Long COVID symptoms such as fatigue, muscle weakness, joint pain, poor endurance, and respiratory problems can have a significant impact on your daily routine. Some long COVID patients’ symptoms are so severe that they need a reduced work schedule or are no longer working due to their illness. Persistent symptoms can follow both mild COVID and cases that required treatment in the ICU.
Health professionals are starting to recognize how physical rehabilitation can be beneficial for these patients. For example, an organization called World Physiotherapy — which includes 125 member organizations and represents more than 660,000 physiotherapists worldwide — published a briefing paper arguing that physical therapy is a fundamental part of long COVID-19 recovery and can improve function in people living with long-term symptoms.
Physical therapy is an important component of the treatment regimen we offer long COVID patients at our clinic, Cognitive FX. But for most patients, physical therapy is not the whole solution. Many patients need a combination of therapies in order to resolve the underlying issues causing their post-COVID symptoms. That’s why we offer a multidisciplinary approach that is tailored to each patient and which produces better results than relying on a single therapy.
In this article, we’ll look at …
Our treatment was originally designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, over 90% of our patients show improvement. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific symptoms of long COVID and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
How Does Physical Therapy Help Long COVID Patients?.jpg?width=1000&height=445&name=Physical%20therapy%20covid%20(6).jpg)
Long COVID patients often feel fatigued, have trouble breathing, and can struggle to climb stairs or walk a few minutes down the block. As a result, they spend more time sitting or lying down, which further contributes to low endurance, exercise intolerance, and poor muscle strength.
Physical therapy can help these patients improve their range of movement and return to their prior level of functioning. Studies show that it can lead to significant improvements in many post-COVID-19 symptoms — not just physical symptoms, such as fatigue and fitness, but also emotional symptoms, such as anxiety and depression.
Typically, sessions include a variety of different exercises, ranging from resistance training and aerobic exercises to respiratory exercises and balance training. Some interventions focus primarily on specific symptoms, such as respiratory problems or poor balance, while others offer a more generalized approach to improve fitness and increase quality of life. If you engage in physical therapy, make sure your therapist is not simply offering a generic “one-size-fits-all” program that may not be suitable for your condition.
Physical therapy for those recovering from long COVID-19 aims to:
Improve Respiratory Function
Poor respiratory function is common in COVID-19 patients. Even patients who were previously fit and active may start to struggle with shortness of breath just from climbing stairs.
Physical therapy is a way to address these issues. Studies show that it can improve endurance, muscle strength, and posture, which all contribute to better lung capacity. In other words, physical therapy helps your lungs function more efficiently and take in more oxygen with each breath, increasing oxygen saturation so you can breathe easier.
With targeted exercises and breathing techniques, your therapist can help you recover strength and redevelop more efficient breathing patterns.
Reduce Fatigue
Fatigue is another common symptom of long COVID-19. For some patients, post-COVID fatigue appears during physical exercise (exercise intolerance) or after engaging in exercise or cognitive activities (known as post-exertional malaise). For others, the fatigue is always present. Some patients may be diagnosed with chronic fatigue syndrome by providers who don’t recognize the presence of long-haul COVID.
In this case, physical therapists can offer guidance, education, and reassurance. They work to help patients gradually recover energy levels and return to their normal daily activities. Physical therapists typically use aerobic exercises and resistance training to improve mobility and fitness. Therapists also teach patients when to be active and when to rest, as well as relaxation techniques and how to pace themselves during the day to avoid becoming overtired.
Improve Cardiovascular Endurance.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(4).jpg)
Cardiac injury is reported in many studies as an important COVID-19 manifestation. For example, just over 19% of hospitalized patients in the cited study experienced cardiac injury. This value increases dramatically in patients with pre-existing heart issues.
Physical therapists can guide patients with serious heart problems through gentle exercises that are not strenuous. These exercises aim to improve range of motion and prevent deconditioning and stiffness. For milder cases, typical exercise sessions may involve resistance training and aerobic exercises on equipment such as a stationary bike or treadmill.
Many physical therapists will closely monitor your heart rate, blood pressure, respiration rate, and oxygen level while you exercise to assess how your body responds. If you experience chest tightness or pain, difficulty in breathing, dizziness, palpitations, sweating, or balance issues, inform your therapist.
Increase General Fitness and Muscle Strength
After long periods of inactivity and not engaging in physical exercise, some patients recovering from SARS-CoV-2 infection experience muscle weakness, which can severely affect their everyday lives.
Physical therapists can use a range of exercises, including aerobic sessions and endurance training, to help patients improve their balance, posture, and muscle strength, as well as to reduce breathing problems and improve quality of life. Stretching and strength exercises also help restore your general fitness and ability to move.
Relieve Joint Pain
Joint pain is a common symptom in long COVID patients that can affect a specific area or spread more widely. Many patients complain about sore and stiff joints, especially the shoulders, neck, back, hips, and knees. As you start using these joints less than you would normally, they can become weak and deconditioned. As a result, you might find it hard to grip objects, lift your arms above your head, or even just stand up.
In this case, your therapist will suggest stretching exercises to increase your range of motion. The aim of these exercises is to help reduce joint pain and make you feel more in control of them. Certain strengthening exercises and training on proper posture and body mechanics help in this situation as well.
Improve Sleep
Many post-COVID syndrome patients complain of sleep impairments, including waking up frequently during the night, struggling to go to sleep, and daytime drowsiness.
Studies show that engaging in regular physical activity can help with sleep. Your physical therapist can teach you various exercises to stretch and strengthen your muscles before going to bed to help you sleep better. Physiotherapists can also help improve your quality of sleep with massage therapy and exercises designed to relieve any pain you may have.
Reduce Depression and Anxiety
The effects of COVID-19 can include a wide range of psychological difficulties, such as anxiety, panic, stress, and depression. For these patients, aerobic sessions combined with breathing exercises and mindfulness can be effective in reducing symptoms. For example, breathing techniques can help relieve tightness in the chest, ease breathing, and promote relaxation.
Multidisciplinary Therapy Regimens Are Better than Physical Therapy Alone.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(5).jpg)
Physical therapy sessions help reduce pain, improve overall health and well-being, and contribute to long COVID patients’ return to their previous level of functioning. But long COVID can cause a number of complications (sequelae) in the body that physical therapy alone cannot address.
In most patients, several of these conditions are concurrent. While physical therapy can facilitate improvements in brain function, and there are providers who take this into account, specialists are often needed for vision, vestibular, and autonomic rehabilitation. And for more complete brain recovery, multimodal approaches are more effective.
At Cognitive FX, we specialize in treating lingering symptoms from brain injury. Our typical patient suffers from post-concussion syndrome (PCS). PCS patients continue to experience symptoms for months or even years afterward a concussion. Shortly after the COVID-19 pandemic started, we noticed that COVID long haulers had surprisingly similar symptom profiles to those of PCS patients.
We scanned the brains of a few long COVID patients and confirmed that they were suffering from the same type of brain dysfunction that we treat at our clinic. We adjusted our recovery program accordingly for the needs of COVID long haulers (such as accommodating certain pulmonary problems and heart complications, although there are some complications we can’t accommodate). Now, our rehabilitation program is available to any long COVID patient who passes our screening criteria. (You can start the process here.)
Long COVID Treatment at Cognitive FX
.jpg?width=251&height=342&name=Physical%20therapy%20covid%20(2).jpg)
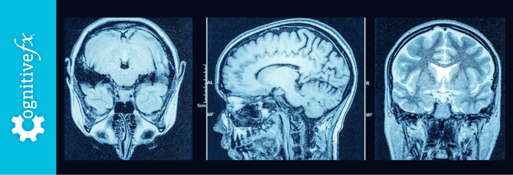
Before treatment starts, patients undergo a full examination with our clinicians, including a check of medical history and current symptoms. Our patients also receive a brain imaging scan called functional Neurocognitive Imagining (fNCI), which allows our team to determine how the COVID virus affected your brain.
In a healthy brain, neurons receive oxygen and nutrients from a network of blood vessels in the brain. This process, called neurovascular coupling (NVC), allows nerve cells to request the right amount of resources at the right time and in the right location. The problem is that long COVID disrupts this connection, often affecting regions throughout the brain. As a result, patients experience a wide range of symptoms (depending on what areas were affected), such as headaches, brain fog, difficulty tracking conversations, sleep disruptions, and more.
Using the fNCI scan, our team can identify exactly what areas of the brain were affected by NVC dysfunction. The scan assesses blood flow dynamics throughout 56 regions in the brain while the patient performs a series of cognitive tasks. fNCI also looks at communication between brain regions.-1.jpg?width=552&height=303&name=Physical%20therapy%20covid%20(3)-1.jpg)
Our therapists then use the imaging results to design a custom-made treatment plan for each patient to address the affected areas identified in the scan. We call our treatment Enhanced Performance in Cognition Treatment (EPIC treatment).
During EPIC treatment, patients go through a repeating, three-stage cycle:
- Prepare the brain for therapy.
- Activate the brain with selected therapies.
- Recover and rest (before the next cycle).
Prepare
.jpg?width=292&height=334&name=Physical%20therapy%20covid%20(1).jpg)
Patients engage in short bursts of cardio, followed by breathing exercises. This improves blood flow in the brain and triggers the release of neurochemicals that improve the brain’s ability to respond to therapy. One of these chemicals is called brain-derived neurotrophic factor (BDNF), which promotes the growth of brain cells and improves communication between different areas of the brain. In practical terms, every time you exercise, BDNF makes your brain more flexible and able to benefit more from subsequent therapy.
During these sessions, patients are closely monitored by our therapists. If needed, they can adjust exercise intensity if patients start to experience trouble breathing, heart issues, or any other medical conditions. We find that many long COVID patients need shorter bursts of exercise followed by a longer recovery period. Many COVID patients need additional help with breathing exercises.
Activate.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(3).jpg)
After exercise, patients complete a series of different therapies including:
These therapies cover a wide range of exercises. For example, our therapists may ask you to balance on a Bosu ball while tossing color-coordinated tennis balls back and forth and naming a food for each letter of the alphabet. This activity engages brain regions responsible for balance, hand-eye coordination, and word recall at the same time..jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(7).jpg)
Or, during neurointegration therapy, you might combine visual and vestibular function by seeking out and tapping letters of the alphabet positioned around you in a 3D cage (pictured above).
Recover-1.jpg?width=552&height=246&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(3)-1.jpg)
Patients have multiple periods of rest and relaxation during the day. This may include:
- Neuromuscular massage to the neck and shoulders to relieve tension, improve circulation, and alleviate pain. It’s common for long COVID patients to experience neck stiffness and headaches, so this type of massage can be very beneficial.
- Patients can relax in a dark room with ambient sounds while listening to binaural beats. The app produces two close sound frequencies that the brain averages into one single frequency. After a while, natural brain waves begin to copy that frequency, a process similar to what you may experience through meditation. This helps the patient to relax and the brain to rest.
- Patients also learn mindfulness techniques. This is a type of meditation where you focus on what you’re feeling in the moment. Mindfulness involves breathing techniques, guided imagery, and other practices to relax the body and mind and help reduce stress.
At the end of the treatment, patients receive a second fNCI scan. This allows our team to understand how your brain is responding to treatment. After your follow-up scan, one of our clinicians will also meet with you to go over your results and give you some “homework.” Homework typically includes some combination of aerobic exercise, cognitive games, and cognitive rest to do at home. It’s an important part of your recovery journey.
Continue Your Recovery Journey at Cognitive FX-1.jpg?width=552&height=306&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(4)-1.jpg)
There aren’t many good healthcare options for COVID-19 survivors who suffer from ongoing symptoms. Many primary care doctors don’t have the resources to treat it and may not have established referral relationships with reliable, local treatment providers.
But at Cognitive FX, we’ve seen an average of 60% symptom improvement after just one treatment week. Many people experience improvements after just the first day. We can provide more types of therapy at one time than any other treatment provider. We make the most of your time with us. Your symptoms are real, they have a cause, and they can get better with appropriate treatment.
To determine if you are eligible for our treatment program, please fill out our online form and schedule a consultation.

.jpg?width=1000&height=445&name=Physical%20therapy%20covid%20(6).jpg)
.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(4).jpg)
.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(5).jpg)
.jpg?width=251&height=342&name=Physical%20therapy%20covid%20(2).jpg)
-1.jpg?width=552&height=303&name=Physical%20therapy%20covid%20(3)-1.jpg)
.jpg?width=292&height=334&name=Physical%20therapy%20covid%20(1).jpg)
.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(3).jpg)
.jpg?width=1999&height=1333&name=Physical%20therapy%20covid%20(7).jpg)
-1.jpg?width=552&height=246&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(3)-1.jpg)
-1.jpg?width=552&height=306&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(4)-1.jpg)