Can’t Sleep After COVID? How to Treat COVID Insomnia (2026)
You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
At the moment, treatment options for long COVID patients are limited. Many patients cope with their symptoms using existing medications or treatments targeting specific symptoms like headaches or sleep problems, but these efforts are just stopgaps. They don’t actually resolve the underlying cause of symptoms associated with long COVID. Researchers know there is a growing need to identify new and effective treatments for these patients.
One of the options currently under assessment is called hyperbaric oxygen therapy (HBOT), where patients breathe high oxygen concentrations for short periods of time.
Using HBOT during acute COVID infection delivers extra oxygen to the brain, which seems to alleviate many of COVID’s cognitive and physical symptoms. However, HBOT may not continue to be beneficial for long COVID patients. Be cautious about using HBOT as a COVID long-hauler; research in this field is still very limited. It’s important to compare it with other treatment options available to you and to evaluate whether it is worth the cost.
In this article, we look at the research studies and clinical trials assessing HBOT for COVID patients and long-haulers, as well as the current limitations for this procedure. We include…
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.

Hyperbaric oxygen therapy has been around for decades. In most applications, it involves stepping into a hyperbaric oxygen chamber and breathing pure oxygen in air pressure up to three times that of our atmosphere.
This procedure was originally developed to treat decompression illness in deep-sea divers (colloquially known as “the bends”). Decompression illness occurs when divers reach the surface too quickly and air bubbles expand in their bloodstream. HBOT “returns” the patient to the pressure (or, in other words, the depth) at which they were diving and then allows for a gradual return to normal values, slowly reducing the volume of the air bubbles.
Its use has since expanded to address other conditions. At the moment, FDA-approved uses for HBOT include the following:
Some researchers and physicians offer HBOT for conditions that the FDA has not approved. Off-label HBOT is sometimes offered for HIV/AIDs, migraines, cerebral palsy, traumatic brain injury, heart disease, stroke, asthma, depression, spinal cord injury, sports injuries, and Alzheimer’s disease.

Initial medical interventions for COVID patients focused on treating breathing problems and the inflammatory response to the SARS-CoV-2 virus. But for many patients with a severe COVID-19 infection, these interventions were not enough. In many hospitals, doctors were using ventilators at the highest settings possible but were still not achieving adequate blood oxygenation for many patients. Worryingly, oxygen saturation levels in the blood below 90% were associated with high mortality.
At this stage, doctors with experience in using hyperbaric chambers for other conditions started wondering whether HBOT could be used to treat hypoxic COVID patients. Soon, some clinics and hospitals started treating patients in the hope of overcoming their hypoxia and reducing the need for intubation.
One of the first reported uses of HBOT in COVID patients was published back in May 2020. In this study, patients with severe cases of COVID received HBOT instead of mechanical ventilation. After only five sessions in a chamber, the patients experienced significant improvements in their breathing. Although the study included only five participants, the researchers involved in this work believed the results warranted further investigation.
Since then, there have been multiple studies with more participants looking at the efficacy of HBOT in COVID-19 treatment, with particular emphasis on patients with severe cases and those who needed mechanical ventilation. Taken overall, these studies show that HBOT can:
In addition, there are several clinical trials testing different HBOT regimes currently underway in the U.S. and around the world. This includes, for example, a large multicenter trial enrolling participants in four major medical centers to evaluate the effectiveness of HBOT for treating patients with moderate to severe respiratory distress due to the coronavirus (ClinicalTrials.gov Number: NCT04619719).
For over five decades, doctors have used HBOT to treat a variety of conditions. This technique is safe for patients, with few contraindications and side effects. As such, HBOT is becoming an attractive alternative to other oxygen delivery methods, such as ventilation, particularly in severe COVID cases. Patients in HBOT chambers can breathe normally, avoiding invasive mechanical ventilation, which could cause serious side effects.
There is also some evidence that HBOT has anti-inflammatory and anti-viral properties, and many doctors believe this technique should be considered a valuable tool in managing some patients with COVID-19. However, more research is needed to fully understand how patients can benefit from this technique.

One of the first reported uses of HBOT to manage long haul COVID found promising results: Patients experienced improvements in fatigue and cognitive function, some of the most common symptoms associated with long COVID. The authors suggested HBOT helped reduce inflammation and promoted healing by increasing the amount of oxygen reaching the tissues.
More recently, a team of researchers published a new study suggesting that there’s more to HBOT than just increased oxygen flow. In these studies, the authors used MRI scans before and after treatment to detect whether a period in a hyperbaric chamber can actually change the brain of long COVID patients.
Analysis of these scans revealed significant changes in several parts of the brain, which matched how symptoms improved for the patients after treatment. COVID long-haulers reported less pain and fatigue, as well as better cognitive skills, such as attention, memory, processing information, and executive functions. Patients also slept better and had fewer psychiatric symptoms. For example, the scans detected improvements in a zone of the brain called posterior corona radiata, which explains the less severe symptoms of depression and anxiety after only a few sessions.
The authors suggested hyperbaric oxygen treatment promotes a mechanism in the brain called neuroplasticity, a process where the brain creates and reorganizes nerve cell connections after injury. In other words, HBOT led to significant changes in parts of the brain, which in turn resulted in improved function in the areas damaged by the COVID-19 virus.
HBOT may help these patients thanks to the hyperoxic-hypoxic paradox. In simple terms, inhaling massive amounts of oxygen for a short period and then breathing normal amounts afterward “tricks” the body into thinking it’s being deprived of oxygen.
When our body detects a drop in oxygen levels, it triggers certain metabolic changes to help protect our internal organs. This includes, among others, a boost in the immune system, increased breathing rates, and improved blood flow to all organs. It also reduces neuroinflammation and induces neurogenesis (formation of new nerve cells in the brain). For the authors, some or all of these mechanisms may explain the beneficial effects of HBOT in long COVID patients.

A growing number of providers are now offering HBOT as an alternative therapy to treat long COVID patients. It has even been branded a “miracle cure,” with hyperbaric chambers appearing in various locations throughout the country.
However, is HBOT a good option for treating post-COVID-19 syndrome? We believe it may be helpful for patients who have very specific causes of long-term COVID symptoms and may also be helpful for short-term symptom relief. But for most patients, we can’t recommend it due to the:
Once we’ve explained our reasoning, we’ll discuss the next key question, which is whether HBOT is more helpful for most patients than a readily available alternative: cardio exercise.
While early results are important and point to some possible benefit to patients suffering from long COVID, they represent an initial evaluation. There have been only a few recent studies with a limited number of participants. In addition, these patients participated in short-term clinical trials. The researchers have not published data to show whether the reported improvements are maintained or disappear over time.
In our view, the initial results suggest that HBOT merits further research with larger and more rigorously designed studies. The technique has not been tested enough to be reliably used to treat long-haulers.
At the moment, many clinics charge tens of thousands of dollars to provide HBOT to long COVID patients. Some researchers believe the price barrier will eventually disappear if the technique works, but others aren’t convinced.
At Cognitive FX, we believe there are better options for the expense. For example, several types of therapy (such as physical therapy for long COVID) have produced good results and are less expensive.
You can learn more about our long COVID treatment program below.
Furthermore, each provider will offer their own “recipe” in terms of the type of chamber used, pressure during treatment, duration, number of sessions, and other factors.
This approach makes it very difficult to determine whether a certain provider’s treatment method is effective. And in some cases, it may even render the HBOT useless. For example, some providers use “soft” or “mild” chambers, which typically cannot reach pressures higher than 1.4 atmospheres and, therefore, cannot provide reliable treatment.
First, long COVID can have many causes. In some patients, long COVID may be caused when COVID reactivates dormant viruses. In others, it may come from autoimmune issues. In most patients, poor neurovascular coupling (discussed in detail in the next section) is a key contributor to symptoms. In these situations, HBOT is likely not a long-term solution.
Studies have also not differentiated between patients who are recovering from severe COVID infections versus those who had only a mild case. Overall, there simply have not been enough clinical trials on long COVID patients to clearly determine which patients are likely to benefit from this treatment and which patients are not.
Second, HBOT is not suitable for everyone. Patients with a cold, fever, and certain lung, ear, and eye conditions cannot safely receive HBOT.
The FDA has approved HBOT for a variety of conditions, but at the moment, they have not authorized the use of hyperbaric chambers to treat COVID-19.
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.

Researchers have proposed that HBOT is helpful because it boosts oxygen in the brain. But there are two main issues with this hypothesis.
First, extra oxygen in the brain is not necessarily beneficial for these patients. In many long COVID patients, a shortage of oxygen in the brain is not the problem. The problem is the brain’s ability to use that oxygen and other micronutrients efficiently when and where they’re needed.
In a healthy brain, a network of blood vessels transports oxygen and nutrients, delivering them to specific regions of the brain as needed. This partnership between blood vessels and neurons is called neurovascular coupling (NVC).
In most long COVID patients, NVC is disrupted. The delicate balance of communication between blood vessels and the neurons they supply doesn’t function correctly. While the associated brain tissues remain alive, they can’t always carry out their necessary functions. Flooding the brain with oxygen does not help the brain operate better over time if healthy NVC is not restored.
Think of it like a car that’s supposed to be getting 40 mpg but is instead only getting 10 mpg. If you keep filling up the gas tank (in this example, analogous to HBOT), then you can force the car to run. But it’s not doing so efficiently, and you haven’t repaired the actual problem.
At Cognitive FX, we lead our patients through cardiovascular exercise to prepare the brain for therapy. Many people think that the increased blood flow to the brain is why exercise helps the brain recover from injury, but in many cases, patients actually have too much oxygen in their brains and aren’t able to use it properly due to poor NVC.
In reality, exercise is beneficial for two reasons:
Aerobic exercise triggers the release of chemicals such as brain-derived neurotrophic factor (BDNF), which improve the brain’s ability to respond to therapy.
Cerebral autoregulation is the system which controls how much blood flows into the brain. When a long COVID patient or someone else with a brain injury engages in exercise and their heart rate and blood pressure rise, too much oxygen is released into the brain. The brain stem flags this as an error and will attempt to adjust accordingly.
With repeated exercise (done safely under the supervision of trained therapists), the brain is more likely to regulate blood flow in a healthy manner. This contributes to the patient’s overall recovery.
With that in mind, there’s a notable difference between the effect of HBOT — which only increases the oxygen concentration in the brain — and exercise, which promotes healthy release of neurochemicals and teaches the body to regulate blood flow in a healthier manner.

Since the pandemic started, we’ve treated many COVID long-haulers at our clinic. Our patients experience significant improvements after treatment, although some symptoms improve faster than others.
Before treatment starts, all patients undergo a functional NeuroCognitive Imaging (fNCI) scan. This brain imaging scan assesses function in 56 regions of the brain while the patient completes a series of cognitive tasks. The scan also allows us to evaluate the health of connections between these regions. In addition to the scan, patients complete a series of physical, visual, and cognitive tests.
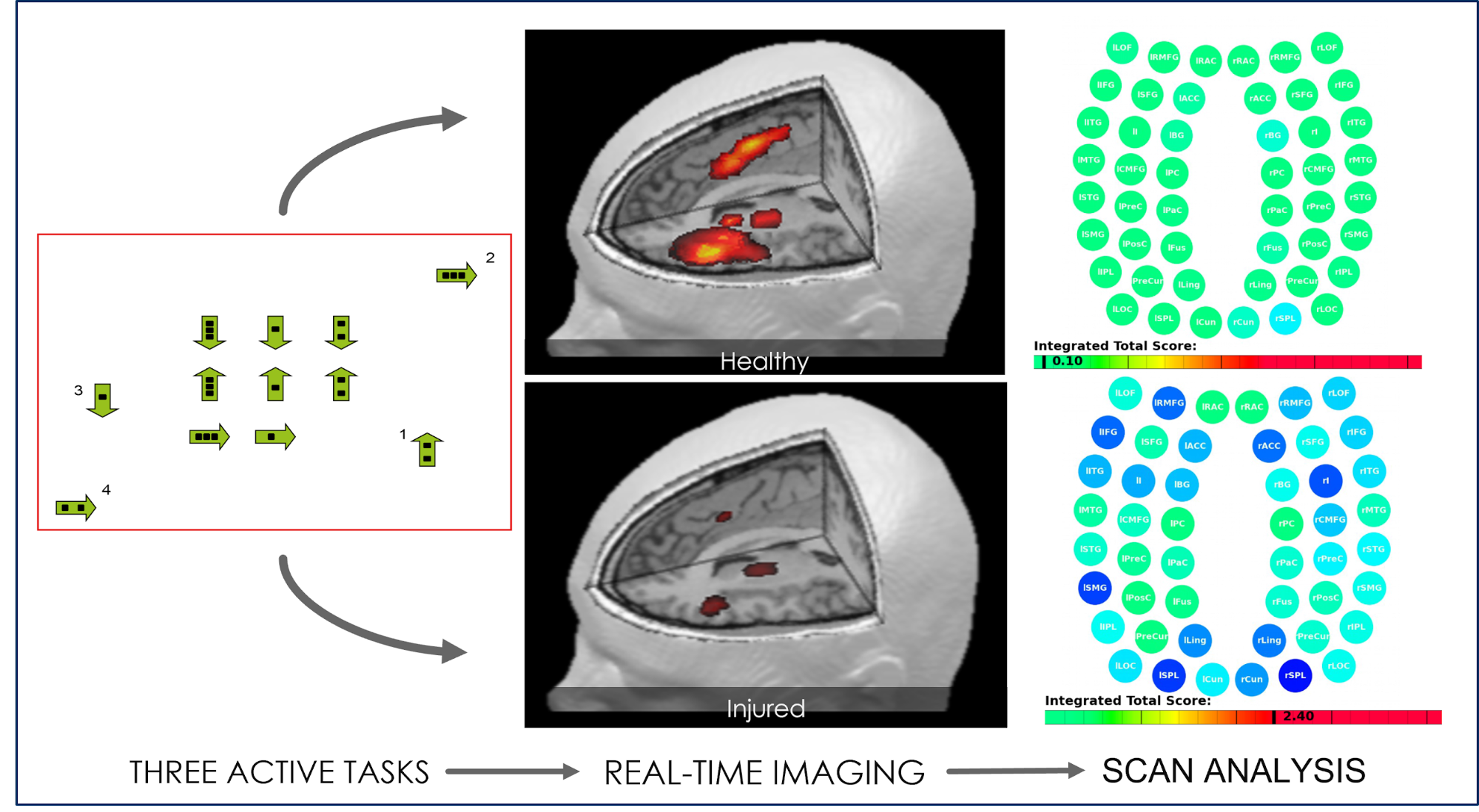
All of these results are then combined and used to design a custom treatment plan. During treatment, patients cycle repeatedly through three stages: Prepare, Activate, and Recover.

At the end of treatment, patients undergo a second scan to monitor improvement. Patients also meet with our team to get their final assessment, a list of exercises to do at home, and referrals for any follow-up treatment.
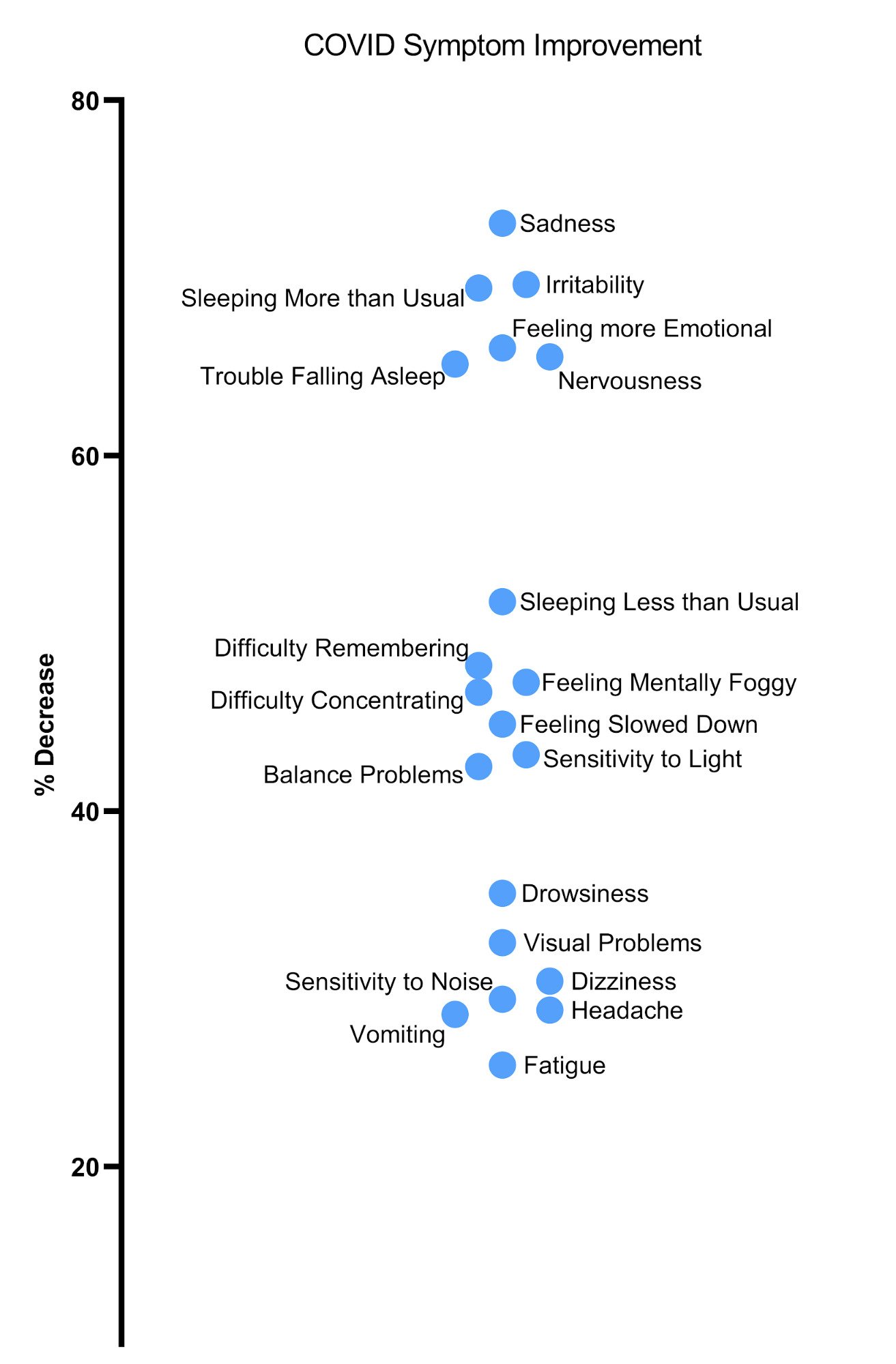
In the chart above, you can see average symptom decrease based on 47 patients at the end of one treatment week. Some symptoms, such as fatigue, improve more when the patient has time to rest at home. Therapy is hard work! Patients who continue their therapy assignments at home typically show continued improvement.

You can learn more about what it’s like to receive treatment for COVID-19 at Cognitive FX by reading about three members of the Sharp family. They were some of the earliest patients in the U.S. to contract COVID and suffered from long-term symptoms for over a year before finding our treatment center. The family’s matron, Sarah Sharp, noticed a difference after just one day.
“I woke up, and I felt a mental clarity like I could see for the first time in 20 months. It's like getting glasses for the first time,” she said. “I could think clearly. I know it sounds weird to say that just after one day, but that's what it was. It turned my brain on.”
Both she, her daughter, and her son all experienced a significant improvement in their quality of life after treatment.
To learn more about the symptoms of long COVID and treatment options, see these posts:
To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.

Most patients with COVID-19 recover within a few days or weeks after a brief acute infection. However,about 10%experience long-term symptoms such as brain fog, fatigue, headaches, shortness of...

If you're reading this, you've probably tried everything for the headaches that won't quit since your COVID infection. Maybe it's been three months. Maybe it's been two years. You've likely cycled...
Your heart races when you stand. You hate the dizzy spells. Your head hurts, you’re exhausted, and you can’t think clearly like you used to.

Even after you've recovered from the acute symptoms of COVID-19, you might find yourself struggling with short-term memory loss, concentration issues, and other cognitive symptoms. If it's been weeks...

When the pandemic started, we were told that children wouldn’t be seriously affected by the virus. And while most children only experience a mild version of the disease, evidence shows that some...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY