Can’t Sleep After COVID? How to Treat COVID Insomnia (2026)
You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
COVID-19 can cause cognitive symptoms in some patients, such as short-term memory loss, difficulties concentrating, problems recalling words, and brain fog (a condition known as long COVID). While most initial studies focused on patients hospitalized with severe COVID symptoms, it became apparent that most long COVID patients developed their condition after only a mild case of COVID.
A new study (Smith et al.) published recently in the scientific journal Nature suggests that even mild cases of COVID can affect the brain. Using magnetic resonance imaging (MRI), the researchers compared the brains of the same patients before and after they contracted COVID-19. They found changes in areas of the brain which could tie into common symptoms, including loss of smell and taste, headaches, and memory problems.
Multiple media outlets extensively covered this study, but many of these offered the reader little more than a description of the results. As one of the only groups of healthcare providers that offer multidisciplinary long COVID rehabilitation regimens in the U.S. (without relying on underperforming medications so far), we can provide more narrative. Not only can we comment on what the recent study showed about post-COVID brain damage, but also…
Our treatment was originally designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, over 90% of our patients show improvement. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
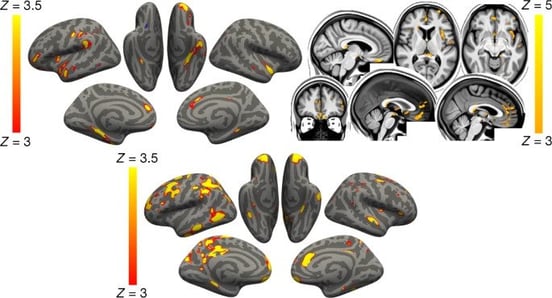
An image from the study published in Nature showing loss of grey matter in the brain after COVID infection.
The Smith et al. study is one of the first to focus on patients with a mild condition. With nearly 800 volunteers, it’s also the most extensive COVID-19 study involving brain scans.
Researchers from the University of Oxford, UK, administered cognitive tests to and scanned the brains of 785 patients aged 51 to 81. The brain imaging was done as part of the UK Biobank Project. This 30-year long-term study started in 2006 to follow 500,000 volunteers aged between 40 and 69 to study how genetics and the environment influence the development of different diseases. Researchers had already scanned more than 40,000 people when the coronavirus pandemic hit, making it the perfect tool to study before and after scans for the same patients.
The study included:
The results clearly show that even mild cases of COVID can have a real impact on the brain.
Less than six months after the infection, some patients had lost up to 2% of brain volume and gray matter thickness in specific areas of the brain, including the orbitofrontal cortex and the parahippocampal gyrus.
These losses may explain some of the symptoms experienced by patients with COVID. For example, the orbitofrontal cortex — located at the front of the brain, just above the eye sockets — has extensive connections with sensory areas, which may explain the loss of smell and taste. In addition, the parahippocampal gyrus, which sits just above the hippocampus at the base of the neck, plays a vital role in memory, decision making, and spatial processing, potentially explaining cognitive symptoms such as brain fog, memory loss, and anxiety.
For comparison, we all lose brain volume as we get older, but 2% is almost ten times greater loss than that experienced every year by older adults due to normal aging.
In addition, patients struggled more on cognitive tests after COVID, possibly caused by atrophy of a specific part of the brain called the cerebellum, a brain structure also linked to cognition. Patients took longer to answer the questions that measured attention, visual screening ability, and processing speed. There were no differences regarding memory recall, reaction time, or reasoning tests.
This study isn’t the first to show that COVID can affect cognitive function. Multiple studies show how COVID-19 patients score significantly lower in tests of attention, memory, and executive function than healthy people.
One worrying finding was that the differences between the infected and healthy patients increased as the patients got older. The differences were minimal for those in their 50s and 60s, but the gap extended considerably for those in their 70s and 80s. It’s difficult to say whether this happens because younger patients recover faster or because they’re not affected as severely as older patients.
In this study, the authors didn’t really explore the causes of these brain changes. However, we’ve written in the past about how COVID can affect the brain. One of these ways is by disrupting the normal distribution of oxygen and nutrients to the areas of the brain that need it.
In a healthy brain, neurons get oxygen and nutrients from a network of blood vessels that cover the brain. This relationship — called neurovascular coupling (NVC) — relies on a complex, dynamic signaling system in which the nerve cells request what they need when they need it.
However, a COVID infection can disrupt this dynamic. As a consequence, many areas in the brain stop being able to perform their functions. This is called neurovascular coupling dysfunction. As a result, patients experience many physical and cognitive symptoms, including headaches, brain fog, sleep problems, difficulty tracking conversations, difficulty multitasking, and more.
In the Smith et al. study, one of the main areas affected by the virus was the hippocampus. This area may be particularly vulnerable to neurovascular coupling dysfunction because it relies on adult neurogenesis, a process in which the adult brain produces new brain cells. This mechanism can’t continue without sustained supply of resources, which neurovascular coupling dysfunction could disrupt.
At first, researchers believed this process didn’t serve any purpose, but recent evidence shows that adult neurogenesis is particularly important to form recurrent but different short-term memories, such as where you left your car keys today instead of where you left them yesterday.
In short, mild cases of COVID may cause these changes in brain tissue because the virus disrupts normal NVC in the hippocampus and surrounding areas. In turn, this may block the process of neurogenesis and lead to brain shrinkage and progressive cognitive decline and short-term memory loss. The same tissue damage can be detected in aging patients and those with neurodegenerative disorders (such as Alzheimer’s disease) or traumatic brain injuries.
It is likely that NVC is not the only factor involved in these brain abnormalities. Other possible contributors include:

In the Smith et al. study, the interval between the original SARS-CoV-2 infection and the second round of imaging was less than six months. This period is not enough to determine if the loss of gray matter and other cognitive deficits would persist and develop into long COVID or reverse back to normal.
It is possible that the cognitive changes caused by the virus may endure for a long time. For example, a report found that 12 months after their infection, older adults in Wuhan, China, were still showing signs of cognitive impairment. In contrast, their spouses — who were not infected with the virus and worked as a control group — did not show the same symptoms.
However, as the abnormal changes are associated with loss of smell, it’s plausible that once patients recover their sense of smell, they also regain their cognitive function. A study found that, although patients were still experiencing some cognitive difficulties six months after their infection, there was a marked improvement in neurological and cognitive function since the illness.
All that said, we’ve found that many symptoms of long COVID are reversible with treatment. That’s because neurovascular coupling dysfunction and many of the conditions associated with it, such as vision problems, are reversible.
When reports of COVID long haulers first surfaced, we noticed that the symptoms for this condition were very similar to those of our patients with post-concussion syndrome (PCS).
We confirmed the similarity between long COVID and PCS using brain imaging. The long COVID patients we’ve imaged show clear neurovascular coupling dysfunction.
Note: We’ve also found that many long COVID patients experience autonomic nervous system dysfunction, something they share in common with mild traumatic brain injury patients. We account for that in our treatment program.
Because of that, we adapted our treatment protocols to suit COVID long haulers. This approach is successful because long COVID causes mild brain injury; at its heart, our treatment program is for the long-term symptoms of brain injury. At our clinic, we also treat patients with persistent symptoms from brain infections, CO poisoning, “chemo” brain, transient ischemic attack, and others, all of which have a similar effect on the brain.
For all our patients, the aim is to address symptoms by restoring healthier neurovascular coupling in the brain, including the hippocampus and the orbitofrontal cortex. Before treatment starts, patients undergo a brain scan called functional neurocognitive imaging (fNCI) to find out which areas were affected by the virus. The scan assesses blood flow dynamics in 56 brain regions while the patient performs a series of cognitive tasks. fNCI also looks at communication between brain regions.
Our therapists then use these results to design a customized treatment plan for each patient, which we call Enhanced Performance in Cognition Treatment, or EPIC for short.

During the EPIC treatment, patients are treated with multidisciplinary therapies to restore healthier NVC, autonomic function, and vision. Most patients see improvements in symptoms such as fatigue, brain fog, sleep disturbances, visual difficulties, and headaches, to name just a few.
Daily sessions of cardio exercise, typically done on a stationary bike or treadmill, is a key component of our treatment program. Our therapists monitor how patients react in these sessions and adjust the duration and intensity of each activity as needed. Studies show that exercise stimulates adult neurogenesis (as explained above) through a chemical released in the brain called brain-derived neurotrophic factor (BDNF). BDNF is involved in keeping these new nerve cells alive, which in turn improves memory and learning.
Preparing the brain with cardio exercise makes it more receptive to the other therapy appointments you have each day. Those therapies include…
Our therapists use cognitive therapy, for example, to address any cognitive impairments, including issues related to memory, attention, executive functioning, and word finding. Exercises include word games, puzzles, finding hidden patterns and memorizing a list of words.

During her EPIC week, cognitive therapy was Sam Pembelton’s favorite type of therapy. “The one I really noticed that I improved in throughout the week was the cognitive activities. It was an hour-long therapy and it was just one-on-one with someone. You’d do a cognitive activity, like sorting through a deck of cards, but at the same time someone would give you a four-letter sentence and you'd have to arrange it alphabetically while you were still sorting through the cards. It was a lot of multitasking!”
Sensorimotor therapy is another type of therapy we use at Cognitive FX. You’ll receive sensors for your hands and feet that measure how closely you’re able to tap, clap, and stomp in time to a given beat. At the same time, you might complete various cognitive tasks, such as playing Taboo or solving a visual search puzzle.
-2.jpg?width=1999&name=image3%20(1)-2.jpg)
These exercises might sound strange, but their effect on the body is real. One of our long COVID patients, Sarah, shared how she felt just one day into treatment: “I woke up, and I felt a mental clarity like I could see for the first time in 20 months. It's like getting glasses for the first time. I could think clearly. I know it sounds weird to say that just after one day, but that's what it was. It turned my brain on.”
We’ve found that many of the COVID-19 survivors who come to us experience breathing difficulties. This is not surprising given that the virus starts by attacking the respiratory system. Our therapists teach patients a range of exercises, such as deep breathing or diaphragmatic breathing, to help them relax and control their breathing. Many of our patients continue to use these exercises at home to continue improving.
At the end of treatment, patients undergo another brain scan to determine how their brains improved during treatment. Patients also meet with a therapist to assess progress and receive a series of exercises to do at home to continue their journey to recovery.
Our treatment was originally designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, over 90% of our patients show improvement. Thus far, we’ve seen similar results with Long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.
Your heart races when you stand. You hate the dizzy spells. Your head hurts, you’re exhausted, and you can’t think clearly like you used to.
.png?height=175&name=Physical%20therapy%20covid%20(2).png)
Long COVID symptoms such as fatigue, muscle weakness, joint pain, poor endurance, and respiratory problems can have a significant impact on your daily routine. Some long COVID patients’ symptoms are...

You’d think a family of eight with the foresight to pull their children out of school earlier than the rest of the nation would be safe during the COVID-19 pandemic. Instead, seven out of the eight...
Memory and attention problems are common in long COVID patients: A recentstudyshowed that 70% of COVID long haulers experience memory and concentration difficulties for months after their initial...

Many patients have heard of the most common long-term effects of COVID-19: symptoms such as breathing issues, brain fog, and constant fatigue. But there is mounting evidence that COVID-19 may also...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY