What is EPIC Concussion Treatment? | Cognitive FX
By Mark Allen, Director of Research
The Enhanced Performance in Cognition - EPIC concussion treatment provided at Cognitive FX is a highly effective approach to concussion rehabilitation. We have...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Most patients with COVID-19 recover within a few days or weeks after a brief acute infection. However, about 10% experience long-term symptoms such as brain fog, fatigue, headaches, shortness of breath, and even psychological issues like depression and anxiety. Experiencing these persistent symptoms is known as long COVID, long-haul COVID or post-acute sequelae of SARS-Cov-2 infection (PASC).
Treating long COVID is complex; different patients may suffer different complications, so there is no one accepted protocol to treat long-haul COVID. Some patients try to find specialists to treat the symptoms that are causing the most trouble. Others resort to untested or unproven treatments, such as hyperbaric oxygen therapy for long COVID.
At Cognitive FX, we evaluate long-haul COVID patients and offer personalized treatment based on the results. We start by determining exactly how long COVID has affected blood flow in your brain using state-of-the-art brain imaging techniques. Then, we design a tailor-made protocol to address what we find. To deliver this treatment, we rely on a multidisciplinary team to give our patients the best possible care.
That said, our long-haul COVID treatment protocol has elements in common from patient to patient. Most of the therapies we use are helpful for all patients, but the way we administer them is where the tailored treatment experience comes in.
In this article, we’ll explain:
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.
The term “long COVID” is used to describe ongoing COVID-19 symptoms in people more than four weeks after their original infection. An estimated 65 million patients around the world have long COVID, but the number is likely much higher due to many undocumented cases since the pandemic began. Many of these patients experience COVID-19 symptoms that affect multiple organs at once, leading to problems in several body systems and lowering quality of life.
Neurological and Cognitive Symptoms
Neurological and cognitive symptoms are some of the most common symptoms of long COVID. These symptoms can linger for weeks or months after the initial COVID-19 infection. They include:
Respiratory Symptoms
Post-COVID syndrome can cause respiratory problems, including:
Gastrointestinal Symptoms
COVID long-haulers often experience a wide range of symptoms, including:
Cardiovascular Symptoms
Long COVID can also trigger cardiovascular symptoms and cause long-term heart damage. These include:
Mental Health Symptoms
COVID long-haulers can experience a wide range of psychological problems. These issues may develop from the virus itself or from the stress of living with long-term symptoms. Mental health effects of long COVID include:
.jpg?width=1000&height=550&name=long-haul-covid-treatment-protocol%20(4).jpg)
There are multiple, potentially overlapping causes of long COVID. Research into long-term effects of COVID is still ongoing, and new evidence is coming to light every week. Some causes may include the following:
In a healthy brain, nerve cells receive oxygen and nutrients from a network of blood vessels in response to need. This dynamic mechanism, called neurovascular coupling (NVC), allows neurons to “order” what they need and have it delivered at the right time and to the right location.
In COVID long-haulers, this connection is disrupted in some areas of the brain. As a result, affected areas can’t function as normal, causing many of the physical and cognitive symptoms experienced by these patients, such as sleep problems, feelings of overwhelm, memory issues, brain fog, vision and vestibular problems, and more.
Read more about how NVC dysfunction was linked to long COVID symptoms.
Dysfunction of the autonomic nervous system (ANS) is also recognized as an important feature of long COVID-19.
Our attention is focused on two sections of the ANS that can be affected after the coronavirus infection: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS represents your “fight or flight” response, and it can make changes such as increasing your heart rate, stimulating blood flow to your muscles, and increasing muscle tension.
In contrast, the PNS is your “rest and digest” system, and it lowers heart rate, regulates digestion and bladder function, and slows down breathing rates. Under normal circumstances, the PNS and SNS switch control back and forth throughout the day to meet your body’s needs at the time.
But for many long COVID patients, the healthy balance between PNS and SNS is replaced with dominance of only one of the branches. Typically, the SNS becomes dominant over the PNS. This leads to a variety of symptoms throughout the body, including abnormal heart rate, fatigue, shortness of breath, and headaches.
Further reading: COVID can cause dysautonomia

It’s also common for long COVID patients to develop vision and/or vestibular issues. When it comes to vision issues, patients may complain of dry eyes, redness, itching, blurry vision, and sensitivity to light. Vestibular symptoms include dizziness, vertigo, lightheadedness, spatial disorientation, and sleep disturbances, among others.
COVID-19 can cause vision and vestibular issues in multiple ways, including direct viral infection, severe inflammation, or blood clotting that could restrict the blood supply to the eyes or in the inner ear (where the vestibular system is located). Any of these can lead to damage and cause long-term vision and vestibular complaints.
Further reading: Vision problems and COVID
Dysfunctional breathing can cause hyperventilation, irregular breathing patterns, shortness of breath (dyspnea), irregular heart rhythm, and impaired physical stamina in patients with long COVID. Altered breathing dynamics may trigger the SNS, forcing its dominance over PNS. Many patients get trapped in a cycle in which altered breathing dynamics make their ANS dysfunction worse, and then ANS dysfunction aggravates their breathing problems.
Further reading: Breathing problems after COVID-19
Microclots: The SARS-CoV-2 virus can also affect the vascular (blood flow) and coagulation (blood clotting) systems. Some studies show that the virus leads to the formation of blood clots which the body doesn’t seem to be able to break down, forcing these microclots to stay in the bloodstream. Researchers theorize that these microclots accumulate and block the supply of oxygen and nutrients to different parts of the body. In turn, this may cause symptoms such as headaches, brain fog, and fatigue.
Vagus nerve damage: Long COVID may be the consequence of damage to the vagus nerve. This nerve connects the brain to the heart, lungs, and intestines and plays a key role in many bodily functions, including heart rate, speech, the gag reflex, sweating, and digestion. Patients with vagus nerve issues can experience difficulties swallowing, dizziness, a high heart rate, low blood pressure, dizziness, and balance issues, among other symptoms.
Generalized inflammation: During a COVID infection, inflammation is a normal response from the immune system and usually only lasts a few days. In some COVID-19 patients, however, the immune response goes too far and triggers a generalized inflammatory response throughout the body. This inflammatory response may trigger ANS dysfunction, which could perpetuate inflammation throughout the body and cause many post-COVID symptoms.
Hidden virus: There is now evidence that the SARS-CoV-2 virus can reach everywhere in the body and that it stays longer than previously expected. Some studies suggest that the virus can hide in different tissues, leading to long-term COVID symptoms such as fatigue, chest pain, brain fog, and more.
.jpg?width=1905&height=1160&name=long-haul-covid-treatment-protocol%20(7).jpg)
Long COVID is difficult to treat, and treatment options are limited, partly because the disease takes so many different forms and has so many potential causes. One patient may experience fatigue and brain fog, while another develops gastrointestinal issues or mental health problems. One patient’s headaches may stem from neurovascular coupling dysfunction, while another’s stems from breathing dysfunction.
For this reason, most attempts to treat long COVID have focused on specific symptoms rather than finding one single approach. For example, some doctors and other health care providers are using treatments similar to the ones used for patients with myalgic encephalomyelitis/chronic fatigue syndrome. The rationale behind this is that both conditions share many symptoms, including extreme fatigue and crashes after exertion, so a similar treatment plan may help COVID patients.
Researchers and clinicians have also found promising signs that certain drugs used for other conditions may reduce the chances of developing long COVID and ease symptoms among patients who already have the condition. There are ongoing clinical trials testing, for example, antihistamines, diabetes medication, and some antivirals.
The problem is that most primary care services don’t offer a consistent approach to treating long COVID. In frustration, long-haulers have turned to a vast range of over-the-counter medicines, remedies, supplements, therapies, and dietary changes to manage lingering symptoms.
Unfortunately, there’s little scientific evidence to show that these remedies work. There are also serious risks associated with self-prescription, including using products off-label in unsafe doses. What’s more, harmful drugs/drug interactions can further aggravate or add to symptoms of post-acute COVID-19.
Fortunately, certain types of therapy — a non-pharmacological long COVID intervention — can significantly improve symptoms. At Cognitive FX, we take a multidisciplinary therapy approach to treatment.

Instead of attempting to treat individual symptoms one at a time, we follow a different approach. We treat long COVID holistically using a combination of physical exercise and therapy.
Our protocol includes the following:
Here are some more details about each stage of the patient journey at Cognitive FX.
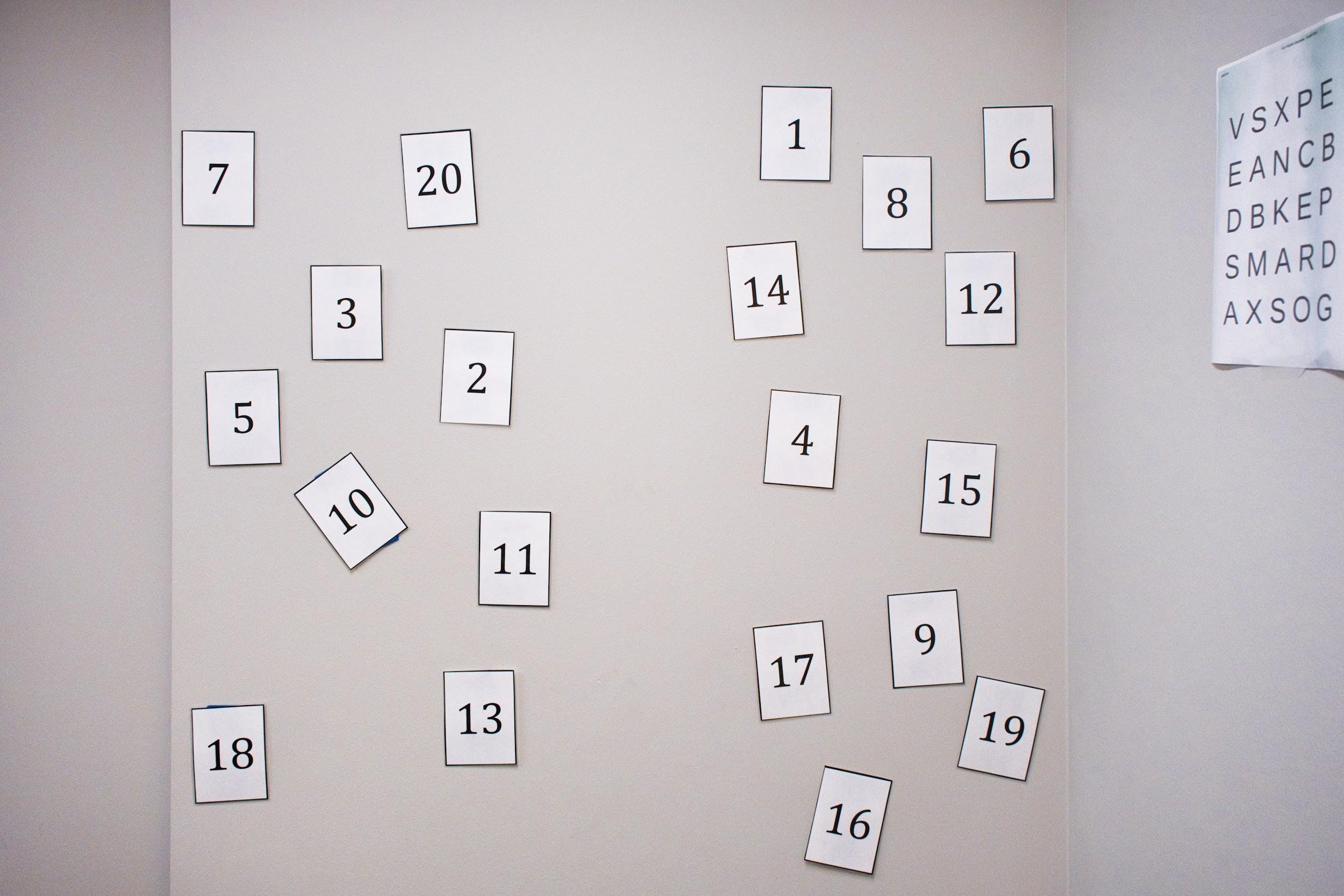
At Cognitive FX, we use a variety of tests to assess how long COVID has affected our patients’ lives. During this process, we will ask you about your symptoms and medical history.
This assessment also includes a:
Each patient undergoes a functional MRI designed to determine how and where the virus affected their brain. This brain imaging scan is called functional NeuroCognitive Imaging (fNCI). The fNCI scan assesses how well neurons are functioning in about 100 regions in the brain and how those regions communicate with each other while the patient performs a series of standardized cognitive tasks.
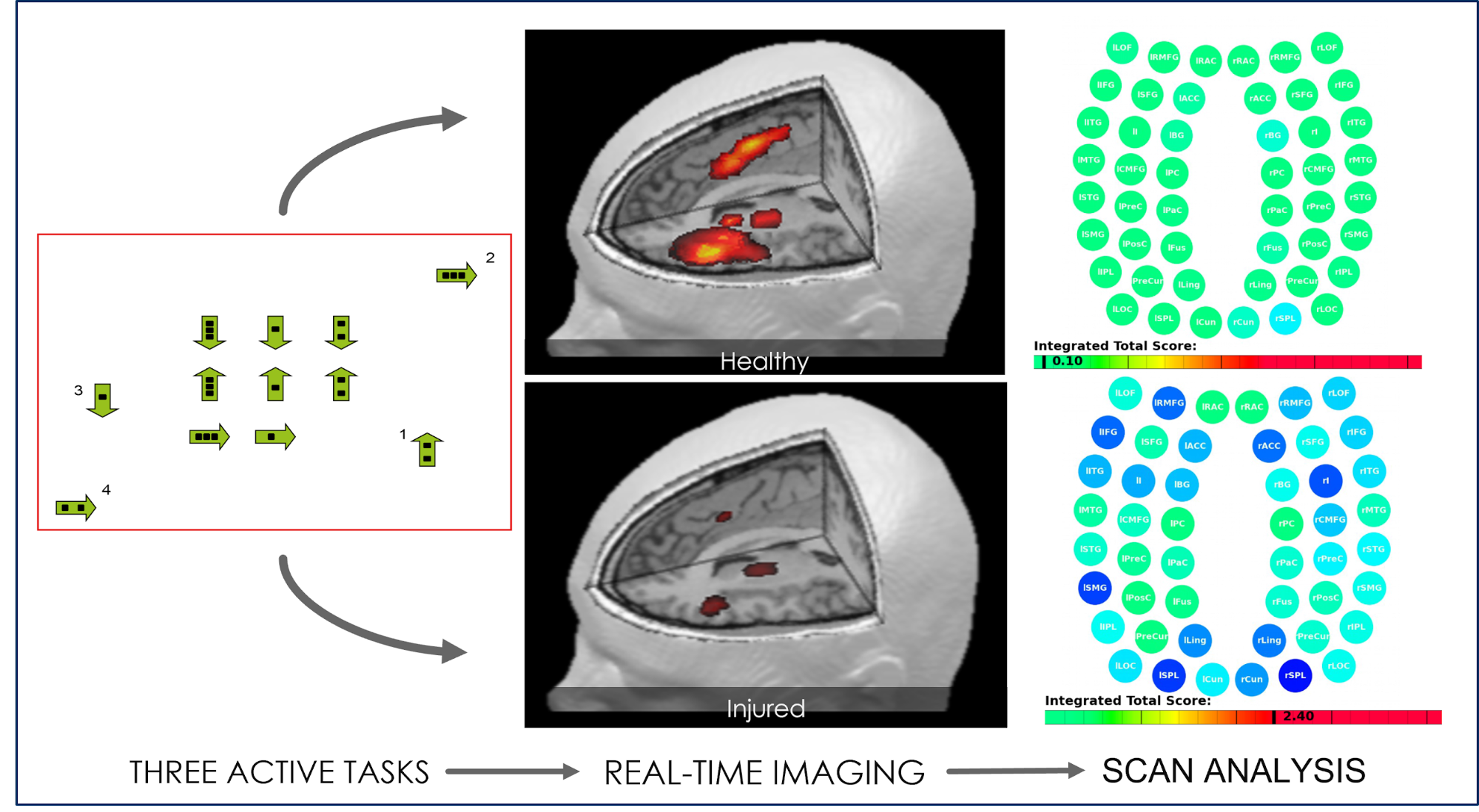
With the information gathered during the initial medical examination and the results from the scan, our therapists can then design our therapy protocol to target the areas of your brain that were most impacted by COVID-19.

To treat COVID long-haulers, our therapists use a combination of aerobic exercise and multidisciplinary therapies to take advantage of a mechanism in the brain called the post-exercise cognitive boost (PECB). Exercise triggers the release of neurochemicals, including a compound called brain-derived neurotrophic factor (BDNF). BDNF promotes the growth of brain cells and improves communication between different areas of the brain, which in turn makes the patient’s brain more flexible and able to benefit more from subsequent therapy.
Therapies used during treatment include:
Most patients receive all or most of these therapies during their visit. We use fNCI and other test results to inform the selection of specific exercises within each therapy discipline. So while our overall protocol has the same therapies, the exact regimen each patient receives is unique to them.
In addition, these therapies are administered in quick succession, sometimes even in combination with each other. For example, you may be asked to balance on a Bosu ball while tossing color-coordinated tennis balls back and forth and naming an animal for each letter of the alphabet. This pushes your brain to activate areas involved in balance, hand-eye coordination, and word recall at the same time, encouraging the restoration of healthy neurovascular coupling.
.jpg?width=1999&height=1333&name=long-haul-covid-treatment-protocol%20(11).jpg)
Many COVID long-haulers experience trouble breathing or swallowing, have vision or vestibular issues, or struggle with neck pain and sensitivity. Often, these issues are related to dysfunction in the brainstem, which is located at the base of the brain on top of the spinal cord. This area plays a key role in regulating certain actions of the body, including heartbeat, breathing, and balance. Combining different exercises to target two or more of these symptoms can be very helpful for COVID long-haulers. For example, you might perform tongue exercises while moving the neck to help with swallowing and neck pain.
Throughout the day, patients have multiple opportunities to rest and relax so their brains can recover. Rest periods may include a neuromuscular massage to the neck and shoulders, mindfulness meditations, or sitting in a dark room listening to binaural beats (which encourage relaxation and decrease anxiety).
The safety of our patients is paramount to us, and all patients are closely monitored during therapy. Our therapists are trained and know how much to push each patient and can adapt the activities to individual needs. The aim is to offer different exercises to rapidly recondition a patient’s brain without triggering a debilitating crash.
While some of our patients need just one week of therapy, our long COVID patients often experience the best results after two weeks. Patients with symptoms such as headaches, vision and vestibular issues, and ANS dysfunction usually need the longer option. These are complex issues that require more time for fuller recovery.
At Cognitive FX, we measure improvements by:
Not only does this allow us to compare your progress from the beginning to the end of treatment, it also informs our recommendations for your care going forward. Treatment at our clinic is only the beginning; recovery continues at home.
At the end of treatment, you will meet with one of our therapists to go over your results and receive a series of exercises to do at home. This homework typically includes physical exercises, cognitive activities, visual and vestibular exercises, and relaxation techniques and is designed to continue improvements in your brain after treatment. It usually takes an hour or less five times a week and can be reduced as your symptoms improve. If we feel that the patient may benefit from further therapy, we also offer referrals to suitable specialists.
.png?width=680&height=453&name=long-haul-covid-treatment-protocol%20(13).png)
We have a world-renowned, multidisciplinary team focused on patients suffering from conditions that affect brain function. In addition to COVID long-haulers, we also treat patients experiencing long-term symptoms after a concussion (a condition known as post concussion syndrome, or PCS), as well as patients who suffered a transient ischemic attack, carbon monoxide poisoning, encephalitis from infectious diseases, and others.
Our team includes clinical neuropsychologists, neuroscientists, a neuroradiologist, a neurosurgeon, psychologists, cognitive therapists, occupational therapists, physical therapists, a neurointegration specialist, MRI technicians, and many more. We are actively engaged in medical research and publish our results in scientific journals and other publications.
Our team treats hundreds of patients every year at our clinic in Provo, Utah. Patients visit us from across the U.S., Canada, Europe, and other parts of the world.
Our COVID patients often experience significant improvements in emotional symptoms like sadness and irritability, while symptoms like vision problems and fatigue may take a little longer and potentially need further therapy. However, even in these more “stubborn” symptoms, many of our patients say that they’re easier to cope with in their daily lives. Here’s a percent symptom improvement measured in a cohort of 43 patients at the end of one week of treatment at our clinic: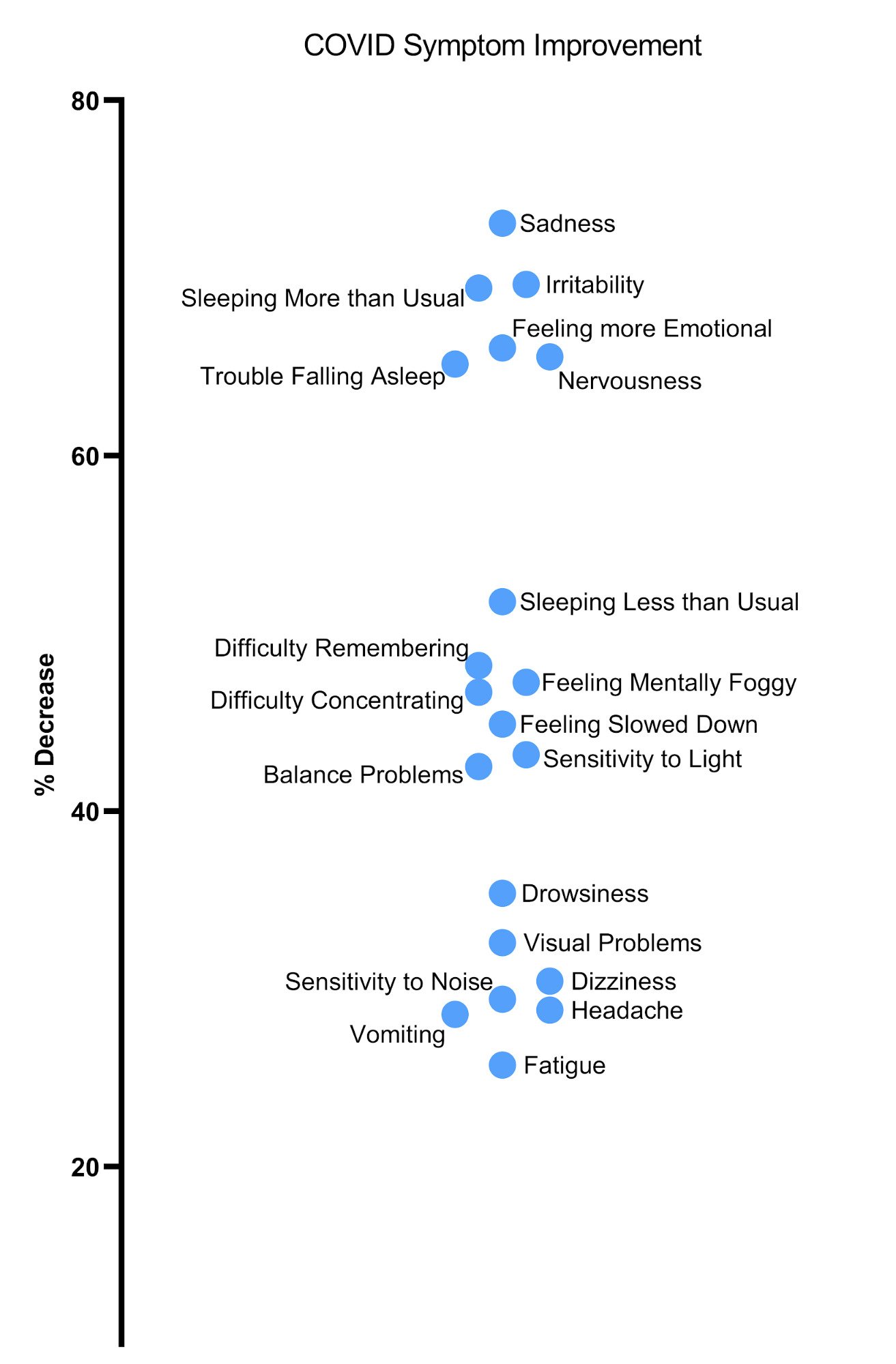
Fatigue and headache symptoms improve as patients go home to rest after a very intense treatment period. Visual problems typically require ongoing vision therapy (three to six months on average) for full improvement.
Want to determine if you’re eligible for treatment at our clinic? Request a consultation with our team.

Dealing with long COVID symptoms is physically and mentally challenging. Below are a few suggestions to deal with some of the most common symptoms. In addition, our blog offers many resources you may find helpful during your recovery from long COVID:
Fatigue
After getting COVID-19, patients often find they have less energy and feel more tired than they did before. With long COVID, even simple everyday tasks become exhausting.
Tips to help you cope with fatigue:
Further reading: Fatigue after COVID
Migraines and Headaches
Migraines and headaches are common in long COVID patients. The best way to cope with these symptoms is to identify what triggers your headaches and develop strategies to help reduce how often and how badly you get them.
Tips to cope with migraines and headaches:
Further reading: Long COVID headache treatments
Brain Fog, Memory Problems, and Other Cognitive Problems
Many long COVID patients complain of brain fog, memory problems, and other cognitive issues, such as difficulty concentrating or struggling to follow conversations. These symptoms often become worse with fatigue.
Tips to cope with cognitive impairments:
Further reading:
Sleep Disturbances
.jpg?width=2000&height=1118&name=long-haul-covid-treatment-protocol%20(2).jpg)
Sleep problems are one of the most common symptoms of long COVID. This includes, for example, insomnia, waking up feeling tired, difficulties falling asleep, or waking up frequently during the night.
Tips to cope with sleep problems:
Depression and Anxiety
Changes in mental health — such as stress, anxiety, depression, and feeling overwhelmed — are common in patients experiencing long COVID. Being unwell and potentially unable to work can be very stressful, especially when symptoms don’t seem to improve.
Tips to support your mental health:
Exercise Intolerance
Many COVID long-haulers struggle with any kind of physical activity. This is known as post-exertional malaise (PEM). Typically, symptoms can start at any time during exercise or up to 72 hours after activity and can last for days or weeks.
Avoid the trap of doing as much as you can when you feel fine because this will lead to a prolonged period of forced rest with increased symptoms.
Tips to cope with post exercise malaise:
Changes in Smell and Taste
The most well known symptom during the acute phase of this disease is loss of smell and taste. Most recover within two or three weeks, but about 5% of patients experience a loss of smell or taste that continues for months. Some patients also experience unusual smells, or they complain certain foods taste different.
Tips to help cope with the loss of smell and taste:
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.
By Mark Allen, Director of Research
The Enhanced Performance in Cognition - EPIC concussion treatment provided at Cognitive FX is a highly effective approach to concussion rehabilitation. We have...

The University of Pittsburgh Medical Center (UPMC) is a world-renowned healthcare provider and insurer with groundbreaking work in research, treatments, and clinical care. UPMC runs 40 hospitals and...

Concussions can have long-term physical, cognitive, and emotional effects. Symptoms such as brain fog, headaches, and depression can last for months or years after the initial injury. When the...

If you're suffering from persistent symptoms after a concussion — a condition calledpost-concussion syndrome (PCS)— you might think that Stanford Healthcare (part of Stanford University) would be a...

From a small outpatient clinic in the 1920s, Cleveland Clinic has grown to become one of the world’s largest integrated medical systems. With over 65,000 providers worldwide, Cleveland Clinic has...

If you have post-concussion syndrome, you might think that the Mayo Clinic would be a serious contender as your treatment provider. After all, the Mayo Clinic is a world-renowned medical and research...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY