More than 20 million Americans have lingering symptoms that can be described as long COVID (or “post-COVID conditions”), but doctors and scientists are still researching why it develops. As a result, these patients often struggle to get a diagnosis and find a suitable treatment for their condition.
Understandably, it’s easy for these patients to get frustrated and consider alternative treatments. There are many products and supplements claiming to help with long COVID, so how do you know which ones are safe and trustworthy? Sometimes, there is no information available, or it is presented in a difficult-to-understand format.
For example, colloidal silver has been promoted as a health supplement that can boost the immune system and treat COVID-19, but those claims have been found to be fraudulent. Not only is colloidal silver not a legitimate COVID-19 treatment, but it can also interact negatively with certain prescription drugs, cause skin discoloration, and even result in serious organ damage.
Unfortunately, there is no miracle supplement that can cure long COVID. But that doesn’t mean you’ll be stuck taking 10 different medications for your condition. There are natural ways to treat long COVID.
At Cognitive FX, we offer a scientifically sound regimen of multidisciplinary therapy that has already shown success in treating long COVID. In addition, we’ll explain what you can do naturally at home to improve long COVID symptoms.
Here’s a quick overview of what we’ll explain in this post:
After just one week of treatment, 90% of our patients already show symptom improvement. Using advanced brain scan techniques, we can also see how our patients' brains respond to treatment. Thus far, we’ve seen strong results with long COVID patients who pass our current screening criteria. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
What Are the Symptoms of Long COVID?
The term “long COVID” describes symptoms that last more than a few weeks after a COVID-19 infection. This condition has been called by many names, including post-acute COVID-19 Syndrome (PACS), chronic COVID-19 syndrome, and long-haul COVID-19.
It’s still not clear how common long COVID is, with estimates varying widely from 9% to 80% of post-COVID patients. As this is such a new disease, each research team used its own definition, which can explain (at least partially) these reported differences. To address this issue, in October 2021, the World Health Organization (WHO) proposed the name “post-COVID-19 condition” and suggested a unifying definition as “the condition that occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually three months from the onset of COVID-19, with symptoms that last for at least two months and cannot be explained by an alternative diagnosis.”
The likelihood of developing long COVID is not related to how ill you were when you first got COVID. This means even if you had a mild or asymptomatic case, you could experience long-term symptoms. In addition, the wide-ranging symptoms make it very difficult for doctors to diagnose. One study reported over 200 symptoms that can fluctuate or even appear out of the blue after patients have recovered.
Some symptoms are the same as COVID-19 and include:
- Fatigue
- Shortness of breath
- Loss of sense of taste or smell
- Difficulty concentrating
- Muscle ache
- Headaches
- Cough
- Memory loss
- High temperature
- Sore throat
However, many patients also experience a wide range of other symptoms, including:
- Joint pain
- Chest pain or tightness
- Breathlessness
- Heart palpitations
- Dizziness
- Pins and needles
- Tinnitus or earache
- Nausea
- Diarrhea
- Abdominal pain
- Loss of appetite
- Skin rashes
- Memory problems
- Concentration problems
- Brain fog
- Depression and anxiety
- Fatigue
- Extreme tiredness
- Problems sleeping
- Changes in the menstrual cycle
What Causes Long COVID Symptoms?
Even after most countries around the world have largely lifted restrictions and the number of COVID-19 cases is finally going down, there are still many questions about long COVID, including why some patients develop long-term symptoms and what mechanisms are behind these symptoms.
There are several theories to explain these long-lasting symptoms. As researchers investigate more, it’s becoming increasingly clear that it’s not just one factor, but a combination of different factors which affect each long hauler in a different way.
Here are a few of the most prominent causes of long COVID symptoms:
Neurovascular Coupling Dysfunction
Scientists studying how COVID impacts the body found a link between the endothelium and long COVID.
The endothelium is the thin membrane that lines the inside of blood vessels. In the brain, this is a key component of the neurovascular unit, which also includes vascular cells, glial cells, and neurons.
In a normal brain, neurons receive oxygen and nutrients from a surrounding network of blood vessels. This is called neurovascular coupling, and it involves a delicate mechanism by which neurons can “order” the resources they need to be delivered at the right time and to the right location.
When COVID-19 damages the endothelium, it disrupts this connection between neurons and blood vessels. As a consequence, affected areas in the brain will not function as well as they should because they can no longer receive the resources they need to operate normally. This is called neurovascular coupling dysfunction and results in many of the physical and cognitive symptoms described above.
Further reading: What is neurovascular coupling?
Dysfunction of the Autonomic Nervous System
Many studies have also confirmed that the COVID virus causes dysfunction of the autonomic nervous system (ANS).
In simple terms, the ANS controls many bodily functions, including heart rate, breathing patterns, and blood pressure. Two parts of the ANS include the sympathetic (SNS) and the parasympathetic nervous system (PNS). The SNS is responsible for our “fight or flight” reactions, and the PNS controls our “rest and digest” processes.
Under normal circumstances, PNS and SNS work together to allow your body to respond to the environment. However, long COVID can disrupt this fine balance, causing many different symptoms including exercise intolerance, headaches, blood pressure changes, urinary incontinence, heart palpitations, problems breathing, and more. Curiously, the severity of the original COVID-19 infection doesn’t necessarily correlate with the degree of autonomic dysfunction, and even patients who had a mild case can develop considerable autonomic dysfunction.
Autonomic nervous system dysfunction and neurovascular coupling dysfunction are closely related; many patients develop both.
Further reading: Long COVID Can Cause POTS and Dysautonomia
Vision & Vestibular Symptoms

Many patients who get COVID develop some form of eye (vision) and ear (vestibular) symptoms, and these are among the complaints that end up persisting for a long time.
Vision symptoms may include dry eyes, redness, itching, blurry vision, sensitivity to light, and the feeling that there is a foreign particle in the eye. Vestibular symptoms include dizziness, vertigo, lightheadedness, spatial disorientation, sleep disturbances, and more. Sometimes there’s an overlap between vision and vestibular symptoms. Many of these are common during the acute phase but they’re also a sign of long-term COVID.
For example, If you wake up feeling normal (no headaches or dizziness) but then start to struggle as the day goes on, it’s likely that you’re experiencing vision-related symptoms. Your eyes rest overnight but become more tired during the day, causing symptoms to recur.
With vestibular issues, it’s often the opposite. In a healthy brain, the vestibular system knows when you’re asleep because you don’t really move your head. During this period, most of this system is not active, and “non-adaptive fibers” in the utricle and saccule (which are involved in orientation and balance) take over. For long haulers, however, this mechanism is disrupted, making it harder to fall asleep or causing headaches, dizziness, and nausea in the morning when you wake up.
Other Possibilities
There are several other theories to explain long COVID symptoms, including:
- Tiny blood clots: Many researchers believe tiny blood clots may be impairing blood flow in different organs, including the lungs, causing long-term symptoms. This idea gained some credence when a South African team reported that such clots can linger for a long time in the blood of long haulers.
- Persistent infection: It’s also possible that remnants of the SARS-CoV-2 virus may stay in your body after the original infection, causing long-lasting symptoms. Researchers from the U.S. National Institutes of Health analyzed tissues from 44 people who had COVID and found viral RNA in their brains, muscles, guts, and lungs. They’re now trying to establish how this lingering virus is driving illness in long COVID patients.
- Exaggerated immune response: Instead of returning to normal levels after fighting the infection, the immune system in some patients stays on constant high alert. This chronic inflammation can cause a series of health problems, including cognitive and physical symptoms.
- Nerve damage: New research suggests that damage to the vagus nerve (which extends from the brain to the torso) may be responsible for many of the long COVID symptoms, including abnormal heart rate, dizziness, and gastrointestinal problems. Researchers found a range of structural and/or functional alterations in the vagus nerve of long haulers, including nerve thickening, trouble swallowing, and symptoms of impaired breathing. Since the vagus nerve is intimately involved with autonomic nervous system regulation, it’s not surprising that any damage to it could drive symptoms related to ANS dysfunction.
- Change in habits post-COVID: The COVID-19 pandemic has upended much of society in ways we never experienced before. Changes in diet were common during the months of lockdown, with patients resorting to snacking mostly on foods with poor nutritional value, leading to fatigue. Research shows that sleep disturbances also became more prevalent since the start of the pandemic, increasing anxiety and depressive symptoms, as well as irritability, changes in mood, and lack of concentration. This, combined with less exercise, resulted in a lower quality of life — particularly in COVID long haulers.
Treatment at Cognitive FX

At Cognitive FX, we instead use a combination of exercise and multidisciplinary therapies to treat COVID long haulers. Our treatment addresses neurovascular coupling dysfunction, autonomic nervous system dysfunction, vestibular imbalance, and vision problems, which — as we explained earlier — are some of the main mechanisms behind long COVID symptoms.
You can learn more about how we developed our treatment program here.
The key to our success is treating long COVID for what it is: a brain injury. We’ve adapted our regular brain injury treatment program to address the specific needs of long COVID patients. For example, long COVID patients often experience more severe breathing problems than some of our other brain injury patients, so our therapists spend extra time walking them through helpful breathing exercises. Some COVID patients suffer from cardiovascular complications; when that happens, we adjust their exercise routine accordingly.
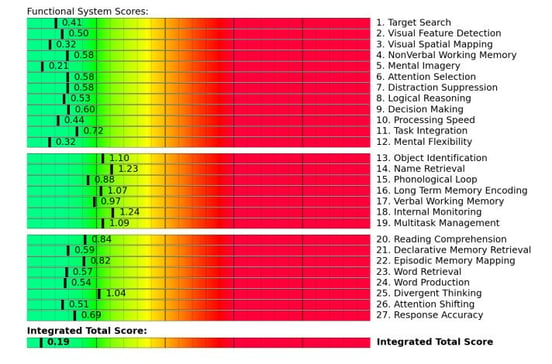
Every long COVID patient is different, so we begin treatment with a full assessment of your physical and cognitive capabilities, your symptom profile, and your medical history. Most importantly, we use advanced brain imaging technology called functional Neurocognitive Imagining (fNCI), which is a type of functional MRI capable of tracking blood flow throughout the brain. Using fNCI, our team can identify which areas of your brain were affected and how healthy their communication is with other areas of the brain. We examine 56 brain regions while you execute a series of cognitive tests.
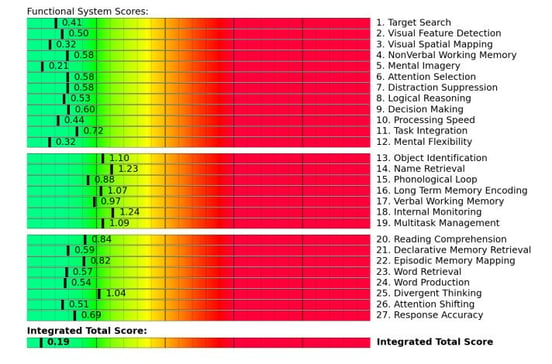 An example fNCI scan results summary from a healthy patient.
An example fNCI scan results summary from a healthy patient.
Using the results from the scan, our treatment team tailors a treatment plan specifically for your needs. During treatment — which we call Enhanced Performance in Cognition, or EPIC for short — you’ll engage in a series of cardio exercises along with other therapies such as cognitive, sensorimotor, neuromuscular, and vision therapies, to name just a few. These therapies help your brain and body recover while improving your symptoms.
-1.jpg?width=1999&name=image5%20(2)-1.jpg)
You’ll also see a psychologist who can help with symptoms like anxiety and depression. In addition, you will learn mindfulness meditation to help calm the mind and body. If we feel that you may need more support for your mental health, we will make specific recommendations for follow-up near your home.
On the last day of treatment, you’ll undergo a second scan to monitor your improvement. Results for our long COVID patients so far have been positive, with patients reporting significant improvement in symptoms like headaches, dizziness, and brain fog.
After just one week of treatment, 90% of our patients already show symptom improvement. Using advanced brain scan techniques, we can also see how our patients' brains respond to treatment. Thus far, we’ve seen strong results with long COVID patients who pass our current screening criteria. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Supplements to Treat Long COVID Symptoms: Can They Help?

If you’re struggling to find an effective treatment for the long-term effects of coronavirus infection, you may have been looking for alternative medicines.
It may be tempting to try, but there’s very limited research regarding the use of these interventions to treat long COVID. Also, be aware that there are many dangers involved with self-prescription, such as harmful drug interactions, side effects, and incorrect dosing. Long COVID is a complex condition affecting many organs in the body and causing a variety of symptoms; interactions between products become more likely if you try multiple treatments at the same time.
There is some research starting now in this field, but it’s still in its infancy. Most of the products listed below have not been tested fully. Listing these products here does not mean we endorse them; it is for your information only. Before starting any supplement, consult with your doctor.
One of the few natural products that have been tested in COVID patients includes prebiotics and probiotics. Long COVID patients often complain of digestive problems, including abdominal discomfort and diarrhea. This may be caused by disruption to their gut microbiota, with significant losses of good bacteria such as Lactobacillus and Bifidobacterium. It is likely that using prebiotics and probiotics can regulate the balance of intestinal microbiota and reduce the risk of secondary infection in those patients.
No studies so far evaluated the use of probiotics for the management of long COVID, but according to the International Scientific Association of Probiotics and Prebiotics, many researchers are assessing the ability of various probiotic strains to reduce the viral load via different mechanisms of action. In the U.K., there is also an ongoing clinical trial to test the efficacy of a product called Live Biotherapeutic MRx-4DP0004, which contains Bifidobacterium; and in the U.S., researchers are testing a product with Lactobacillus to see whether it has the ability to decrease infections and improve long term outcomes.
Some studies have also shown that certain vitamin and mineral supplements (such as Vitamin C) may be able to help long haulers recover from fatigue. These products may help the body fend off viral infections and boost immunity, which may in turn prevent prolonged post-COVID fatigue and gastrointestinal problems.
There is some limited data suggesting that some supplements may also improve cognitive and mental symptoms, like brain fog and anxiety. Vitamins B and C, iron, and magnesium are all involved in energy metabolism and can help fight physical and mental fatigue. The results look promising, but more research is needed to assess the efficacy of using dietary supplements for COVID long haulers.
Melatonin is another supplement currently being tested for long COVID treatment. There are no studies yet involving long haulers, but in patients suffering from diseases with high levels of inflammation, the use of melatonin successfully lowered the levels of circulating cytokines and improved symptoms. Researchers are further exploring its use to treat COVID-19 by focusing on melatonin’s ability to reduce blood vessel permeability, reduce anxiety, and improve sleeping patterns.
Honeybee products, including honey, beeswax, and propolis, are commonly used for their medicinal properties, including for symptoms of viral respiratory tract infections. There are no studies with COVID long haulers, but one study showed that propolis (a mix of resin and beeswax) reduced the risk of shock, respiratory failure, and kidney injury in hospitalized patients with COVID. The authors attributed the results to propolis’ antiviral and anti-inflammatory properties, suggesting that it may also help treat long COVID.
Evidence also suggests that curcumin has the potential to help with long COVID due to its ability to block viral replication and control inflammatory cytokines. Further research is needed, including finding a way to increase its bioavailability (which reflects the body’s ability to absorb and use the helpful components).
When it comes to addressing symptoms like brain fog and other cognitive issues, natural flavonoids luteolin and quercetin may be an option. Both have broad antiviral properties, inhibit neuroinflammation, and reduce cognitive decline. Like all the other supplements, further research is needed.
Despite the fact that, in theory, these natural products may be able to help long haulers, the reality is that further research is needed to confirm safety and efficacy. And even if they do help, these supplements are never going to be a cure for long COVID. It takes a more comprehensive treatment approach to recovery than supplements alone can offer.
Instead, request a consultation with the Cognitive FX team to see how we can help you. You need an experienced healthcare provider specialized in brain injuries who can identify the cause of your long-hauler symptoms and develop an appropriate, comprehensive treatment plan.
What You Can Do at Home

Beyond therapy and supplements, there are a few key steps you can take at home to promote recovery from long COVID.
Follow a Balanced Diet
If you’re experiencing the effects of long COVID, what you eat will have a major impact on how you feel. Choosing to follow a healthy and balanced diet is a good way to promote your recovery at home.
Some foods, such as oily fish rich in omega-3, nuts, and seeds, can be helpful to reduce the inflammatory response characteristic of this viral disease. Also, fruit and vegetables are high in antioxidants and can counteract oxidative stress caused by inflammation. In contrast, you should avoid foods like highly processed foods, high in fat or high in sugar, as these may have a pro-inflammatory effect.
Further reading: Nutrition for a recovering brain
Rest Frequently during the Day
Patients often find that attempts to push through fatigue and migraines make them feel worse and exacerbate the intensity of their symptoms. While you’re recovering, rest as much as you need, and allow yourself more time to complete your normal routine.
- Pace yourself during the day. Carefully plan what you need to do but don’t overexert yourself. Take breaks when needed.
- Break complex or time-consuming tasks into smaller chunks and alternate between easy and difficult activities.
- Pick the time of the day when you’re more alert to complete the most important or difficult tasks.
- Practice breathing exercises to control your breathing patterns and relax both body and mind.
Follow a Good Sleep Pattern
Recent studies show that up to half of long haulers complain of sleep disorders. This is not surprising as sleep patterns can be disrupted after a viral infection. If you have trouble falling asleep or wake up frequently during the night, it’s important that you address this issue. There is a close relationship between poor sleep and poor mental health. A poor night’s sleep can make feelings of depression, anxiety, and stress feel worse.
- Go to bed early and follow the same pattern every day.
- Avoid screens close to bedtime and use blue-light filters when you do use them.
- Restrict caffeine to the morning only (although it’s better if you can do without it while you recover). Avoid alcohol at night as well.
- Make sure your bedroom has a relaxing atmosphere that can help you sleep. You might need to declutter or add a source of white noise.
- If you need it, take a short nap during the day, but no longer than 30 minutes. Longer naps can actually be counterproductive.
Engage in Regular Exercise
Physical activity plays a vital role during recovery from long COVID. Choose something that you can achieve without causing a massive flare-up of your long-haul symptoms. There’s a fine balance between doing too much and not doing enough. We highly recommend intervals: Short bursts of cardio (around 30 seconds to one minute) followed by one to two minutes of controlled breathing.
To know when it’s safe to continue exercising versus when you should stop, follow this simple rule:
- If you’ve noticed three symptoms starting or getting worse during exercise, then it’s time to stop.
- Similarly, if a single symptom is getting worse quickly, going from what you would rate as a 1 (mild) to a 4 (severe), it’s a sign that you need a break.
- If you’re just feeling a slight headache or experiencing mild dizziness, it’s okay to continue. Exercise helps the brain heal and will keep other symptoms under control in the future.
Reduce Stress in Your Life
Dealing with long COVID can be very stressful. As you’re able, plan some “you” time during the day. Go for a walk, sign up for a yoga class, or simply sit in a quiet place reading a good book. Learn your symptom triggers and avoid or limit situations that may push you past your limits. For example, if driving in heavy traffic is too much for you, look for an alternative route or travel at a different time.
You may find it helpful to stick to a consistent daily routine. And don’t be afraid to ask loved ones for help when you need it.
Remember that some days will be better than others. Recovery isn’t linear, but you can keep improving with time.
FAQ: Does the COVID-19 Vaccine Help with Long COVID?
While the COVID-19 vaccine is effective at reducing hospitalization and death, a new study showed that it only reduces the chance of developing long COVID by 15%. Some scientists are investigating whether the booster shot can help current COVID-19 long haulers recover, but the results are mixed. While some patients report feeling better — possibly because of a renewed antibody response — not all notice an effect, and no rigorous studies have confirmed a benefit for long haulers.
After just one week of treatment, 90% of our patients already show symptom improvement. Using advanced brain scan techniques, we can also see how our patients' brains respond to treatment. Thus far, we’ve seen strong results with long COVID patients who pass our current screening criteria. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.



-1.jpg?width=1999&name=image5%20(2)-1.jpg)







.png?height=175&name=Physical%20therapy%20covid%20(2).png)


