominant over the PNS). You might also experience problems with brain function, vision, or vestibular function (orientation in space).
So what causes nervous system malfunction after COVID? While research is ongoing, there are at least five common culprits contributing to symptoms: the body’s immune response to COVID-19, damage to endothelial tissue, neurovascular coupling dysfunction, breathing changes, and lifestyle changes.
Whenever SARS-CoV-2 — the virus behind the COVID-19 pandemic — enters a part of your body, the body responds by sending a platoon of immune cells to attack the virus. Localized inflammation is a normal and healthy response to a viral infection; it’s part of what the body needs to do to survive infectious diseases.
But in some COVID-19 patients, the immune response goes too far. It triggers a hyperinflammation response throughout the body (causing systemic inflammation instead of localized inflammation).
Many researchers have focused their efforts on cytokines: chemicals released during excessive immune reactions in COVID patients. Elevated cytokine levels have been detected in long COVID patients who are experiencing a variety of symptoms. For example, one study showed that patients with high levels of cytokines (not necessarily cytokine storms) are more likely to experience headaches as compared to patients with low levels of cytokines. Since cytokines are known to impact working memory and attention, they’re clear suspects for post-COVID cognitive impairment.
Since the immune system and the autonomic nervous system work together closely, major changes in one can affect the other. High cytokine levels are likely triggers for autonomic dysfunction, which could then perpetuate inflammation throughout the body while causing many post-COVID symptoms.
Researchers are also noticing a rise in autoimmune disorders after COVID-19 infection. Some patients are developing antibodies to their own cells instead of just to the coronavirus disease, which in turn is leading to new allergies and rheumatic conditions such as arthritis. (Note that you can have these immune issues without having developed an autoimmune disease).
The coronavirus can, via direct entry to the cells or through inflammation, damage the endothelium (the lining of the blood vessels). This has several consequences.
First, the ANS communicates closely with the vascular system (blood vessels). If some part of the vascular system malfunctions, it could cause instructions from the ANS to be carried out incorrectly. Alternatively, the ANS might receive incorrect feedback from the vascular system. The result of this or any other malfunctions could be autonomic dysfunction.
Second, the endothelium is a key part of the neurovascular unit, which is composed of vascular cells, glial cells, and neurons. The vascular system brings important resources (oxygenated blood, etc.) to brain cells. If the endothelium is damaged by COVID-19 or neuroinflammation, then the vascular system in that area will not function as well as it should, which in turn means those neurons will likely not function as well as they should.
%20(5)-1.jpg?width=552&height=326&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(5)-1.jpg) Image source: Nelson et al (2016).
Image source: Nelson et al (2016).
These post-COVID changes could result in many common symptoms, such as headaches, blood pressure problems, exercise intolerance, and more. Some researchers are also investigating whether the inflammation and vascular damage from COVID-19 infection put patients at increased risk for Alzheimer’s, vascular dementia, or other neurological disorders.
The cerebrovascular network responds dynamically to the needs of neurons (a relationship known as neurovascular coupling, or NVC). As clusters of nerve cells activate to perform a task, they summon just the right amount of blood at just the right times. Damage to the endothelial cells or other post-COVID complications could disrupt that delicate communication cycle.
NVC dysfunction can cause many cognitive and physical symptoms after COVID-19, such as sleep problems, feelings of overwhelm, memory issues, vision problems, and more. It’s also closely linked with autonomic nervous system dysfunction. We treat both ANS dysfunction and NVC dysfunction at our clinic.
Further reading: How we found a viable treatment for COVID-19 Long-Haulers
%20(4).jpg?width=552&height=303&name=s%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(4).jpg)
Least surprising on this list is that the effects of COVID-19 extend to post-infection breathing issues. Inflammation in the lungs can result in lower oxygenation throughout the brain and body. A severe COVID-19 infection can even inhibit lung function so much that the patient suffers from hypoxia (too little oxygen throughout the body). Severe infections are unique because they can cause scarring, may require intubation, or result in other complications that then cause breathing issues in addition to ANS dysregulation.
But even just the experience of altered breathing during a mild COVID infection can cause problems. Why? It takes roughly 100,000 repetitions to make a new motor pattern. Because we breathe around 25,000 times per day, just four days of altered breathing during COVID could cause lingering issues, such as breaths that are too shallow and rapid. Such breathing patterns leave stale air in the lungs (not great for healing) and raise blood oxygen levels relative to carbon dioxide. But we need that carbon dioxide for our cells to use oxygen, so the excess oxygen from rapid breathing goes unused.
Dysfunctional breathing could take the form of hyperventilation, periodic deep sighing, irregular breathing patterns, breathing from primarily the upper chest, and forced abdominal respirations. Common symptoms of dysfunctional breathing are dyspnea, tachycardia, impaired physical stamina, and sighing while feeling starved of air.
Altered breathing dynamics can activate the sympathetic nervous system, pushing it into dominance over the parasympathetic nervous system. Unfortunately, many patients experience a cycle in which altered breathing dynamics make their ANS dysfunction worse, and the ANS dysfunction perpetuates the breathing problems they experience.
Further reading: Breathing problems after COVID-19
The nervous system responds to your environment. Changes in your stress level, diet, and exercise regimen could all contribute to ongoing symptoms.
If you’ve been stressed for a while (say, while you’re recovering from a COVID-19 infection), that sustained stress can trigger some amount of ANS dysfunction. Even purely psychological stress can negatively impact ANS function. There is even an association between ANS dysfunction, elevated inflammation levels, and depression. Many patients find themselves caught in a cycle of emotional and autonomic dysregulation that requires therapy to resolve.
Exercise levels can also impact the nervous system. Exercise levels help to prevent and treat autonomic disorders, but COVID-19 can make it difficult to exercise. Learning how to exercise without exacerbating symptoms is key to recovery.
Finally, neurological health and diet are linked. Many patients slipped into unhealthy eating habits during the pandemic. Emphasizing a diet rich in fruit, vegetables, omega-3s, and other brain-friendly foods while de-emphasizing saturated fats, sugars, and simple carbohydrates can help.
%20(4).jpg?width=1000&height=445&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(4).jpg)
Because of the way that long COVID can affect the brain and nervous system, patients may experience a wide range of neurological manifestations throughout the body. Many of our patients have asked questions like, “Is this normal?” or “Can COVID cause this?” And the answer, oftentimes, is, ”Yes” — especially when they are suffering from some combination of vascular issues, breathing changes, ANS dysfunction, neurovascular coupling dysfunction, vision issues, and vestibular problems. In other words, long COVID can affect the entire body, from the brain all through the peripheral nervous system.
Patients may also develop secondary conditions (called sequelae), such as high blood pressure, that can also contribute to symptom burden.
Below is a list of possible neurological complications from long COVID (gathered from multiple sources such as this article and this one, along with our own studies of patients). Symptoms of COVID that are hyperlinked lead to blog posts examining the symptom in greater detail.
Some of these symptoms may worsen situationally. For example, some patients may start to feel faint while standing for a long time. Or your cognitive difficulties may worsen after using a computer for a few hours. Many of these symptoms worsen after extended physical or cognitive exertion.

At Cognitive FX, we offer treatment protocols to assist with post-COVID brain challenges (neurovascular coupling dysfunction), autonomic dysfunction, vision issues, and vestibular problems. Because treatment often results in better sleep, symptoms stemming from poor sleep quality often improve as well.
At our clinic, we primarily treat post-concussion syndrome (PCS) patients. These patients suffer from lingering mild traumatic brain injury symptoms that won’t go away without treatment. Shortly after long COVID was observed, we realized that long COVID symptoms strongly overlapped with our concussion patients’ experiences.
So, we did what any good neuroscience practitioner would do: We started scanning long COVID patients’ brains. The results confirmed that long COVID patients were indeed suffering from a similar type of brain dysfunction — one that we could treat at our clinic. We’ve since confirmed that many long COVID patients respond well to our treatment approach, though some symptoms improve immediately, while others respond better to continued efforts after the treatment intensive.
%20(6)-1.jpg?width=552&height=840&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(6)-1.jpg) Average percent decrease in symptom severity across 43 patients. As we collect results from more patients these numbers may change.
Average percent decrease in symptom severity across 43 patients. As we collect results from more patients these numbers may change.
You can read more about our research process here.
When you come to our clinic for treatment, one of the first things you’ll do is get a functional Neurocognitive Imaging (fNCI) scan. fNCI is a type of functional MRI that looks at blood flow dynamics throughout 56 regions of the brain while the patient performs a series of standardized cognitive tasks. Our protocol also allows us to look at connections between those brain regions.
We’re then able to infer the health of brain regions involved in specific tasks, such as visual-spatial mapping, name retrieval, multitasking, and reading comprehension. Here’s an example from a patient with neurovascular dysfunction:
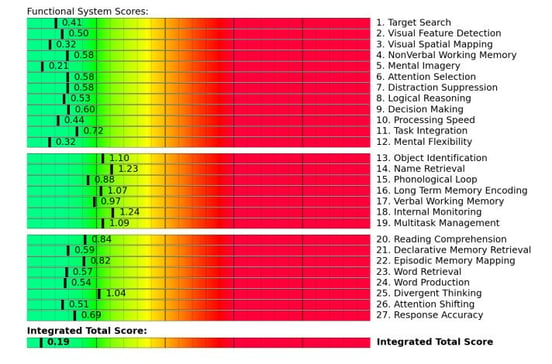
If you score in the yellow zone or beyond, then the brain regions responsible for that score become our priority during your treatment program because they’re the ones in most need of rehabilitation.
We also consider how well your brain regions are communicating with each other.
%20(3)-1.jpg?width=552&height=256&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(3)-1.jpg)
For example, the scan above shows unexpectedly low activity in the right anterior cingulate cortex (rACC, in blue). rACC plays a key part in sustained attention and is involved in other types of attention as well. As a result of this information, our therapist team could adapt their regimen to include sustained attention therapy exercises for this patient.
In addition to the brain scan, you’ll undergo testing for vision and vestibular function, along with a handful of cognitive and physical capabilities. The rest of treatment is a tailored therapy regimen designed to address your specific needs.
%20(6).jpg?width=1999&height=1333&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(6).jpg)
Treatment involves a unique combination of therapies and other strategies to promote recovery from long COVID. All patients cycle repeatedly through three stages: Prepare, Activate, and Recover. These stages prepare the brain for therapy, immerse the brain and body in carefully selected therapies, and give time and space for recovery before repeating the process.
%20(7).jpg?width=1999&height=1333&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(7).jpg)
Your therapists will guide you through short bursts of cardio followed by measured breathing. This step encourages the sympathetic and parasympathetic nervous systems to balance each other better, improves blood flow in the brain, and releases neurochemicals that improve the brain’s ability to respond to therapy. One of those neurochemicals, brain-derived neurotrophic factor (BDNF), improves cognitive flexibility and has been shown to improve therapy outcomes in brain injury patients.
Your therapists can moderate exercise intensity based on whether you’re having trouble breathing, experiencing heart issues, or have any other medical conditions affecting your ability to exercise. Many long COVID patients need shorter bursts of exercise with a longer recovery period. They’re also more likely to need additional help with breathing exercises.
After exercise comes a combination of physical and cognitive therapies. Those therapies include…
.jpg?width=218&height=326&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It).jpg)
Some of these therapies may be combined. For example, you might balance on a Bosu board (exercising your vestibular system and the part of the brain governing balance) while tossing a football back and forth (hand-eye coordination and reflex response) and naming a city for each letter of the alphabet (word recall).
Or, during sensorimotor therapy, you might clap and stomp through a four-step repeating pattern to the beat of a metronome while also completing a visual maze taped to the wall.
%20(2).jpg?width=1000&height=445&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(2).jpg)
Recovery is interwoven throughout the day. Some examples include:
At the end of treatment, you’ll receive a final evaluation and recommendations for “homework” and any follow-up treatment. So far, we’re finding that many long COVID patients need to continue vision therapy at home. (The eyes often take six months to a year to fully respond to therapy.) We’ll also explain if you need follow-up attention from our team or from another specialist (such as an endocrinologist if we suspect you have hormone dysregulation).
Further reading: How this family of eight recovered from long COVID

While lifestyle changes are no substitute for therapy, they can make a tremendous difference in symptom burden. Some practices we encourage you to try at home are…
%20(5).jpg?width=1999&height=1333&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(5).jpg)
There aren’t many good healthcare options for COVID-19 survivors who suffer from ongoing symptoms, but at Cognitive FX, we’ve seen an average of 60% symptom improvement after just one treatment week. Many people experience improvements even after just the first day. We can provide more types of therapy at one time than any other treatment provider, and we make the most of your time with us. Your symptoms are real, they have a cause, and they can get better with appropriate treatment.
To determine if you are eligible for our treatment program, please schedule a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.
Your heart races when you stand. You hate the dizzy spells. Your head hurts, you’re exhausted, and you can’t think clearly like you used to.
COVID-19 can cause cognitive symptoms in some patients, such as short-term memory loss, difficulties concentrating, problems recalling words, and brain fog (a condition known as long COVID). While...

Long COVID is real. Data shared by the Centers for Disease Control and Prevention (CDC) from theHousehold Pulse Survey(July/August 2022) show that more than 40% of adults in the United States have...

You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.

You did everything right.

The fight with cancer is difficult enough, so it’s understandable if you’re frustrated and confused by the cognitive symptoms that can crop up after chemotherapy. Memory problems? Clouded thinking?...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY