Your heart races when you stand. You hate the dizzy spells. Your head hurts, you’re exhausted, and you can’t think clearly like you used to.
If this is how you describe your experience with COVID, you may be dealing with a condition called postural orthostatic tachycardia syndrome (POTS). Multiple studies show that long COVID can cause POTS.
POTS is a type of dysautonomia, which is a disorder of the autonomic nervous system (ANS). The ANS regulates functions we don't consciously control, such as blood pressure, heart rate, and body temperature.
It can be challenging to obtain a POTS diagnosis. Many doctors are not familiar with this condition and may dismiss these symptoms as just lingering effects of coronavirus disease or even psychological signs caused by stress and mental health problems.
However, POTS can be debilitating (or at least a hassle to deal with) and requires specific treatment to mitigate symptoms. At Cognitive FX, many of the patients we see developed POTS or some other form of autonomic dysfunction after suffering a concussion.
Typically, our patients find our clinic after suffering post-concussion symptoms for months or even years, including symptoms like dizziness, brain fog, and headaches. Some have been diagnosed with chronic fatigue syndrome (with no explanation of what could have caused it).
While we don't officially diagnose POTS or other forms of dysautonomia in our patients, the long list of associated symptoms is usually enough to recognize autonomic problems. For this reason, our treatment is purposely designed to treat the root of the problem — the ANS dysfunction — rather than addressing individual symptoms. You can read more about how our multidisciplinary treatment works later in the article.
Although Long COVID dysautonomia has been recognized as a medical condition, we still don't know much about this disease. This article tries to unveil as much as possible, including how long COVID can cause POTS and how our treatment program is designed to help COVID-19 patients.
We cover…
Our treatment program is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What is Dysautonomia?
Dysautonomia is a general term used to describe several medical conditions that share a common problem: the malfunction of a part of the nervous system called the autonomic nervous system (ANS).
The ANS regulates the automatic functions of the body that we don't need to think about, such as blood pressure, heart rate, digestion, breathing, body temperature, kidney and bladder function, and many others.
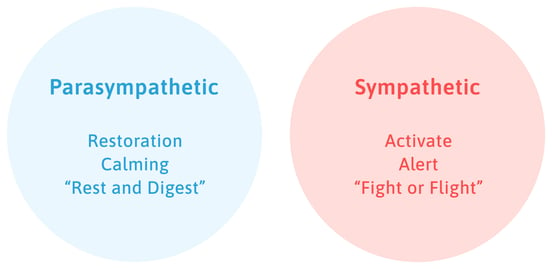
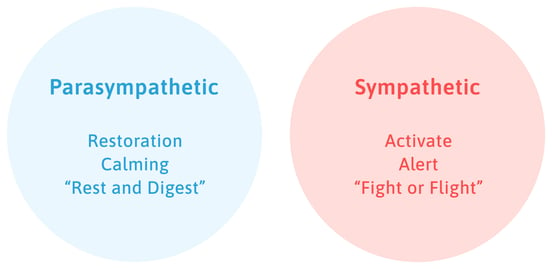
This branch of the nervous system has two components: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS is known as the "fight or flight" mode and is active whenever you need a fast reaction from your body. It increases heart rate and stimulates blood flow to the muscles when you need to escape danger or cope with stress.
In contrast, the PNS is responsible for calming functions in the body, such as digestion. It's known as the "rest and digest" part of the ANS. It lowers heart rate, stimulates digestion, and regulates bladder function.
In a healthy person, both components are in constant flux during the day. For example, the SNS may be more active when you have an important meeting at work, but then the PNS takes over when you have a cup of coffee to relax.
If one of these components stops working correctly, it can affect your entire body. Think of SNS and PNS dominance like a tug of war. Usually, the SNS is winning, but sometimes the PNS can yank back for a period of time before the SNS takes over again. That rapid switch from SNS dominance to PNS dominance and back again is why you could have a racing heart but then suddenly get diarrhea, for example.
People living with dysautonomia have difficulties regulating crucial body functions like breathing, blood pressure, heart rate, urinary function, body temperature, and more.
Is Dysautonomia the Same as POTS?
An explanation of POTS from Dysautonomia International.
Dysautonomia and POTS are not the same, but they are related: POTS (short for Postural Orthostatic Tachycardia Syndrome) is a form of dysautonomia in which patients experience an increase in heart rate when they stand up.
A similar disease is called Orthostatic Hypotension (OH). Instead of affecting heart rate, patients with OH experience a decrease in blood pressure when they reach an upright position.
Both of these conditions are grouped under the umbrella term orthostatic intolerance. The word orthostasis refers to the body's ability to stand upright. When you stand up, your body needs to adjust your heart rate and blood pressure to prevent blood from accumulating in your legs and to ensure enough blood reaches the brain.
If this doesn't happen, it may cause dizziness, lightheadedness, or even fainting. Typically, symptoms decrease when you sit down or lie down. If the symptoms start when you're already standing up, it cannot be classified as orthostatic intolerance.
Can Long COVID Cause POTS?

When COVID long haulers started reporting POTS-like symptoms such as lightheadedness, brain fog, dizziness, tiredness, and increased heart rate, the similarities with dysautonomia were so striking that doctors began testing for this condition.
Several studies have since confirmed that long COVID can lead to dysfunction of the autonomic nervous system, affecting almost two-thirds of long haulers. Postural orthostatic tachycardia syndrome (POTS) and orthostatic hypotension (OH) are the most likely types of ANS dysfunction diagnosed in these patients.
This relationship should not come as a surprise, as several other viruses, including human immunodeficiency virus (HIV), herpes viruses, flavivirus, and human T-lymphotropic virus can also cause ANS dysfunction.
How Does Long COVID Cause Dysautonomia?
Researchers don’t fully understand the reasons why long COVID often leads to dysautonomia. It is also unclear whether dysautonomia is more common in long COVID patients than in patients suffering dysautonomia with other origins, or whether any mechanisms are unique to long haulers.
At Cognitive FX, we suspect a slightly different mechanism (or set of mechanisms) may be at play in long haulers compared to our patients suffering from post-concussion syndrome. Although our PCS patients experience similar symptoms, we've noticed that long haulers tend to suffer more acutely from ANS dysfunction.
According to the latest research, COVID-19 illness causes ANS dysfunction through a combination of the following mechanisms:
- Direct effect: There is some emerging evidence that the SARS-CoV-2 virus can directly target components of the nervous system, including the ANS. Studies have shown that this virus can attack areas in the brain where the ACE2 receptor is found. This includes the brainstem, the hypothalamus, the pituitary gland, and the carotid body, all of which are involved in coordinating autonomic responses.
- Exaggerated response from your immune system: An uncontrolled cytokine storm — which is known to happen in long haulers — may also trigger an attack on the body’s autonomic nervous system.
- Neurovascular coupling dysfunction: Neurovascular coupling dysfunction — which we’ve demonstrated happens in long haulers — may cause ANS dysfunction by overactivating the sympathetic nervous system. No studies have been done in these patients, but some conditions, like hypertension, for example, are associated with a heightened activation of the sympathetic nervous system as a result of neurovascular coupling dysfunction.
- Stress due to the pandemic: Stress and worry put a person’s body in a constant state of high alert. If this situation is maintained for an extended period, there’s a high risk that the body cannot return to the rest and digest response, leading to dysautonomia.
- Long periods of bed rest: Prolonged periods of bed rest, especially for patients who spent several weeks in the hospital, can cause ANS dysfunction. A study showed that a rest period of only 3 weeks was enough to trigger some symptoms associated with dysautonomia in otherwise healthy patients.
Our treatment program is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
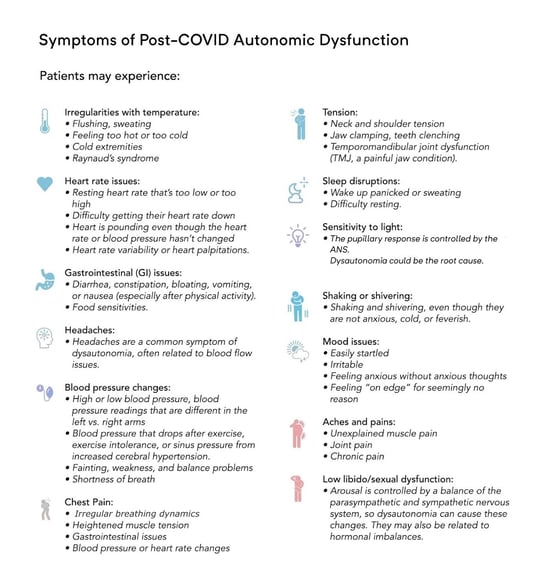
What are the Symptoms of Long COVID Dysautonomia?
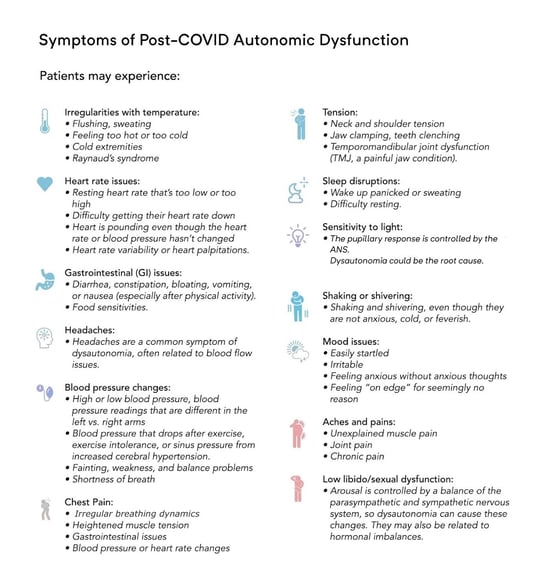
For some patients, symptoms are present all the time, while for others, they come and go in waves. Likewise, some COVID-19 symptoms tend to be more prevalent when you’re anxious or stressed, while others are noticeable even when you’re perfectly calm.
A few common symptoms of POTS or other autonomic disorders after COVID-19 include:
- Persistent fatigue (also known as post-viral fatigue or post-COVID fatigue)
- Low energy levels and low motivation
- Breathlessness and shortness of breath
- Lightheadedness with prolonged sitting or standing, which may lead to fainting
- Feeling dizzy when standing up
- Brain fog
- Trouble concentrating or remembering new information
- Exaggerated startle response and panic
- Heart palpitations or other beat abnormalities
- Chest discomfort
- Feeling like your heart is pounding
- Nausea
- Vomiting
- Headaches
- Excessive sweating
- Shaking
- Exercise intolerance
- General worsening of symptoms with increased activity
- Purple discoloration of the hands and feet (if the limbs are lower than the level of the heart)
- Erectile dysfunction
- Bladder problems
- GI issues and abdominal discomfort
- Sleep disturbance
- Pins and needles (peripheral neuropathy symptoms)
- Joint and muscle pain
Symptoms typically might worsen…
- In hot environments, such as a hot bath or shower, or on a warm day
- In situations where you need to stand for a long period of time, like waiting in a queue
- If you skipped a meal or haven’t had any food for a few hours
- If you’re recovering from a common cold or infection
Treating Long COVID Dysautonomia at Cognitive FX
As we've mentioned before, once we noticed how coronavirus affects the brain in a similar way to post-concussion syndrome (PCS), the primary condition we treat at our clinic, we adapted our treatment to offer a solution for COVID long haulers.
We've had very encouraging results so far. Most of our post-COVID-19 long haulers report significant improvements after treatment, including breathing easier, experiencing fewer headaches, and feeling less dizzy and lightheaded.
Treatment starts with a functional neurocognitive imaging (fNCI) scan for all patients. This measures how this viral infection has disrupted the connection between nerve cells and the blood vessels that supply them with oxygen and nutrients. This disruption is called neurovascular coupling (NVC) dysfunction.

Ultimately, our treatment aims to restore normal neurovascular coupling in the areas highlighted as dysfunctional by the scan.
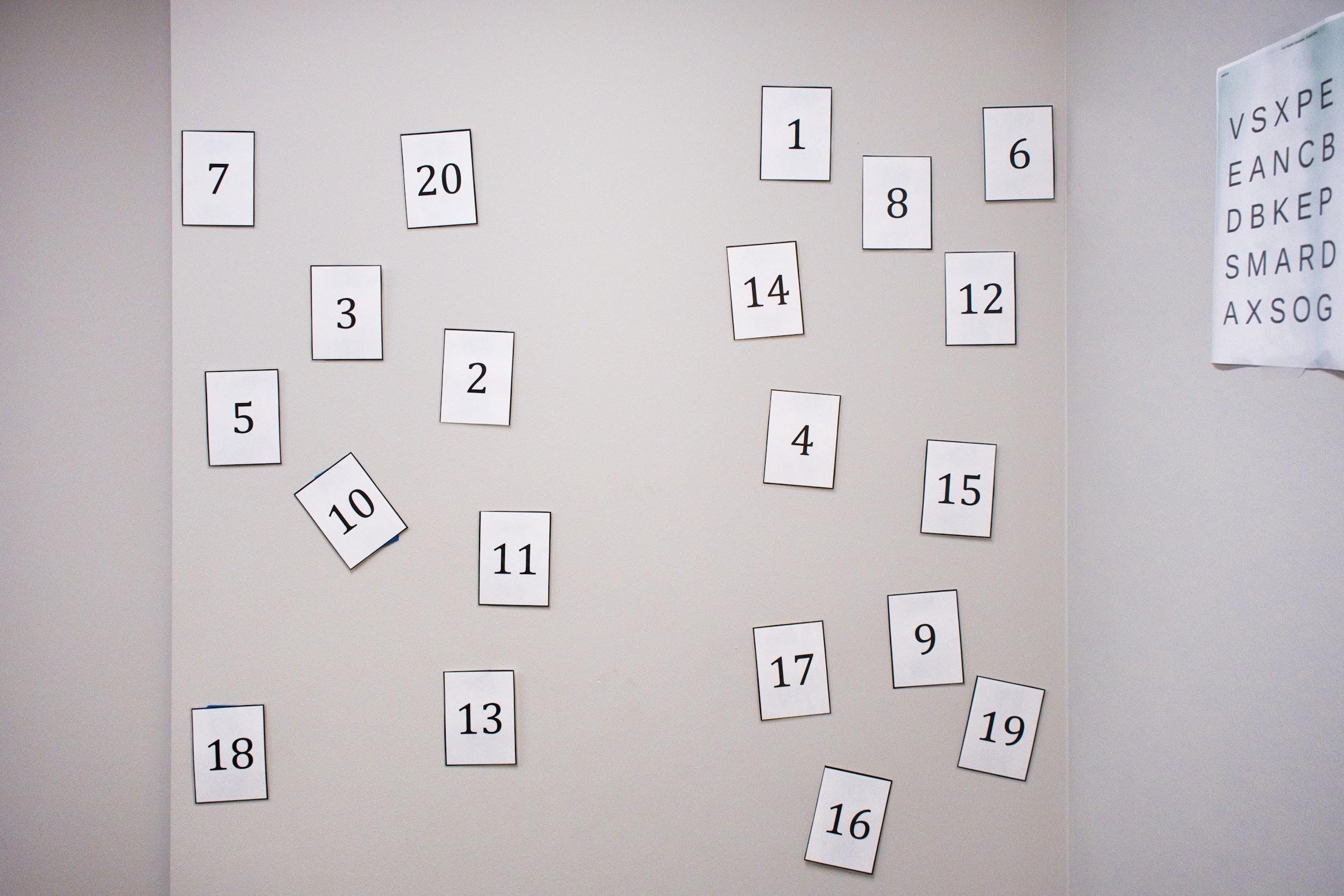
To achieve this, our patients undergo a period of treatment known as EPIC — short for Enhanced Performance in Cognition — which involves a series of physical and cognitive exercises combined with periods of rest.
In addition to treating NVC dysfunction, alternating between aerobic exercise and rest helps re-regulate the autonomic nervous system.
In long COVID patients, the sympathetic nervous system often stays dominant, overshadowing any involvement of the parasympathetic branch. To combat sympathetic nervous system dominance, patients complete a series of short intervals of aerobic exercise accompanied by rest periods.
Aspects of treatment that directly target the autonomic nervous system include:
- Aerobic exercise: This can be done on a stationary bike or treadmill. Our therapists monitor how patients react in these sessions and adjust the duration and intensity of each activity as needed. For example, if you feel dizzy and lightheaded while on the treadmill — a sure sign that your sympathetic nervous system is still dominant — our therapist may recommend using a stationary bike instead for safety reasons.
- Periods of rest: This includes breathing exercises, mindfulness meditation, and Brainwaves sessions to promote activation of the parasympathetic nervous system and to help you relax. For example, we use a 4-6-1 breathing pattern: Breathe in for four seconds, breathe out for six seconds, hold for one second, and repeat. When needed, we assign different breathing exercises. Brainwaves use a combination of frequencies to help your brain achieve a state similar to meditation. This helps it calm down after therapy sessions or when you’re feeling overwhelmed.
- Neuromuscular massage: This is a specialized form of physical therapy where the therapist targets soft tissue. Many of our patients report painful and stiff neck muscles, which often leads to severe headaches. Neuromuscular therapy helps patients relax and find some relief from neck pain by switching “off” the sympathetic nervous system and turning “on” the parasympathetic nervous system.

Treatment also includes a series of different therapies, including cognitive therapy, sensorimotor therapy, and neurointegration therapy, to name just a few.
The aim is to promote the brain's ability to heal and restore healthy neurovascular coupling, which in turn reduces the incidence and intensity of long-term symptoms caused by the coronavirus infection (including those caused by dysautonomia).
Patients undergo a second fNCI to see how their brain improved during their EPIC treatment. They also receive a series of exercises to do at home to continue their journey to recovery.
Note: COVID-19 POTS may require the assistance of more than one healthcare provider. Specialists in cardiology, neurology, gastroenterology, or even immunology might be a necessary ‘piece of the puzzle’ to help you make a full recovery. This is because COVID might cause direct damage to some of your body’s systems which can’t be addressed through therapy. Because of this, we screen all potential patients carefully before accepting them. We want to ensure that you’ll receive as much benefit as possible when you visit our clinic.
How to Manage Long-Haul COVID Dysautonomia at Home

Many lifestyle adaptations can help long haulers cope with long-term effects and other health issues caused by their dysautonomia. It's important to note that each patient is different, and these suggestions will not suit everyone. If in doubt, consult your doctor before making any changes to your daily routine. Your physician may also recommend medication such as fludrocortisone if therapy and lifestyle changes are insufficient.
Counter Maneuvers
If you experience lightheadedness and vertigo, try tensing your leg muscles or crossing your legs while standing. This has been shown to reduce symptoms, increase oxygenation to the brain, and reduce sympathetic activity.
Exercise Regularly
We recommend a structured exercise program including aerobic and resistance elements. If you find that standing up for extended periods is problematic, try using an exercise bike or a rowing machine.
Increase Fluid and Salt Intake
Most patients with POTS benefit from an increase in both fluid and salt intake. This is particularly useful for patients with low blood pressure. The typical recommendation is 3-5 grams of salt and 2-3 liters of water per day.
If you need to increase your intake, change it gradually over the course of a few days. This may not suit all patients, especially if they have other medical conditions or take medication that may alter blood pressure. It's essential to check with your doctor or a healthcare professional before making any dietary changes.
If you find that your symptoms are worse in the morning, it helps to start the day with a large glass of water.
Humming, Singing or Gargling

Humming, singing, or gargling is an effective way to stimulate the parasympathetic nervous system. These activities stimulate your vocal cords, which in turn activate the vagus nerve. As part of the parasympathetic nervous system, the vagus nerve can help to counterbalance the “fight or flight” mechanism and relax your body.
Eat Smaller Meals
Eating a large meal redirects a large amount of blood to aid in the digestion process. In POTS patients, this may trigger or aggravate symptoms.
Eat several smaller meals throughout the day instead of three large ones. Also, avoid excessive alcohol and caffeine.
Elevate Your Head During Sleep
Dysautonomia patients should sleep with their head slightly elevated in order to stimulate blood circulation. Don't just put a few extra pillows under your head (this will only put strain on your neck): raise the top of the bed by about 4-6 inches to place the entire body at an angle.
Use Compression Garments
Compression stockings and abdominal binders can be helpful for some patients to stimulate blood circulation and increase blood pressure.
Studies suggest you need to compress all lower body parts, including the calf, thigh, and low abdomen. Compressing just the leg is not as effective, presumably because it's not enough to affect blood pressure.
Maintain an Even Temperature
It is crucial for POTS patients to maintain an even temperature as extremes, particularly heat, can make symptoms worse. At home, you can set your air conditioning to a comfortable temperature. When you're not at home, handheld fans and spray bottles with water work well for keeping your face cool. Placing a wet towel around your neck can also help you cope better with your daily activities.
Avoid Standing for Long Periods
Most patients with dysautonomia struggle to stay standing for long periods. If you need to stand for a long time, try to squeeze your feet and legs every couple of minutes, or shift your weight from one foot to the other. The idea is to keep moving your lower half of the body as much as possible to improve circulation and help your heart pump blood.
Find Out What Triggers Your Symptoms
Every patient is different, and various situations can trigger symptoms. Keep track of what your triggers are, so you can avoid them if possible or at least plan your activity levels.
Our treatment program is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.







%20(9).png?height=175&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(9).png)